Os principais objetivos do tratamento são limitar o dano miocárdico por meio da restauração do fluxo sanguíneo o mais rapidamente possível e diminuir o remodelamento subsequente, o qual tem efeitos deletérios sobre a função ventricular e o prognóstico.[88]Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165.
https://academic.oup.com/eurheartj/article/40/2/87/5079120
http://www.ncbi.nlm.nih.gov/pubmed/30165437?tool=bestpractice.com
A revascularização imediata e rápida com intervenção coronária percutânea (ICP) em até 90 minutos após a primeira manifestação dos sintomas ou a trombólise em até 12 horas após o início dos sintomas pode prevenir ou minimizar o dano ao miocárdio e diminuir a morbidade e mortalidade ao prevenir complicações agudas.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[106]Redfors B, Mohebi R, Giustino G, et al. Time delay, infarct size, and microvascular obstruction after primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2021 Feb;14(2):e009879.
https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.120.009879
http://www.ncbi.nlm.nih.gov/pubmed/33440999?tool=bestpractice.com
É altamente recomendável que as comunidades locais ou áreas regionais desenvolvam um sistema de resposta rápida para o tratamento do IAMCSST. A estratégia ideal de revascularização coronária pode não ser clara para todos os pacientes com IAMCSST (por exemplo, se houver doença coronariana complexa e/ou condições comórbidas); é mais provável que isso se aplique aos pacientes mais idosos.[107]Damluji AA, Forman DE, Wang TY, et al. Management of acute coronary syndrome in the older adult population: a scientific statement from the American Heart Association. Circulation. 2023 Jan 17;147(3):e32-62.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10312228
http://www.ncbi.nlm.nih.gov/pubmed/36503287?tool=bestpractice.com
As diretrizes do American College of Cardiology/American Heart Association recomendam um processo de tomada de decisão compartilhada, centrado nesses pacientes, que utilize uma equipe multidisciplinar que inclua representantes da cardiologia intervencionista, cirurgia cardíaca e cardiologia clínica.[75]Gulati M, Levy PD, Mukherjee D, et al; Writing Committee Members. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.
https://www.jacc.org/doi/10.1016/j.jacc.2021.07.053
http://www.ncbi.nlm.nih.gov/pubmed/34756653?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[107]Damluji AA, Forman DE, Wang TY, et al. Management of acute coronary syndrome in the older adult population: a scientific statement from the American Heart Association. Circulation. 2023 Jan 17;147(3):e32-62.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10312228
http://www.ncbi.nlm.nih.gov/pubmed/36503287?tool=bestpractice.com
Manejo inicial
O paciente deve ser internado em uma unidade com monitoramento cardíaco contínuo e iniciar repouso rigoroso no leito nas primeiras 12 a 24 horas. Oxigênio suplementar pode ser administrado se a saturação de oxigênio estiver inferior a 90%.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
O uso liberal do oxigênio está associado a maior mortalidade nos pacientes com síndrome coronariana aguda.[108]Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018 Apr 28;391(10131):1693-705.
http://www.ncbi.nlm.nih.gov/pubmed/29726345?tool=bestpractice.com
[109]Siemieniuk RAC, Chu DK, Kim LH, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ. 2018 Oct 24;363:k4169. As diretrizes recomendam que o oxigênio não seja administrado como procedimento de rotina nos pacientes normóxicos com síndrome coronariana aguda (SCA) suspeitada ou confirmada.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
Administra-se aspirina imediatamente.
Uma analgesia adequada com morfina pode ser usada para aliviar a dor resistente a outros medicamentos anti-isquêmicos em tolerância máxima e reduzir a atividade simpática relacionada, o que pode aumentar ainda mais a demanda por oxigênio do miocárdio. Entretanto, a morfina pode retardar os efeitos da terapia com P2Y12 oral.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
A nitroglicerina também deve ser administrada imediatamente, se o paciente não estiver hipotenso, já que reduz a demanda de oxigênio pelo miocárdio e atenua a isquemia, e pode raramente abortar o IAM se houver espasmo coronariano. Entretanto, não deve ser administrada em doses que interfiram na terapia analgésica. A dosagem sublingual deve ser administrada primeiro a todos os pacientes, enquanto a terapia intravenosa é reservada aos pacientes com hipertensão ou com insuficiência cardíaca.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
Pacientes hemodinamicamente instáveis
O choque cardiogênico ocorre em 5% a 10% das pessoas que se apresentam com um IAMCSST, e a mortalidade intra-hospitalar é ≥50%.[90]Zeymer U, Bueno H, Granger CB, et al. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(2):183-97.
https://academic.oup.com/ehjacc/article/9/2/183/5933392
http://www.ncbi.nlm.nih.gov/pubmed/32114774?tool=bestpractice.com
[91]Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 2021 Nov 9;326(18):1840-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661446
http://www.ncbi.nlm.nih.gov/pubmed/34751704?tool=bestpractice.com
Se a revascularização com ICP falhar ou não for viável, recomenda-se uma cirurgia de revascularização miocárdica (CRM) urgente para os pacientes com choque cardiogênico ou instabilidade hemodinâmica.[90]Zeymer U, Bueno H, Granger CB, et al. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(2):183-97.
https://academic.oup.com/ehjacc/article/9/2/183/5933392
http://www.ncbi.nlm.nih.gov/pubmed/32114774?tool=bestpractice.com
[91]Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 2021 Nov 9;326(18):1840-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661446
http://www.ncbi.nlm.nih.gov/pubmed/34751704?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Os pacientes com estados de baixo débito cardíaco e choque cardiogênico podem se beneficiar de uma infusão de dobutamina.[90]Zeymer U, Bueno H, Granger CB, et al. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(2):183-97.
https://academic.oup.com/ehjacc/article/9/2/183/5933392
http://www.ncbi.nlm.nih.gov/pubmed/32114774?tool=bestpractice.com
[91]Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 2021 Nov 9;326(18):1840-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661446
http://www.ncbi.nlm.nih.gov/pubmed/34751704?tool=bestpractice.com
As diretrizes afirmam que o uso adjuvante de uma bomba de balão intra-aórtico (BBIA) ou de um dispositivo de suporte circulatório mecânico ventricular pode ser considerado em determinados pacientes com risco de comprometimento hemodinâmico durante a ICP (por exemplo, nos pacientes com doença arterial periférica ou aórtica grave).[90]Zeymer U, Bueno H, Granger CB, et al. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(2):183-97.
https://academic.oup.com/ehjacc/article/9/2/183/5933392
http://www.ncbi.nlm.nih.gov/pubmed/32114774?tool=bestpractice.com
[91]Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 2021 Nov 9;326(18):1840-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661446
http://www.ncbi.nlm.nih.gov/pubmed/34751704?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Os resultados de estudos observacionais parecem ser conflitantes para a BBIA no IAM e, em ensaios clínicos randomizados e controlados (ECRC), não foi demonstrada redução da mortalidade após um IAM, mesmo em pacientes com choque cardiogênico.[110]Ahmad Y, Sen S, Shun-Shin MJ, et al. Intra-aortic balloon pump therapy for acute myocardial infarction: a meta-analysis. JAMA Intern Med. 2015 Jun;175(6):931-9.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2210888
http://www.ncbi.nlm.nih.gov/pubmed/25822657?tool=bestpractice.com
[  ]
In people with myocardial infarction complicated by cardiogenic shock, what are the effects of intra-aortic balloon pump counterpulsation (IABP)?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1071/fullMostre-me a resposta
]
In people with myocardial infarction complicated by cardiogenic shock, what are the effects of intra-aortic balloon pump counterpulsation (IABP)?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1071/fullMostre-me a resposta
Terapias antiagregante plaquetária e anticoagulante
A aspirina deve ser administrada a todos os pacientes, juntamente com ticagrelor ou prasugrel.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[111]Montalescot G, Wiviott SD, Braunwald E, et al. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet. 2009 Feb 28;373(9665):723-31.
