A dor biliar, o sintoma mais comum de colelitíase, resulta da obstrução do ducto cístico ou da obstrução e/ou passagem de um cálculo biliar pelo ducto colédoco. Dor biliar, colecistite, colangite ou pancreatite desenvolvem-se anualmente em 1% a 2% dos indivíduos com colelitíase assintomática.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[2]Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012 Apr;6(2):172-87.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3343155
http://www.ncbi.nlm.nih.gov/pubmed/22570746?tool=bestpractice.com
[9]Abraham S, Rivero HG, Erlikh IV, et al. Surgical and nonsurgical management of gallstones. Am Fam Physician. 2014 May 15;89(10):795-802.
http://www.ncbi.nlm.nih.gov/pubmed/24866215?tool=bestpractice.com
[14]Freidman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol. 1989;42(2):127-36.
http://www.ncbi.nlm.nih.gov/pubmed/2918322?tool=bestpractice.com
[15]Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982 Sep 23;307(13):798-800.
http://www.ncbi.nlm.nih.gov/pubmed/7110244?tool=bestpractice.com
[16]McSherry CK, Ferstenberg H, Calhoun WF, et al. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985 Jul;202(1):59-63.
http://www.ncbi.nlm.nih.gov/pubmed/4015212?tool=bestpractice.com
[17]Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg. 1993 Apr;165(4):399-404.
http://www.ncbi.nlm.nih.gov/pubmed/8480871?tool=bestpractice.com
As características de colecistite, colangite e pancreatite podem se sobrepor clinicamente; portanto, o diagnóstico por exames de imagem acurados é essencial. Além da avaliação laboratorial padrão, o exame radiográfico inicial escolhido para a colelitíase sintomática é a ultrassonografia transabdominal.'[72]Ross M, Brown M, McLaughlin K, et al. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011 Mar;18(3):227-35.
http://www.ncbi.nlm.nih.gov/pubmed/21401784?tool=bestpractice.com
[73]Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020 Nov 5;15(1):61.
https://wjes.biomedcentral.com/articles/10.1186/s13017-020-00336-x
http://www.ncbi.nlm.nih.gov/pubmed/33153472?tool=bestpractice.com
A escolha do próximo exame de imagem depende do índice de suspeita clínica para complicações da colelitíase.
História
A dor biliar típica (cólica biliar) ocorre no quadrante superior direito do abdome ou na região epigástrica, às vezes após o consumo de alimentos, geralmente cerca de 1 hora após a alimentação, particularmente ao fim do dia e à noite.[74]Berhane T, Vetrhus M, Hausken T, et al. Pain attacks in non-complicated and complicated gallstone disease have a characteristic pattern and are accompanied by dyspepsia in most patients: the results of a prospective study. Scand J Gastroenterol. 2006 Jan;41(1):93-101.
http://www.ncbi.nlm.nih.gov/pubmed/16373282?tool=bestpractice.com
Essa dor constante aumenta em intensidade e dura várias horas. A dor de curta duração (<30 minutos) não é cólica biliar, ao passo que a dor de longa duração (mais de 5 horas) sugere colecistite ou outra complicação importante.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
A dor pode ser acompanhada de náuseas.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
Os fatores de risco devem ser identificados; estes incluem história familiar positiva, obesidade, diabetes, síndrome metabólica, uso de certos medicamentos (por exemplo, octreotida, agonistas do receptor do peptídeo semelhante ao glucagon 1, ceftriaxona), doença do íleo terminal, gravidez, cirrose e anemia hemolítica (por exemplo, anemia falciforme ou talassemia).[4]Nakeeb A, Comuzzie AG, Martin L, et al. Gallstones: genetics versus environment. Ann Surg. 2002 Jun;235(6):842-9.
http://www.ncbi.nlm.nih.gov/pubmed/12035041?tool=bestpractice.com
[5]Katsika D, Grjibovski A, Einarsson C, et al. Genetic and environmental influences on symptomatic gallstone disease: a Swedish study of 43,141 twin pairs. Hepatology. 2005 May;41(5):1138-43.
http://www.ncbi.nlm.nih.gov/pubmed/15747383?tool=bestpractice.com
[21]Stampfer MJ, Maclure KM, Colditz GA, et al. Risk of symptomatic gallstones in women with severe obesity. Am J Clin Nutr. 1992 Mar;55(3):652-8.
