Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
- sangramento retal
- diarreia
- sangue nas fezes
Outros fatores diagnósticos
- dor abdominal
- artrite e espondilite
- desnutrição
- desconforto abdominal
- febre
- perda de peso
- constipação
- erupção cutânea
- uveíte e episclerite
- palidez
Fatores de risco
- história familiar de doença inflamatória intestinal
- antígeno leucocitário humano-B27
- infecção
- uso de anti-inflamatórios não esteroidais (AINEs)
- não fumante ou ex-fumante
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- estudos das fezes para patógenos infecciosos
- calprotectina fecal (CF)
- Hemograma completo
- perfil metabólico completo (incluindo testes da função hepática)
- velocidade de hemossedimentação (VHS)
- proteína C-reativa
- radiografia abdominal simples
- sigmoidoscopia flexível
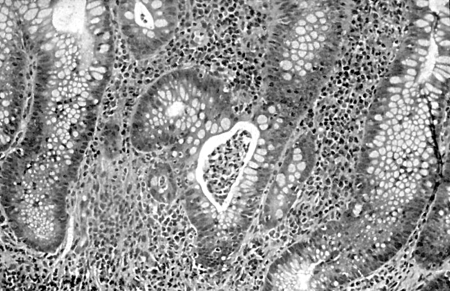
- colonoscopia
- biópsias
Investigações a serem consideradas
- Tomografia computadorizada (TC)
- ultrassonografia intestinal
Algoritmo de tratamento
Colaboradores
Autores
Andrew Poullis, BSc, MBBS, MD, FRCP
Consultant Gastroenterologist
Department of Gastroenterology
St George’s Hospital
London
UK
Declarações
AP is an author of a reference cited in this topic.
Sailish Honap,
Consultant Gastroenterologist
Department of Gastroenterology
St George’s Hospital
London
UK
Declarações
SH has received honoraria from Pfizer (speaker, consultant, advisory board member, and received travel grants), Janssen (speaker fees, travel grants), AbbVie (speaker fees, consultant, travel grants), Takeda (speaker fees), Ferring (travel grants), Pharmacosmos (travel grants), Galapagos (travel grants).
Kamal Patel,
Declarações
all disclosures
Aaron Bhakta, BMedSci (Hons), BMBS, MSc, MRCP
Clinical Fellow in Gastroenterology
Department of Gastroenterology
St George’s Hospital
London
UK
Declarações
AB declares that he has no competing interests.
Agradecimentos
Dr Hesam A. Nooredinvand, and Dr Andrew Poullis would like to gratefully acknowledge Dr Ben Shandro, Dr Anet Soubieres, Dr Rhys Hewett, Dr Willem J.S. de Villiers, and Dr Houssam Mardini, previous contributors to this topic.
Declarações
BS, AS, RH, WJSD, and HM declare that they have no competing interests.
Revisores
Stephen B Hanauer, MD
Professor of Medicine
Gastroenterology and Hepatology
Northwestern University
Evanston
IL
Declarações
SW declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
World Gastroenterology Organisation. Global guidelines: inflammatory bowel disease. Aug 2015 [internet publication].Texto completo
Rubin DT, Ananthakrishnan AN, Siegel CA, et al. ACG clinical guideline update: ulcerative colitis in adults. Am J Gastroenterol. 2025 Jun 3;120(6):1187-224.Texto completo Resumo
Moran GW, Gordon M, Sinopolou V, et al. British Society of Gastroenterology guidelines on inflammatory bowel disease in adults: 2025. Gut. 2025 Jun 23;74(Suppl 2):s1-101.Texto completo Resumo
Singh S, Loftus EV Jr, Limketkai BN, et al. AGA living clinical practice guideline on pharmacological management of moderate-to-severe ulcerative colitis. Gastroenterology. 2024 Dec;167(7):1307-43.Texto completo Resumo
Harbord M, Eliakim R, Bettenworth D, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: current management. J Crohns Colitis. 2017 Jul 1;11(7):769-84.Texto completo Resumo
National Institute for Health and Care Excellence (UK). Ulcerative colitis: management. May 2019 [internet publication].Texto completo
National Institute for Health and Care Excellence. Colorectal cancer prevention: colonoscopic surveillance in adults with ulcerative colitis, Crohn's disease or adenomas. Sep 2022 [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível aqui.
O uso deste conteúdo está sujeito ao nosso aviso legal