http://www.ncbi.nlm.nih.gov/pubmed/19249633?tool=bestpractice.com
O prasugrel e o ticagrelor estão associados a reduções nos eventos isquêmicos em comparação com o clopidogrel, embora também haja um maior risco de sangramento com esses agentes.[112]Navarese EP, Khan SU, Kołodziejczak M, et al. Comparative efficacy and safety of oral P2Y(12) inhibitors in acute coronary syndrome: network meta-analysis of 52816 patients from 12 randomized rials. Circulation. 2020 Jul 14;142(2):150-60.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489363
http://www.ncbi.nlm.nih.gov/pubmed/32468837?tool=bestpractice.com
[113]Turgeon RD, Koshman SL, Youngson E, et al. Association of ticagrelor vs clopidogrel with major adverse coronary events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. JAMA Intern Med. 2020 Mar 1;180(3):420-8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6990835
http://www.ncbi.nlm.nih.gov/pubmed/31930361?tool=bestpractice.com
[114]Ruiz-Nodar JM, Esteve-Pastor MA, Rivera-Caravaca JM, et al. One-year efficacy and safety of prasugrel and ticagrelor in patients with acute coronary syndromes: Results from a prospective and multicentre achilles registry. Br J Clin Pharmacol. 2020 Jun;86(6):1052-61.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7256120
http://www.ncbi.nlm.nih.gov/pubmed/31912949?tool=bestpractice.com
O prasugrel é contraindicado nos pacientes com uma história de AVC isquêmico ou ataque isquêmico transitório, e seu uso não é recomendado em pacientes >75 anos de idade ou em pacientes com baixo peso corporal (<60 kg) devido ao maior risco de sangramento (embora reduções nas doses possam mitigar esse risco); portanto, o ticagrelor é usado com mais frequência.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[115]Goodwin MM, Desilets AR, Willett KC. Thienopyridines in acute coronary syndrome. Ann Pharmacother. 2011 Feb;45(2):207-17.
http://www.ncbi.nlm.nih.gov/pubmed/21304037?tool=bestpractice.com
[116]Menichelli M, Neumann FJ, Ndrepepa G, et al. Age- and weight-adapted dose of prasugrel versus standard dose of ticagrelor in patients with acute coronary syndromes : results from a randomized trial. Ann Intern Med. 2020 Sep 15;173(6):436-44.
http://www.ncbi.nlm.nih.gov/pubmed/32687741?tool=bestpractice.com
O ticagrelor pode estar associado a um maior risco de sangramento e morte que o clopidogrel em pacientes idosos.[117]Szummer K, Montez-Rath ME, Alfredsson J, et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome: insights from the SWEDEHEART registry. Circulation. 2020 Nov 3;142(18):1700-8.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050645
http://www.ncbi.nlm.nih.gov/pubmed/32867508?tool=bestpractice.com
O clopidogrel é um inibidor alternativo de P2Y12 que pode ser usado quando o ticagrelor e o prasugrel forem contraindicados ou não estiverem disponíveis.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[117]Szummer K, Montez-Rath ME, Alfredsson J, et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome: insights from the SWEDEHEART registry. Circulation. 2020 Nov 3;142(18):1700-8.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050645
http://www.ncbi.nlm.nih.gov/pubmed/32867508?tool=bestpractice.com
O cangrelor, um inibidor intravenoso de P2Y12, pode ser usado como adjuvante à ICP para reduzir os riscos de IAM periprocedimental, de repetição da revascularização coronária e de trombose no stent nos pacientes não tratados previamente com um inibidor de P2Y12 e que não estiverem em tratamento com um inibidor da glicoproteína IIb/IIIa.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[118]Steg PG, Bhatt DL, Hamm CW, et al. Effect of cangrelor on periprocedural outcomes in percutaneous coronary interventions: a pooled analysis of patient-level data. Lancet. 2013 Dec 14;382(9909):1981-92.
http://www.ncbi.nlm.nih.gov/pubmed/24011551?tool=bestpractice.com
A heparina não fracionada é o anticoagulante de preferência de uso como agente único, além da terapia antiplaquetária. De forma alternativa, a bivalirudina e a enoxaparina podem ser usadas.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
Inibidores adicionais da glicoproteína IIb/IIIa (inibidores GPIIb/IIIa) só são recomendados se houver evidência de fluxo lento, ausência de refluxo ou uma complicação trombótica na ICP.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Medidas de suporte
Analgesia adequada com morfina é essencial para aliviar a dor e a atividade simpática a ela relacionada, as quais podem aumentar a demanda de oxigênio pelo miocárdio.
O oxigênio suplementar pode ser administrado se a saturação de oxigênio for inferior a 90%.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
As diretrizes recomendam que o oxigênio não seja administrado como procedimento de rotina nos pacientes normóxicos com SCA suspeitada ou confirmada.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
O controle glicêmico, incluindo o uso de insulina quando apropriado, também deve ser mantido, embora um controle rígido não tenha demonstrado ser benéfico em pacientes em estado crítico. Uma meta glicêmica de 7.8-10.0 mmol/L (140-180 mg/dL) é recomendada para a maioria dos indivíduos em estado crítico (aqueles na UTI) com hiperglicemia. Metas glicêmicas mais rigorosas individualizadas podem ser apropriadas para indivíduos em estado crítico selecionados.[26]American Diabetes Association. Standards of care in diabetes - 2025. Diabetes Care. 2025 Jan 1;48(Suppl 1):S1-343.
https://diabetesjournals.org/care/issue/48/Supplement_1
Eletricamente instável: pós-parada cardíaca
Recomenda-se revascularização de emergência nos pacientes com parada cardíaca que tiverem sido ressuscitados, estiverem hemodinamicamente estáveis e cujo eletrocardiograma (ECG) mostre evidências de IAMCSST. A ICP em etapas de uma estenose significativa de artéria não infartada é recomendada após uma ICP primária bem-sucedida em determinados pacientes hemodinamicamente estáveis com doença multivascular.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Como opção, a ICP multivascular pode ser considerada no momento da ICP primária em determinados pacientes, embora as evidências em prol dessa estratégia sejam mais fracas.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
No entanto, os médicos devem considerar os dados clínicos, a gravidade/complexidade da lesão e o risco de nefropatia por contraste para determinar a estratégia de ICP ideal (primária ou em etapas).
A CRM de emergência é contraindicada em pacientes pós-parada cardíaca que estejam comatosos.
A trombólise é uma opção possível se a ICP não estiver imediatamente disponível, mas a ressuscitação cardiopulmonar (RCP) prolongada é uma contraindicação ao uso de trombolíticos.
Recomenda-se hipotermia para pacientes que sofreram parada cardíaca, foram ressuscitados e permanecem comatosos.