http://www.ncbi.nlm.nih.gov/pubmed/1550039?tool=bestpractice.com
[22]Stolk MF, van Erpecum KJ, Koppeschaar HP, et al. Postprandial gall bladder motility and hormone release during intermittent and continuous subcutaneous octreotide treatment in acromegaly. Gut. 1993 Jun;34(6):808-13.
https://www.doi.org/10.1136/gut.34.6.808
http://www.ncbi.nlm.nih.gov/pubmed/8314514?tool=bestpractice.com
[51]Faillie JL, Yu OH, Yin H, et al. Association of bile duct and gallbladder diseases with the use of incretin-based drugs in patients with type 2 diabetes mellitus. JAMA Intern Med. 2016 Oct 1;176(10):1474-81.
http://www.ncbi.nlm.nih.gov/pubmed/27478902?tool=bestpractice.com
[53]Becker CD, Fischer RA. Acute cholecystitis caused by ceftriaxone stones in an adult. Case Rep Med. 2009 Apr 26;2009:132452.
https://www.hindawi.com/journals/crim/2009/132452
http://www.ncbi.nlm.nih.gov/pubmed/19707473?tool=bestpractice.com
[54]Parente F, Pastore L, Bargiggia S, et al. Incidence and risk factors for gallstones in patients with inflammatory bowel disease: a large case-control study. Hepatology. 2007 May;45(5):1267-74.
http://www.ncbi.nlm.nih.gov/pubmed/17464998?tool=bestpractice.com
Exame físico
O exame físico se concentra na identificação de sinais de quaisquer complicações da colelitíase. O sinal de Murphy (parada inspiratória ao palpar a fossa da vesícula biliar) é a característica mais comum do exame abdominal em pacientes com colelitíase sintomática.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
Tem alta sensibilidade (97%), mas baixa especificidade (48%) para colecistite aguda.[75]Singer AJ, McCracken G, Henry MC, et al.Correlation among clinical, laboratory, and hepatobiliary scanning findings in patients with suspected acute cholecystitis. Ann Emerg Med. 1996 Sep;28(3):267-72.
http://www.ncbi.nlm.nih.gov/pubmed/8780468?tool=bestpractice.com
Dispepsia, pirose, flatulência e distensão abdominal são comuns, mas não são característicos da litíase biliar.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[2]Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012 Apr;6(2):172-87.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3343155
http://www.ncbi.nlm.nih.gov/pubmed/22570746?tool=bestpractice.com
A febre sugere uma complicação como colecistite aguda. A icterícia é rara na colecistite aguda simples, sendo mais sugestiva de cálculo no ducto comum, colangite ou pancreatite.[31]Tazuma S, Unno M, Igarashi Y, et al. Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol. 2017 Mar;52(3):276-300.
https://link.springer.com/article/10.1007/s00535-016-1289-7
http://www.ncbi.nlm.nih.gov/pubmed/27942871?tool=bestpractice.com
[76]Narula VK, Fung EC, Overby DW, et al. Clinical spotlight review for the management of choledocholithiasis. Surg Endosc. 2020 Apr;34(4):1482-91.
http://www.ncbi.nlm.nih.gov/pubmed/32095952?tool=bestpractice.com
Exames laboratoriais
Geralmente, o hemograma completo e a bioquímica hepática apresentam resultados normais com um episódio de dor biliar simples.
Uma contagem elevada de leucócitos sugere colecistite, colangite ou pancreatite aguda.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[31]Tazuma S, Unno M, Igarashi Y, et al. Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol. 2017 Mar;52(3):276-300.
https://link.springer.com/article/10.1007/s00535-016-1289-7
http://www.ncbi.nlm.nih.gov/pubmed/27942871?tool=bestpractice.com
Consulte Colecistite aguda e Colangite aguda.
A coledocolitíase obstrutiva normalmente é associada a testes da função hepática alterados; especificamente, fosfatase alcalina elevada e bilirrubina elevada.