Hemodinamicamente estável: ICP disponível em até 90 minutos após o primeiro contato com o serviço médico
ICP
A ICP primária, com colocação de stent (usando stents metálicos ou farmacológicos), é o método de escolha para a revascularização, desde que possa ser realizada em tempo hábil com uma equipe experiente de cirurgiões. A ICP primária é recomendada para pacientes que se apresentam até 12 horas após o início dos sintomas e pode ser benéfica para pacientes que se apresentam entre 12 e 24 horas após o início dos sintomas, embora seja mais eficaz quando o tempo entre sintomas e balão é minimizado.[88]Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165.
https://academic.oup.com/eurheartj/article/40/2/87/5079120
http://www.ncbi.nlm.nih.gov/pubmed/30165437?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[106]Redfors B, Mohebi R, Giustino G, et al. Time delay, infarct size, and microvascular obstruction after primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2021 Feb;14(2):e009879.
https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.120.009879
http://www.ncbi.nlm.nih.gov/pubmed/33440999?tool=bestpractice.com
[119]De Luca G, Cassetti E, Marino P. Percutaneous coronary intervention-related time delay, patient's risk profile, and survival benefits of primary angioplasty vs lytic therapy in ST-segment elevation myocardial infarction. Am J Emerg Med. 2009 Jul;27(6):712-9.
http://www.ncbi.nlm.nih.gov/pubmed/19751630?tool=bestpractice.com
[120]Nielsen PH, Maeng M, Busk M, et al; DANAMI-2 Investigators. Primary angioplasty versus fibrinolysis in acute myocardial infarction: long-term follow-up in the Danish acute myocardial infarction 2 trial. Circulation. 2010 Apr 6;121(13):1484-91.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.109.873224
http://www.ncbi.nlm.nih.gov/pubmed/20308618?tool=bestpractice.com
Isso envolve a transferência imediata para o laboratório de cateterismo com a intenção de abrir a artéria com a colocação do stent. Dá-se preferência aos stents farmacológicos.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[121]Wallace EL, Abdel-Latif A, Charnigo R, et al. Meta-analysis of long-term outcomes for drug-eluting stents versus bare-metal stents in primary percutaneous coronary interventions for ST-segment elevation myocardial infarction. Am J Cardiol. 2012 Apr 1;109(7):932-40.
http://www.ncbi.nlm.nih.gov/pubmed/22221949?tool=bestpractice.com
[122]Brugaletta S, Gomez-Lara J, Ortega-Paz L, et al. 10-Year follow-up of patients with everolimus-eluting versus bare-metal stents after ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2021 Mar 9;77(9):1165-78.
https://www.sciencedirect.com/science/article/pii/S073510972100019X
http://www.ncbi.nlm.nih.gov/pubmed/33663733?tool=bestpractice.com
[  ]
How do drug-eluting stents compare with bare-metal stents for people with acute coronary syndrome?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1890/fullMostre-me a resposta Os stents farmacológicos de terceira geração compostos de polímeros biodegradáveis estão sendo pesquisados atualmente.[123]Raungaard B, Jensen LO, Tilsted HH, et al; Scandinavian Organization for Randomized Trials with Clinical Outcome (SORT OUT). Zotarolimus-eluting durable-polymer-coated stent versus a biolimus-eluting biodegradable-polymer-coated stent in unselected patients undergoing percutaneous coronary intervention (SORT OUT VI): a randomised non-inferiority trial. Lancet. 2015 Apr 18;385(9977):1527-35.
http://www.ncbi.nlm.nih.gov/pubmed/25601789?tool=bestpractice.com
[124]Sabaté M, Brugaletta S, Cequier A, et al. Clinical outcomes in patients with ST-segment elevation myocardial infarction treated with everolimus-eluting stents versus bare-metal stents (EXAMINATION): 5-year results of a randomised trial. Lancet. 2016 Jan 23;387(10016):357-66.
https://boris.unibe.ch/92887
http://www.ncbi.nlm.nih.gov/pubmed/26520230?tool=bestpractice.com
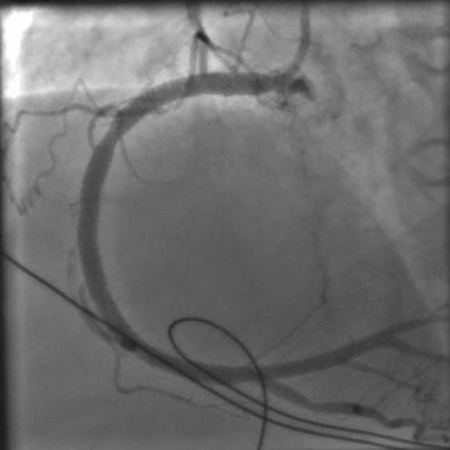
[Figure caption and citation for the preceding image starts]: Angiografia mostrando a artéria coronária direita obstruídaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
]
How do drug-eluting stents compare with bare-metal stents for people with acute coronary syndrome?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1890/fullMostre-me a resposta Os stents farmacológicos de terceira geração compostos de polímeros biodegradáveis estão sendo pesquisados atualmente.[123]Raungaard B, Jensen LO, Tilsted HH, et al; Scandinavian Organization for Randomized Trials with Clinical Outcome (SORT OUT). Zotarolimus-eluting durable-polymer-coated stent versus a biolimus-eluting biodegradable-polymer-coated stent in unselected patients undergoing percutaneous coronary intervention (SORT OUT VI): a randomised non-inferiority trial. Lancet. 2015 Apr 18;385(9977):1527-35.
http://www.ncbi.nlm.nih.gov/pubmed/25601789?tool=bestpractice.com
[124]Sabaté M, Brugaletta S, Cequier A, et al. Clinical outcomes in patients with ST-segment elevation myocardial infarction treated with everolimus-eluting stents versus bare-metal stents (EXAMINATION): 5-year results of a randomised trial. Lancet. 2016 Jan 23;387(10016):357-66.
https://boris.unibe.ch/92887
http://www.ncbi.nlm.nih.gov/pubmed/26520230?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Angiografia mostrando a artéria coronária direita obstruídaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].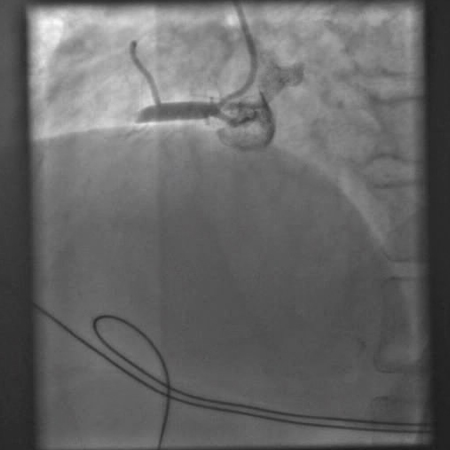 [Figure caption and citation for the preceding image starts]: Angiografia mostrando uma tentativa de abrir a artéria coronária direita obstruída com um balão de angioplastiaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Angiografia mostrando uma tentativa de abrir a artéria coronária direita obstruída com um balão de angioplastiaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends]. [Figure caption and citation for the preceding image starts]: Angiografia após a angioplastia com balão e colocação de stent mostrando uma artéria coronária direita abertaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Angiografia após a angioplastia com balão e colocação de stent mostrando uma artéria coronária direita abertaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].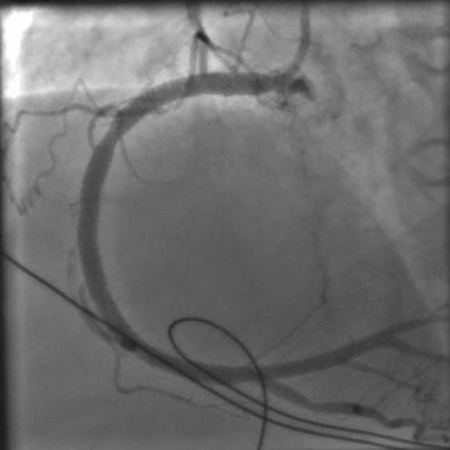
A abordagem radial é preferível à abordagem femoral, pois resulta em desfechos melhores (por exemplo, redução da mortalidade, de eventos cardiovasculares adversos significativos, sangramento importante e complicações decorrentes de sangramentos), principalmente se o cirurgião tiver experiência em acessos radiais.[88]Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165.
https://academic.oup.com/eurheartj/article/40/2/87/5079120
http://www.ncbi.nlm.nih.gov/pubmed/30165437?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[125]Andò G, Capodanno D. Radial versus femoral access in invasively managed patients with acute coronary syndrome: a systematic review and meta-analysis. Ann Intern Med. 2015 Dec 15;163(12):932-40.
http://www.ncbi.nlm.nih.gov/pubmed/26551857?tool=bestpractice.com
[126]Valgimigli M, Gagnor A, Calabró P, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. 2015 Jun 20;385(9986):2465-76.
http://www.ncbi.nlm.nih.gov/pubmed/25791214?tool=bestpractice.com
[127]Nardin M, Verdoia M, Barbieri L, et al. Radial vs femoral approach in acute coronary syndromes: a meta-analysis of randomized trials. Curr Vasc Pharmacol. 2017;16(1):79-92.
http://www.ncbi.nlm.nih.gov/pubmed/28490313?tool=bestpractice.com
A ICP em etapas de uma estenose significativa de artéria não infartada é recomendada após uma ICP primária bem-sucedida em determinados pacientes hemodinamicamente estáveis com IAMCSST e doença multivascular.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Como opção, a ICP multivascular pode ser considerada no momento da ICP primária em determinados pacientes, embora as evidências em prol dessa estratégia sejam mais fracas.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[128]Engstrøm T, Kelbæk H, Helqvist S, et al; DANAMI-3-PRIMULTI Investigators. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3-PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015 Aug 15;386(9994):665-71.
http://www.ncbi.nlm.nih.gov/pubmed/26347918?tool=bestpractice.com
[129]Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015 Mar 17;65(10):963-72.
https://www.jacc.org/doi/10.1016/j.jacc.2014.12.038
http://www.ncbi.nlm.nih.gov/pubmed/25766941?tool=bestpractice.com
[130]Kowalewski M, Schulze V, Berti S, et al. Complete revascularisation in ST-elevation myocardial infarction and multivessel disease: meta-analysis of randomised controlled trials. Heart. 2015 Aug;101(16):1309-17.
http://www.ncbi.nlm.nih.gov/pubmed/26037102?tool=bestpractice.com
Os médicos devem considerar fatores como dados clínicos, estabilidade hemodinâmica, gravidade/complexidade da lesão e risco de nefropatia por contraste para determinar a estratégia de ICP ideal. O cálculo do escore SYNTAX é recomendado para a ICP multivascular ou no tronco coronário esquerdo.
SYNTAX score
Opens in new window
As diretrizes também não recomendam trombectomia por aspiração manual de rotina antes da ICP primária, pois as evidências não sugerem nenhum benefício desse procedimento em relação à ICP isolada.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[131]Bhindi R, Kajander OA, Jolly SS, et al. Culprit lesion thrombus burden after manual thrombectomy or percutaneous coronary intervention-alone in ST-segment elevation myocardial infarction: the optical coherence tomography sub-study of the TOTAL (ThrOmbecTomy versus PCI ALone) trial. Eur Heart J. 2015 Aug 1;36(29):1892-900.
https://academic.oup.com/eurheartj/article/36/29/1892/2465937
http://www.ncbi.nlm.nih.gov/pubmed/25994742?tool=bestpractice.com
Além do mais, estudos sugeriram que a trombectomia por aspiração de rotina pode aumentar o risco de acidente vascular cerebral (AVC).[132]Jolly SS, Cairns JA, Yusuf S, et al; TOTAL Investigators. Stroke in the TOTAL trial: a randomized trial of routine thrombectomy vs. percutaneous coronary intervention alone in ST elevation myocardial infarction. Eur Heart J. 2015 Sep 14;36(35):2364-72.
https://academic.oup.com/eurheartj/article/36/35/2364/2466054
http://www.ncbi.nlm.nih.gov/pubmed/26129947?tool=bestpractice.com
[133]Jolly SS, Cairns JA, Yusuf S, et al; TOTAL Investigators. Outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised TOTAL trial. Lancet. 2016 Jan 9;387(10014):127-35.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5007127
http://www.ncbi.nlm.nih.gov/pubmed/26474811?tool=bestpractice.com
Muitos hospitais têm capacidade para ICP por 24 horas; no entanto, em instalações sem laboratórios de cateterismo, deve-se considerar a transferência de rotina para uma instalação capacitada para ICP para todos os pacientes se o tempo de transferência for razoável e o tempo isquêmico total após a apresentação for inferior a 120 minutos.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
CRM
A revascularização de emergência com CRM pode ser útil se a ICP falhar ou não for viável e uma grande área do miocárdio estiver em risco.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
A CRM é recomendada para os pacientes com choque cardiogênico ou insuficiência cardíaca se a ICP não for viável.[90]Zeymer U, Bueno H, Granger CB, et al. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(2):183-97.
https://academic.oup.com/ehjacc/article/9/2/183/5933392
http://www.ncbi.nlm.nih.gov/pubmed/32114774?tool=bestpractice.com
[91]Samsky MD, Morrow DA, Proudfoot AG, et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 2021 Nov 9;326(18):1840-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661446
http://www.ncbi.nlm.nih.gov/pubmed/34751704?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
A CRM não deve ser realizada após o insucesso de uma ICP primária na ausência de isquemia ou de uma grande área de miocárdio em risco, ou se a revascularização cirúrgica não for viável em decorrência de um estado de não reperfusão ou de alvos distais desfavoráveis.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Terapias antiagregante plaquetária e anticoagulante
A aspirina deve ser administrada a todos os pacientes, juntamente com ticagrelor ou prasugrel.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[111]Montalescot G, Wiviott SD, Braunwald E, et al. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet. 2009 Feb 28;373(9665):723-31.
http://www.ncbi.nlm.nih.gov/pubmed/19249633?tool=bestpractice.com
O prasugrel e o ticagrelor estão associados a reduções nos eventos isquêmicos em comparação com o clopidogrel, embora também haja um aumento do risco de sangramento com esses agentes.[112]Navarese EP, Khan SU, Kołodziejczak M, et al. Comparative efficacy and safety of oral P2Y(12) inhibitors in acute coronary syndrome: network meta-analysis of 52816 patients from 12 randomized rials. Circulation. 2020 Jul 14;142(2):150-60.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489363
http://www.ncbi.nlm.nih.gov/pubmed/32468837?tool=bestpractice.com
[113]Turgeon RD, Koshman SL, Youngson E, et al. Association of ticagrelor vs clopidogrel with major adverse coronary events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. JAMA Intern Med. 2020 Mar 1;180(3):420-8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6990835
http://www.ncbi.nlm.nih.gov/pubmed/31930361?tool=bestpractice.com
[114]Ruiz-Nodar JM, Esteve-Pastor MA, Rivera-Caravaca JM, et al. One-year efficacy and safety of prasugrel and ticagrelor in patients with acute coronary syndromes: Results from a prospective and multicentre achilles registry. Br J Clin Pharmacol. 2020 Jun;86(6):1052-61.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7256120
http://www.ncbi.nlm.nih.gov/pubmed/31912949?tool=bestpractice.com
O prasugrel é contraindicado nos pacientes com uma história de AVC isquêmico ou ataque isquêmico transitório, e seu uso não é recomendado em pacientes >75 anos de idade ou em pacientes com baixo peso corporal (<60 kg) devido ao maior risco de sangramento (embora reduções nas doses possam mitigar esse risco); portanto, o ticagrelor é usado com mais frequência.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[115]Goodwin MM, Desilets AR, Willett KC. Thienopyridines in acute coronary syndrome. Ann Pharmacother. 2011 Feb;45(2):207-17.
http://www.ncbi.nlm.nih.gov/pubmed/21304037?tool=bestpractice.com
[116]Menichelli M, Neumann FJ, Ndrepepa G, et al. Age- and weight-adapted dose of prasugrel versus standard dose of ticagrelor in patients with acute coronary syndromes : results from a randomized trial. Ann Intern Med. 2020 Sep 15;173(6):436-44.