Uma breve obstrução biliar, com subsequente expulsão do cálculo, causa uma precoce elevação transitória da alanina aminotransferase, antes do aumento da fosfatase alcalina.[77]Patwardhan RV, Smith OJ, Farmelant MH. Serum transaminase levels and cholescintigraphic abnormalities in acute biliary tract obstruction. Arch Intern Med. 1987 Jul;147(7):1249-53.
http://www.ncbi.nlm.nih.gov/pubmed/3300588?tool=bestpractice.com
Os pacientes que apresentam dor abdominal intensa de início súbito no quadrante superior esquerdo ou na região epigástrica média (com ou sem irradiação para as costas) devem ter níveis de lipase sérica solicitados para se descartar a pancreatite.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
Consulte Pancreatite aguda.
Os dois testes têm sensibilidade e especificidade parecidas, mas os níveis de lipase continuam elevados por mais tempo (até 14 dias após o início dos sintomas vs. 5 dias para a amilase), fornecendo uma maior probabilidade de se pegar o diagnóstico nos pacientes com uma apresentação tardia.[78]Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Jul 30;108(9):1400-15.
https://journals.lww.com/ajg/fulltext/2013/09000/American_College_of_Gastroenterology_Guideline_.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/23896955?tool=bestpractice.com
[79]Rompianesi G, Hann A, Komolafe O, et al. Serum amylase and lipase and urinary trypsinogen and amylase for diagnosis of acute pancreatitis. Cochrane Database Syst Rev. 2017 Apr 21;4(4):CD012010.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012010.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/28431198?tool=bestpractice.com
Ultrassonografia abdominal
O exame de imagem inicial de escolha em pacientes com suspeita de dor biliar é a ultrassonografia abdominal para detectar cálculos biliares ou dilatação do ducto biliar causada por obstrução biliar.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[72]Ross M, Brown M, McLaughlin K, et al. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011 Mar;18(3):227-35.
http://www.ncbi.nlm.nih.gov/pubmed/21401784?tool=bestpractice.com
[73]Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020 Nov 5;15(1):61.
https://wjes.biomedcentral.com/articles/10.1186/s13017-020-00336-x
http://www.ncbi.nlm.nih.gov/pubmed/33153472?tool=bestpractice.com
[80]American College of Radiology. ACR appropriateness criteria: right upper quadrant pain. 2022 [internet publication].
https://acsearch.acr.org/docs/69474/Narrative
[81]National Institute for Health and Care Excellence. Gallstone disease: diagnosis and management. Oct 2014 [internet publication].
https://www.nice.org.uk/guidance/cg188
Se disponível, a ultrassonografia no local de atendimento (POCUS) direcionada, realizada à beira do leito, pode ajudar a diagnosticar cálculos biliares e agilizar a tomada de decisões clínicas subsequentes.[72]Ross M, Brown M, McLaughlin K, et al. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011 Mar;18(3):227-35.
http://www.ncbi.nlm.nih.gov/pubmed/21401784?tool=bestpractice.com
[73]Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020 Nov 5;15(1):61.
https://wjes.biomedcentral.com/articles/10.1186/s13017-020-00336-x
http://www.ncbi.nlm.nih.gov/pubmed/33153472?tool=bestpractice.com
[82]Pereira J, Bass GA, Mariani D, et al. Surgeon-performed point-of-care ultrasound for acute cholecystitis: indications and limitations: a European Society for Trauma and Emergency Surgery (ESTES) consensus statement. Eur J Trauma Emerg Surg. 2020 Feb;46(1):173-83.
http://www.ncbi.nlm.nih.gov/pubmed/31435701?tool=bestpractice.com
[83]Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-care ultrasonography. N Engl J Med. 2021 Oct 21;385(17):1593-602.
http://www.ncbi.nlm.nih.gov/pubmed/34670045?tool=bestpractice.com
A ultrassonografia abdominal, no entanto, tem baixa sensibilidade para coledocolitíase, apesar de ser precisa na identificação de qualquer dilatação do ducto biliar associada.[84]Pinto A, Reginelli A, Cagini L, et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J. 2013 Jul 15;5(suppl 1):S11.
https://theultrasoundjournal.springeropen.com/articles/10.1186/2036-7902-5-S1-S11
http://www.ncbi.nlm.nih.gov/pubmed/23902680?tool=bestpractice.com
[85]De Angelis C, Marietti M, Bruno M, et al. Endoscopic ultrasound in common bile duct dilatation with normal liver enzymes. World J Gastrointest Endosc. 2015 Jul 10;7(8):799-805.