http://www.ncbi.nlm.nih.gov/pubmed/32687741?tool=bestpractice.com
O ticagrelor pode estar associado a maiores riscos de sangramento e morte que o clopidogrel nos pacientes idosos.[117]Szummer K, Montez-Rath ME, Alfredsson J, et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome: insights from the SWEDEHEART registry. Circulation. 2020 Nov 3;142(18):1700-8.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050645
http://www.ncbi.nlm.nih.gov/pubmed/32867508?tool=bestpractice.com
O clopidogrel é um inibidor alternativo de P2Y12 que pode ser usado quando o ticagrelor e o prasugrel forem contraindicados ou não estiverem disponíveis.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[117]Szummer K, Montez-Rath ME, Alfredsson J, et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome: insights from the SWEDEHEART registry. Circulation. 2020 Nov 3;142(18):1700-8.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050645
http://www.ncbi.nlm.nih.gov/pubmed/32867508?tool=bestpractice.com
O cangrelor, um inibidor intravenoso do P2Y12, pode ser usado como adjuvante à ICP para reduzir o risco de IAM periprocedimental, repetição da revascularização coronária e trombose em stents nos em pacientes não previamente tratados com um inibidor do P2Y12 e que não estejam em tratamento com um inibidor da GPIIb/IIIa.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[118]Steg PG, Bhatt DL, Hamm CW, et al. Effect of cangrelor on periprocedural outcomes in percutaneous coronary interventions: a pooled analysis of patient-level data. Lancet. 2013 Dec 14;382(9909):1981-92.
http://www.ncbi.nlm.nih.gov/pubmed/24011551?tool=bestpractice.com
A heparina não fracionada é o anticoagulante de escolha para uso como agente único, além da terapia antiagregante plaquetária. Como opção, a bivalirudina e a enoxaparina podem ser usadas. Inibidores adicionais da glicoproteína IIb/IIIa (inibidores GPIIb/IIIa) só são recomendados se houver evidência de fluxo lento, ausência de fluxo, ou uma complicação trombótica na ICP.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Medidas de suporte
A administração de betabloqueadores orais deve ser iniciada o quanto antes, pois eles diminuem a extensão do infarto e reduzem a mortalidade, embora seja necessário ter cautela nos pacientes com evidências de insuficiência cardíaca, hipotensão, bradicardia ou asma.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[134]Bangalore S, Makani H, Radford M, et al. Clinical outcomes with β-blockers for myocardial infarction: a meta-analysis of randomized trials. Am J Med. 2014 Oct;127(10):939-53.
https://www.amjmed.com/article/S0002-9343(14)00470-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24927909?tool=bestpractice.com
[135]Peck KY, Andrianopoulos N, Dinh D, et al. Role of beta blockers following percutaneous coronary intervention for acute coronary syndrome. Heart. 2021 May;107(9):728-33.
http://www.ncbi.nlm.nih.gov/pubmed/32887736?tool=bestpractice.com
Os betabloqueadores intravenosos são recomendados apenas nos pacientes hipertensos ou com isquemia continuada, desde que não haja contraindicações ao seu uso.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[136]Pizarro G, Fernández-Friera L, Fuster V, et al. Long-term benefit of early pre-reperfusion metoprolol administration in patients with acute myocardial infarction: results from the METOCARD-CNIC trial (Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction). J Am Coll Cardiol. 2014 Jun 10;63(22):2356-62.
https://www.jacc.org/doi/10.1016/j.jacc.2014.03.014
http://www.ncbi.nlm.nih.gov/pubmed/24694530?tool=bestpractice.com
Na ausência de contraindicações, uma terapia com estatinas de alta intensidade (ou seja, esquemas com estatinas que reduzam o colesterol LDL em ≥50%) deve ser iniciada ou continuada em todos os pacientes com IAMCSST estabilizados.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[137]Schubert J, Lindahl B, Melhus H, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J. 2021 Jan 20;42(3):243-52.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7954251
http://www.ncbi.nlm.nih.gov/pubmed/33367526?tool=bestpractice.com
Nos pacientes de alto risco com SCA (FEVE <40%, hipertensão, diabetes mellitus ou IAMCSST em localização anterior) e na ausência de contraindicações, um inibidor da ECA (IECA) oral ou um bloqueador do receptor da angiotensina (BRA) deve ser iniciado nos pacientes com IAM apropriados.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
Nos pacientes com IAM com FEVE ≤40% e com sintomas de insuficiência cardíaca e/ou diabetes mellitus, a adição de um antagonista do receptor mineralocorticoide (por exemplo, eplerenona) deve ser administrada na ausência de doença renal crônica avançada, hipercalemia ou outra contraindicação. A eplerenona pode ser adicionada para otimizar a terapia medicamentosa nos pacientes elegíveis (creatinina <221 micromoles/L [<2.5 mg/dL] nos homens e <177 micromoles/L [<2.0 mg/dL] nas mulheres; potássio <5.0 mmol/L [<5.0 mEq/L]) de 3 a 14 dias após o IAMCSST com uma fração de ejeção <0.40 e insuficiência cardíaca sintomática ou diabetes mellitus.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[138]Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003 Apr 3;348(14):1309-21.
https://www.nejm.org/doi/10.1056/NEJMoa030207
http://www.ncbi.nlm.nih.gov/pubmed/12668699?tool=bestpractice.com
Demonstrou-se que um início mais rápido do medicamento (<7 dias) reduz significativamente as taxas de mortalidade por todas as causas, morte súbita cardíaca e hospitalização/mortalidade cardiovascular, enquanto o início >7 dias não mostrou efeito significativo sobre os desfechos.[139]Montalescot G, Pitt B, Lopez de Sa E, et al; REMINDER Investigators. Early eplerenone treatment in patients with acute ST-elevation myocardial infarction without heart failure: the Randomized Double-Blind Reminder Study. Eur Heart J. 2014 Sep 7;35(34):2295-302.
https://academic.oup.com/eurheartj/article/35/34/2295/2481156
http://www.ncbi.nlm.nih.gov/pubmed/24780614?tool=bestpractice.com
O oxigênio suplementar pode ser administrado se a saturação de oxigênio for inferior a 90%.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
As diretrizes recomendam que o oxigênio não deve ser administrado como procedimento de rotina nos pacientes normóxicos com SCA suspeitada ou confirmada.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[80]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
O controle glicêmico, incluindo o uso de insulina quando apropriado, também deve ser mantido, embora um controle rígido não tenha demonstrado ser benéfico em pacientes em estado crítico. Uma meta glicêmica de 5.6-10.0 mmol/L (100-180 mg/dL) é recomendada para os indivíduos que não estiverem em estado crítico (aqueles que não estiverem na UTI).[26]American Diabetes Association. Standards of care in diabetes - 2025. Diabetes Care. 2025 Jan 1;48(Suppl 1):S1-343.
https://diabetesjournals.org/care/issue/48/Supplement_1
Anti-inflamatórios não esteroidais devem ser evitados e, se possível, interrompidos em pacientes que já os utilizam.[140]Gibson CM, Pride YB, Aylward PE, et al. Association of non-steroidal anti-inflammatory drugs with outcomes in patients with ST-segment elevation myocardial infarction treated with fibrinolytic therapy: an ExTRACT-TIMI 25 analysis. J Thromb Thrombolysis. 2009 Jan;27(1):11-7.
http://www.ncbi.nlm.nih.gov/pubmed/18695943?tool=bestpractice.com
Hemodinamicamente estável: ICP disponível >90 minutos após o primeiro contato com o serviço médico e até 12 horas após o início dos sintomas sem contraindicações para trombólise
A trombólise é indicada se a ICP não estiver disponível em até 90 minutos após o primeiro contato do paciente com o serviço médico e se o paciente não apresentar nenhuma contraindicação para a terapia trombolítica.[141]Armstrong PW, Gershlick AH, Goldstein P, et al. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013 Apr 11;368(15):1379-87.
https://www.doi.org/10.1056/NEJMoa1301092
http://www.ncbi.nlm.nih.gov/pubmed/23473396?tool=bestpractice.com
[142]Jamal J, Idris H, Faour A, et al. Late outcomes of ST-elevation myocardial infarction treated by pharmaco-invasive or primary percutaneous coronary intervention. Eur Heart J. 2023 Feb 7;44(6):516-28.
https://academic.oup.com/eurheartj/article/44/6/516/6865195
http://www.ncbi.nlm.nih.gov/pubmed/36459120?tool=bestpractice.com
Ela deve ser iniciada em até 30 minutos após a manifestação. A trombólise é usada apenas uma vez após o diagnóstico inicial, e deve ser feita em até 12 horas após o início dos sintomas (idealmente em até 3 horas), já que a eficácia dos agentes fibrinolíticos na lise do trombo diminui ao longo do tempo. O tratamento dentro das primeiras 2 horas (particularmente na primeira hora) pode abortar o IAM e reduzir drasticamente a mortalidade.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[143]Manfredini R, Boari B. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty. Circulation. 2004 May 11;109(18):e219.
https://www.ahajournals.org/doi/10.1161/01.CIR.0000127696.00202.67
As contraindicações absolutas para trombólise são qualquer hemorragia intracraniana prévia, lesão intracraniana maligna ou lesão vascular cerebral estrutural (por exemplo, malformações arteriovenosas) conhecidas, AVC isquêmico nos últimos 3 meses, suspeita de dissecção da aorta, sangramento ativo ou diátese hemorrágica, traumatismo craniano ou facial fechado significativo nos últimos 3 meses, cirurgia intracraniana ou intraespinhal nos últimos 2 meses ou hipertensão grave não controlada (sem resposta clínica à terapia).[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
Trombolíticos podem estar associados a um aumento do risco de sangramento, além do risco associado a outros agentes antitrombóticos e/ou antiplaquetários, e também podem provocar hemorragia intracraniana.
A transferência em até 24 horas para um hospital no qual se possa realizar uma ICP deve ser considerada em todos os pacientes submetidos a terapia fibrinolítica. A angiografia com intenção de revascularizar completamente o vaso afetado deve ser considerada dentro de 24 horas, mesmo após o sucesso da terapia fibrinolítica (isto é, tratamento da estenose residual ou do fluxo deficitário da artéria infartada).[88]Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165.
https://academic.oup.com/eurheartj/article/40/2/87/5079120
http://www.ncbi.nlm.nih.gov/pubmed/30165437?tool=bestpractice.com
[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[142]Jamal J, Idris H, Faour A, et al. Late outcomes of ST-elevation myocardial infarction treated by pharmaco-invasive or primary percutaneous coronary intervention. Eur Heart J. 2023 Feb 7;44(6):516-28.
https://academic.oup.com/eurheartj/article/44/6/516/6865195
http://www.ncbi.nlm.nih.gov/pubmed/36459120?tool=bestpractice.com
Uma ICP de resgate após a trombólise é recomendada para os pacientes com evidências de insucesso na reperfusão (tais como dor torácica contínua; instabilidade hemodinâmica, mecânica ou elétrica; ou choque). Os pacientes tratados devem ser transferidos para realizar uma ICP o mais rapidamente possível após a trombólise.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[144]Borgia F, Goodman SG, Halvorsen S, et al. Early routine percutaneous coronary intervention after fibrinolysis vs. standard therapy in ST-segment elevation myocardial infarction: a meta-analysis. Eur Heart J. 2010 Sep;31(17):2156-69.
https://academic.oup.com/eurheartj/article/31/17/2156/464143
http://www.ncbi.nlm.nih.gov/pubmed/20601393?tool=bestpractice.com
Aqueles transferidos em até 6 horas após a terapia trombolítica tiveram significativamente menos complicações isquêmicas que aqueles que foram transferidos somente se apresentassem complicações.[145]Wijeysundera HC, Vijayaraghavan R, Nallamothu BK, et al. Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials. J Am Coll Cardiol. 2007 Jan 30;49(4):422-30.
https://www.jacc.org/doi/10.1016/j.jacc.2006.09.033
http://www.ncbi.nlm.nih.gov/pubmed/17258087?tool=bestpractice.com
A ICP de resgate está associada a melhores desfechos clínicos após a falha da terapia fibrinolítica.[146]Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009 Jun 25;360(26):2705-18.
https://www.nejm.org/doi/10.1056/NEJMoa0808276
http://www.ncbi.nlm.nih.gov/pubmed/19553646?tool=bestpractice.com
Os agentes antiplaquetários e anticoagulantes (por exemplo, aspirina oral e clopidogrel; heparina intravenosa) também são indicados para o tratamento de IAMCSST, já que limitam a trombose secundária, inibindo a ativação e subsequente agregação plaquetária. O prasugrel e o ticagrelor não são recomendados em pacientes submetidos à trombólise, uma vez que não foram estudados de maneira adequada nesse cenário.[147]Beygui F, Castren M, Brunetti ND, et al. Pre-hospital management of patients with chest pain and/or dyspnoea of cardiac origin. a position paper of the Acute Cardiovascular Care Association (ACCA) of the ESC. Eur Heart J Acute Cardiovasc Care. 2020 Mar;9(1):59-81.
https://academic.oup.com/ehjacc/article/9/1_suppl/59/5923956
http://www.ncbi.nlm.nih.gov/pubmed/26315695?tool=bestpractice.com
Inibidores da GPIIb/IIIa não são indicados no IAMCSST se a terapia trombolítica for indicada. Heparina de baixo peso molecular deve ser considerada ao invés da heparina não fracionada em pacientes tratados com trombólise.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[148]Silvain J, Beygui F, Barthélémy O, et al. Efficacy and safety of enoxaparin versus unfractionated heparin during percutaneous coronary intervention: systematic review and meta-analysis. BMJ. 2012 Feb 3;344:e553.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6653358
http://www.ncbi.nlm.nih.gov/pubmed/22306479?tool=bestpractice.com
[149]Singh S, Bahekar A, Molnar J, et al. Adjunctive low molecular weight heparin during fibrinolytic therapy in acute ST-segment elevation myocardial infarction: a meta-analysis of randomized control trials. Clin Cardiol. 2009 Jul;32(7):358-64.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6653358
http://www.ncbi.nlm.nih.gov/pubmed/19609890?tool=bestpractice.com
As medidas de suporte são as mesmas para pacientes que foram submetidos à ICP em até 90 minutos.
Hemodinamicamente estável: ICP disponível >90 minutos após o primeiro contato com o serviço médico e até 12 horas após o início dos sintomas com contraindicações para trombólise
Em pacientes com contraindicações para trombólise, a ICP é indicada mesmo se não puder ocorrer em até 90 minutos. Os pacientes devem ser transferidos para a realização de ICP o mais rapidamente possível.
Os agentes antiplaquetários/anticoagulantes e as medidas de suporte são as mesmas para pacientes submetidos à ICP em até 90 minutos.
Hemodinamicamente estável: sem acesso à ICP em até 90 minutos e >12 horas após o início dos sintomas
Mesmo depois de 12 horas, caso existam sintomas persistentes, é possível obter benefícios da revascularização, que é mais bem realizada por meio de revascularização coronária percutânea. Pacientes estáveis para os quais a ICP ou a trombólise não for indicada são tratados apenas com farmacoterapia, incluindo betabloqueadores e terapia antiagregante plaquetária e anticoagulação. Se o paciente se tornar instável, ele deve ser submetido à ICP tardia, a qual pode ser realizada até 36 horas após o início dos sintomas.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[150]Hochman JS, Sleeper LA, Godfrey E, et al. Should we emergently revascularize occluded coronaries for cardiogenic shock: an international randomized trial of emergency PTCA/CABG-trial design. The SHOCK Trial Study Group. Am Heart J. 1999 Feb;137(2):313-21.
https://www.sciencedirect.com/science/article/pii/S0002870399005074
http://www.ncbi.nlm.nih.gov/pubmed/9924166?tool=bestpractice.com
A estratégia de ICP primária de rotina ainda deve ser considerada nos pacientes que se apresentarem entre 12 e 48 horas após o início dos sintomas. Entretanto, se o tempo desde o início dos sintomas for >48 horas e o paciente estiver agora assintomático, a ICP de rotina de uma artéria ocluída relacionada ao infarto não é recomendada.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[151]British Cardiovascular Society. PCI in late-presenting STEMI: how late is too late? Jan 2022 [internet publication].