https://www.wjgnet.com/1948-5190/full/v7/i8/799.htm
http://www.ncbi.nlm.nih.gov/pubmed/26191344?tool=bestpractice.com
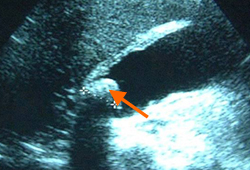
Para a colecistite aguda, a ultrassonografia abdominal tem grande sensibilidade para detectar cálculos e distensão do lúmen da vesícula biliar, além de qualquer característica inflamatória, espessamento da parede da vesícula biliar, fluido pericolecístico e/ou sinal de Murphy radiológico positivo.[84]Pinto A, Reginelli A, Cagini L, et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J. 2013 Jul 15;5(suppl 1):S11.
https://theultrasoundjournal.springeropen.com/articles/10.1186/2036-7902-5-S1-S11
http://www.ncbi.nlm.nih.gov/pubmed/23902680?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Ultrassonografia de colecistite aguda e presença de cálculos biliares: a seta aponta para um cálculo no fundo da vesícula biliar, com sua sombra ecogênica abaixoCortesia de Charles Bellows e W. Scott Helton; usado com permissão [Citation ends].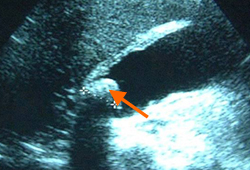 [Figure caption and citation for the preceding image starts]: Ultrassonografia de vesícula biliar demonstrando colelitíase com sombreamento característicoCortesia de Kuojen Tsao; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrassonografia de vesícula biliar demonstrando colelitíase com sombreamento característicoCortesia de Kuojen Tsao; usado com permissão [Citation ends].
Exames de imagem subsequentes
Podem ser necessários exames de imagem adicionais, com base nas características clínicas e do índice associado de suspeita clínica para complicações.
Se houver suspeita de coledocolitíase (por exemplo, ductos biliares dilatados ou bioquímica hepática anormal), é necessária colangiopancreatografia por ressonância magnética (CPRM) ou ultrassonografia endoscópica (USE).[76]Narula VK, Fung EC, Overby DW, et al. Clinical spotlight review for the management of choledocholithiasis. Surg Endosc. 2020 Apr;34(4):1482-91.
http://www.ncbi.nlm.nih.gov/pubmed/32095952?tool=bestpractice.com
[84]Pinto A, Reginelli A, Cagini L, et al. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. Crit Ultrasound J. 2013 Jul 15;5(suppl 1):S11.
https://theultrasoundjournal.springeropen.com/articles/10.1186/2036-7902-5-S1-S11
http://www.ncbi.nlm.nih.gov/pubmed/23902680?tool=bestpractice.com
A CPRM tem sensibilidade de 95% e especificidade de 97% para a detecção de cálculos nos ductos biliares.[76]Narula VK, Fung EC, Overby DW, et al. Clinical spotlight review for the management of choledocholithiasis. Surg Endosc. 2020 Apr;34(4):1482-91.
http://www.ncbi.nlm.nih.gov/pubmed/32095952?tool=bestpractice.com
[86]Romagnuolo J, Bardou M, Rahme E, et al. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2003 Oct 7;139(7):547-57.
http://www.ncbi.nlm.nih.gov/pubmed/14530225?tool=bestpractice.com
no entanto, ela tem sensibilidade reduzida (65%) para a detecção de cálculos biliares pequenos (<5 mm).[86]Romagnuolo J, Bardou M, Rahme E, et al. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2003 Oct 7;139(7):547-57.
http://www.ncbi.nlm.nih.gov/pubmed/14530225?tool=bestpractice.com
[87]Kondo S, Isayama H, Akahane M, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005 May;54(2):271-5.