https://www.britishcardiovascularsociety.org/resources/editorials/articles/pci-late-presenting-stemi
As medidas de suporte são as mesmas para pacientes que foram submetidos à ICP em até 90 minutos.
pós-infarto agudo do miocárdio (IAM) com supradesnivelamento do segmento ST (IAMCSST)
As diretrizes da American College of Cardiology/American Heart Association recomendam que, quando disponíveis, programas de prevenção de reabilitação cardíaca/prevenção secundária sejam fornecidos aos pacientes com infarto do miocárdio com supradesnivelamento do segmento ST (IAMCSST), sobretudo àqueles com vários fatores de risco modificáveis e/ou com risco moderado a alto, para os quais é necessário treinamento com exercícios supervisionado.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[152]Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019 Jul 2;140(1):e69-89.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000663
http://www.ncbi.nlm.nih.gov/pubmed/31082266?tool=bestpractice.com
[153]Smith SC Jr, Benjamin EJ, Bonow RO, et al; World Heart Federation and the Preventive Cardiovascular Nurses Association. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. 2011 Nov 29;124(22):2458-73.
https://www.ahajournals.org/doi/10.1161/CIR.0b013e318235eb4d
[154]Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women - 2011 update: a guideline from the American Heart Association. Circulation. 2011 Mar 22;123(11):1243-62.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3182143
http://www.ncbi.nlm.nih.gov/pubmed/21325087?tool=bestpractice.com
Normalmente, os programas de reabilitação cardíaca usam a terapia em grupo para supervisionar e promover um exercício benéfico, assim como fornecer suporte emocional. A reabilitação cardíaca domiciliar também pode ser uma opção.[152]Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019 Jul 2;140(1):e69-89.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000663
http://www.ncbi.nlm.nih.gov/pubmed/31082266?tool=bestpractice.com
Os objetivos da reabilitação cardíaca são[155]Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005 Jan 25;111(3):369-76.
https://www.ahajournals.org/doi/10.1161/01.CIR.0000151788.08740.5C
http://www.ncbi.nlm.nih.gov/pubmed/15668354?tool=bestpractice.com
[156]Brown TM, Pack QR, Aberegg E, et al. Core components of cardiac rehabilitation programs: 2024 update: a scientific statement from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2024 Oct 29;150(18):e328-47.
https://www.ahajournals.org/doi/10.1161/01.CIR.0000151788.08740.5C
http://www.ncbi.nlm.nih.gov/pubmed/39315436?tool=bestpractice.com
Aumentar a capacidade funcional
Interromper o tabagismo
Modificar lipídios e lipoproteínas
Diminuir o peso corporal e o acúmulo de gordura
Reduzir a PA
Melhorar o bem-estar psicossocial
Evitar a progressão e promover a estabilidade da placa
Restaurar e manter um funcionamento físico, psicológico, emocional, social e vocacional ideal.
A reabilitação cardíaca deve ser iniciada no momento da alta e após a anuência de um médico ambulatorial.[156]Brown TM, Pack QR, Aberegg E, et al. Core components of cardiac rehabilitation programs: 2024 update: a scientific statement from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2024 Oct 29;150(18):e328-47.
https://www.ahajournals.org/doi/10.1161/01.CIR.0000151788.08740.5C
http://www.ncbi.nlm.nih.gov/pubmed/39315436?tool=bestpractice.com
Evidências provenientes de revisões sistemáticas têm demonstrado que a reabilitação cardíaca baseada em exercícios ajuda a melhorar os desfechos nas pessoas com doença coronariana.[157]Dibben G, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2021 Nov 6;11(11):CD001800.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001800.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/34741536?tool=bestpractice.com
Os pacientes sem quaisquer fatores de risco preexistentes para doença cardiovascular (DCV) têm um aumento do risco de mortalidade precoce; mesmo os pacientes considerados de baixo risco requerem início imediato de farmacoterapia baseada em evidências após a SCA.[158]Figtree GA, Vernon ST, Hadziosmanovic N, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex-disaggregated analysis of SWEDEHEART registry data. Lancet. 2021 Mar 20;397(10279):1085-94.
http://www.ncbi.nlm.nih.gov/pubmed/33711294?tool=bestpractice.com
Normalmente, a terapia antiagregante plaquetária dupla deve ser continuada em todos os pacientes por, pelo menos, 12 meses, tenham eles recebido stents ou não.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[159]Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018 Jan 14;39(3):213-60.
https://academic.oup.com/eurheartj/article/39/3/213/4095043
Em determinados pacientes submetidos a ICP, pode-se considerar a terapia antiagregante plaquetária dupla de duração mais curta (1-3 meses), com transição subsequente para uma monoterapia com inibidor de P2Y12 para reduzir o risco de eventos de sangramento.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
[160]Kim BK, Hong SJ, Cho YH, et al. Effect of ticagrelor monotherapy vs ticagrelor with aspirin on major bleeding and cardiovascular events in patients with acute coronary syndrome: the TICO randomized clinical trial. JAMA. 2020 Jun 16;323(23):2407-16.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7298605
http://www.ncbi.nlm.nih.gov/pubmed/32543684?tool=bestpractice.com
[161]Kim HS, Kang J, Hwang D, et al. Prasugrel-based de-escalation of dual antiplatelet therapy after percutaneous coronary intervention in patients with acute coronary syndrome (HOST-REDUCE-POLYTECH-ACS): an open-label, multicentre, non-inferiority randomised trial. Lancet. 2020 Oct 10;396(10257):1079-89.
http://www.ncbi.nlm.nih.gov/pubmed/32882163?tool=bestpractice.com
[162]O'Donoghue ML, Murphy SA, Sabatine MS. The safety and efficacy of aspirin discontinuation on a background of a P2Y(12) inhibitor in patients after percutaneous coronary intervention: a systematic review and meta-analysis. Circulation. 2020 Aug 11;142(6):538 45.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.046251
http://www.ncbi.nlm.nih.gov/pubmed/32551860?tool=bestpractice.com
[163]Khan SU, Singh M, Valavoor S, et al. Dual antiplatelet therapy after percutaneous coronary intervention and drug-eluting stents: a systematic review and network meta-analysis. Circulation. 2020 Oct 13;142(15):1425-36.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7547897
http://www.ncbi.nlm.nih.gov/pubmed/32795096?tool=bestpractice.com
[164]Giacoppo D, Matsuda Y, Fovino LN, et al. Short dual antiplatelet therapy followed by P2Y12 inhibitor monotherapy vs. prolonged dual antiplatelet therapy after percutaneous coronary intervention with second-generation drug-eluting stents: a systematic review and meta-analysis of randomized clinical trials. Eur Heart J. 2021 Jan 21;42(4):308-19.
https://academic.oup.com/eurheartj/article/42/4/308/6025040
http://www.ncbi.nlm.nih.gov/pubmed/33284979?tool=bestpractice.com
A terapia com estatinas de alta intensidade deve ser administrada indefinidamente se tolerada e se não houver contraindicações.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[137]Schubert J, Lindahl B, Melhus H, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J. 2021 Jan 20;42(3):243-52.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7954251
http://www.ncbi.nlm.nih.gov/pubmed/33367526?tool=bestpractice.com
Para os pacientes com risco muito alto de eventos futuros e aqueles com até 75 anos de idade e sem risco muito alto, um agente hipolipemiante não estatina, como a ezetimiba, pode ser adicionado se o paciente estiver em terapia máxima com uma estatina e o nível de colesterol LDL permanecer ≥70 mg/dL.[5]Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-e862.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001309
http://www.ncbi.nlm.nih.gov/pubmed/40014670?tool=bestpractice.com
[165]Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082-143.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625
http://www.ncbi.nlm.nih.gov/pubmed/30586774?tool=bestpractice.com
Um inibidor dos anticorpos contra a pró-proteína convertase subtilisina/kexin tipo 9 (PCSK9) (evolocumabe ou alirocumabe) pode ser associado à terapia com doses máximas de estatina e ezetimiba se o paciente apresentar risco muito alto de eventos futuros e o nível de colesterol LDL permanecer ≥70 mg/dL, ou o de colesterol não HDL for ≥100 mg/dL.[3]Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.
https://academic.oup.com/eurheartj/article/44/38/3720/7243210
http://www.ncbi.nlm.nih.gov/pubmed/37622654?tool=bestpractice.com
[47]Szarek M, Bittner VA, Aylward P, et al. Lipoprotein(a) lowering by alirocumab reduces the total burden of cardiovascular events independent of low-density lipoprotein cholesterol lowering: ODYSSEY outcomes trial. Eur Heart J. 2020 Nov 21;41(44):4245-55.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7724642
http://www.ncbi.nlm.nih.gov/pubmed/33051646?tool=bestpractice.com
[165]Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082-143.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625
http://www.ncbi.nlm.nih.gov/pubmed/30586774?tool=bestpractice.com
[166]Oyama K, Giugliano RP, Tang M, et al. Effect of evolocumab on acute arterial events across all vascular territories : results from the FOURIER trial. Eur Heart J. 2021 Dec 14;42(47):4821-9.
https://academic.oup.com/eurheartj/article/42/47/4821/6372436
http://www.ncbi.nlm.nih.gov/pubmed/34537830?tool=bestpractice.com
Os pacientes são considerados de risco muito alto se apresentarem história de vários eventos importantes de DCV aterosclerótica (SCA recente [nos últimos 12 meses], IAM diferente da SCA recente, AVC isquêmico, doença arterial periférica sintomática [claudicação com índice tornozelo-braquial <0.85, revascularização prévia ou amputação]) ou um evento importante de DCV aterosclerótica e várias condições de alto risco (idade ≥65 anos, história familiar heterozigota, história de CRM ou ICP prévia, diabetes mellitus, hipertensão, doença renal crônica, tabagismo vigente, colesterol LDL persistentemente elevado [≥100 mg/dL (≥2.6 mmol/L)] apesar de terapia à dose máxima tolerada, história de insuficiência cardíaca congestiva).[165]Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082-143.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625
http://www.ncbi.nlm.nih.gov/pubmed/30586774?tool=bestpractice.com
Os inibidores da ECA devem ser iniciados precocemente (ou seja, quando o paciente estiver hemodinamicamente estável, idealmente no primeiro dia de internação) para um efeito favorável sobre o remodelamento ventricular, especialmente nos pacientes com IAM da parede anterior. Os betabloqueadores devem ser mantidos em longo prazo (>1 ano), a continuidade do uso deve ser avaliada com base nas comorbidades.[134]Bangalore S, Makani H, Radford M, et al. Clinical outcomes with β-blockers for myocardial infarction: a meta-analysis of randomized trials. Am J Med. 2014 Oct;127(10):939-53.
https://www.amjmed.com/article/S0002-9343(14)00470-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24927909?tool=bestpractice.com
[167]Virani SS, Newby LK, Arnold SV, et al.2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. Circulation. 2023 Aug 29;148(9):e9-119.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001168
http://www.ncbi.nlm.nih.gov/pubmed/37471501?tool=bestpractice.com
[168]Safi S, Sethi NJ, Korang SK, et al. Beta-blockers in patients without heart failure after myocardial infarction. Cochrane Database Syst Rev. 2021 Nov 5;11(11):CD012565.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8570410
http://www.ncbi.nlm.nih.gov/pubmed/34739733?tool=bestpractice.com
[169]Kim J, Kang D, Park H, et al. Long-term β-blocker therapy and clinical outcomes after acute myocardial infarction in patients without heart failure: nationwide cohort study. Eur Heart J. 2020 Oct 1;41(37):3521-9.
https://academic.oup.com/eurheartj/article/41/37/3521/5857797
http://www.ncbi.nlm.nih.gov/pubmed/32542362?tool=bestpractice.com
O American College of Cardiology e a American Heart Association recomendam que a decisão de manter os betabloqueadores em longo prazo após a revascularização seja tomada de forma individualizada.[105]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038
Um inibidor da proteína cotransportadora de sódio e glicose 2 (SGLT2), como dapagliflozina ou empagliflozina, deve ser administrado aos pacientes com insuficiência cardíaca quando estes estiverem clinicamente estáveis, independentemente da fração de ejeção do ventrículo esquerdo.[170]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
[171]McDonagh TA, Metra M, Adamo M, et al. 2023 Focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023 Oct 1;44(37):3627-39.
https://academic.oup.com/eurheartj/article/44/37/3627/7246292
[172]von Lewinski D, Kolesnik E, Tripolt NJ, et al. Empagliflozin in acute myocardial infarction: the EMMY trial. Eur Heart J. 2022 Nov 1;43(41):4421-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9622301
http://www.ncbi.nlm.nih.gov/pubmed/36036746?tool=bestpractice.com
O uso crônico de nitratos não é rotineiramente recomendado após um IAM, mas pode ser usado como parte do plano de tratamento para insuficiência cardíaca congestiva (ICC) e para angina crônica.
 ]
]
 ]
Os stents farmacológicos de terceira geração compostos de polímeros biodegradáveis estão sendo pesquisados atualmente.[123][124][Figure caption and citation for the preceding image starts]: Angiografia mostrando a artéria coronária direita obstruídaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
]
Os stents farmacológicos de terceira geração compostos de polímeros biodegradáveis estão sendo pesquisados atualmente.[123][124][Figure caption and citation for the preceding image starts]: Angiografia mostrando a artéria coronária direita obstruídaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].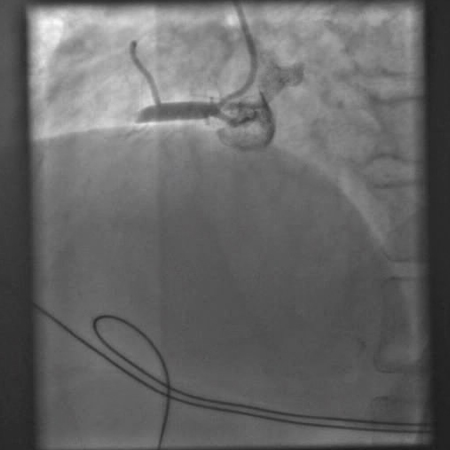 [Figure caption and citation for the preceding image starts]: Angiografia mostrando uma tentativa de abrir a artéria coronária direita obstruída com um balão de angioplastiaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Angiografia mostrando uma tentativa de abrir a artéria coronária direita obstruída com um balão de angioplastiaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].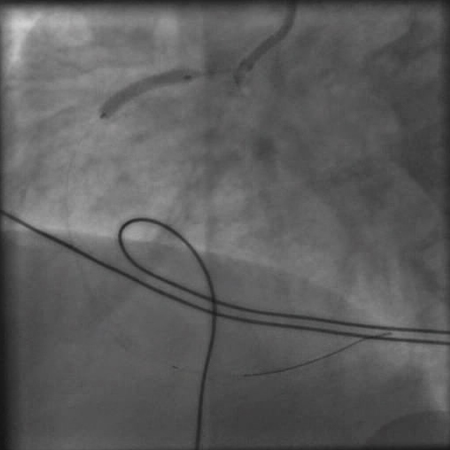 [Figure caption and citation for the preceding image starts]: Angiografia após a angioplastia com balão e colocação de stent mostrando uma artéria coronária direita abertaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Angiografia após a angioplastia com balão e colocação de stent mostrando uma artéria coronária direita abertaDo acervo pessoal do Dr. Mahi Ashwath; usado com permissão [Citation ends].