http://www.ncbi.nlm.nih.gov/pubmed/15837409?tool=bestpractice.com
A USE é igualmente precisa para a detecção de cálculos no ducto biliar, especialmente em pacientes que não podem se submeter a uma CPRM (por exemplo, aqueles com dispositivos implantados). Dependendo da qualificação local, a USE pode ser mais precisa que a CPRM, e pode ser útil para detectar pacientes com risco baixo a moderado de cálculos nos ductos biliares (imagens negativas, mas sintomas e/ou exames de sangue positivos) que se beneficiariam de uma colangiopancreatografia retrógrada endoscópica (CPRE) subsequente.[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[20]ASGE Standards of Practice Committee; Buxbaum JL, Abbas Fehmi SM, Sultan S, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019 Jun;89(6):1075-105;e15.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8594622
http://www.ncbi.nlm.nih.gov/pubmed/30979521?tool=bestpractice.com
[88]Meeralam Y, Al-Shammari K, Yaghoobi M. Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc. 2017 Jun 20;86(6):986-93.
http://www.ncbi.nlm.nih.gov/pubmed/28645544?tool=bestpractice.com
[89]Thorbøll J, Vilmann P, Jacobsen B, et al. Endoscopic ultrasonography in detection of cholelithiasis in patients with biliary pain and negative transabdominal ultrasonography. Scand J Gastroenterol. 2004 Mar;39(3):267-9.
http://www.ncbi.nlm.nih.gov/pubmed/15074397?tool=bestpractice.com
[90]Karakan T, Cindoruk M, Alagozlu H, et al. EUS versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a prospective randomized trial. Gastrointest Endosc. 2009 Feb;69(2):244-52.
http://www.ncbi.nlm.nih.gov/pubmed/19019364?tool=bestpractice.com
[91]Janssen J, Halboos A, Greiner L. EUS accurately predicts the need for therapeutic ERCP in patients with a low probability of biliary obstruction. Gastrointest Endosc. 2008 Sep;68(3):470-6.
http://www.ncbi.nlm.nih.gov/pubmed/18547571?tool=bestpractice.com
[92]Lee YT, Chan FK, Leung WK, et al. Comparison of EUS and ERCP in the investigation with suspected biliary obstruction caused by choledocholithiasis: a randomized study. Gastrointest Endosc. 2008 Apr;67(4):660-8.
http://www.ncbi.nlm.nih.gov/pubmed/18155205?tool=bestpractice.com
[93]Liu CL, Fan ST, Lo CM, et al. Comparison of early endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: a prospective randomized study. Clin Gastroenterol Hepatol. 2005 Dec;3(12):1238-44.
http://www.ncbi.nlm.nih.gov/pubmed/16361050?tool=bestpractice.com
[94]Polkowski M, Regula J, Tilszer A, et al. Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a randomized trial comparing two management strategies. Endoscopy. 2007 Apr;39(4):296-303.
http://www.ncbi.nlm.nih.gov/pubmed/17427065?tool=bestpractice.com
[95]Zhang J, Li NP, Huang BC, et al. The value of performing early non-enhanced CT in developing strategies for treating acute gallstone pancreatitis. J Gastrointest Surg. 2016 Mar;20(3):604-10.
http://www.ncbi.nlm.nih.gov/pubmed/26743886?tool=bestpractice.com
Se a imagem inicial for negativa, mas as características clínicas e/ou exames de sangue sugerirem coledocolitíase e o paciente apresentar alto risco de complicações (por exemplo, colangite aguda, pancreatite aguda), a CPRE é recomendada. A CPRE pode ser tanto diagnóstica quanto terapêutica, permitindo a remoção de quaisquer cálculos obstrutivos para proporcionar drenagem biliar.[94]Polkowski M, Regula J, Tilszer A, et al. Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a randomized trial comparing two management strategies. Endoscopy. 2007 Apr;39(4):296-303.
http://www.ncbi.nlm.nih.gov/pubmed/17427065?tool=bestpractice.com
[  ]
How does early routine endoscopic retrograde cholangiopancreatography compare with early conservative management in people with acute gallstone pancreatitis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.867/fullMostre-me a resposta[Evidência B]a26907fc-423b-47b2-9baa-43fb7efd6214ccaBComo a colangiopancreatografia retrógrada endoscópica (CPRE) precoce de rotina se compara ao tratamento conservador precoce em pessoas com pancreatite biliar aguda?
]
How does early routine endoscopic retrograde cholangiopancreatography compare with early conservative management in people with acute gallstone pancreatitis?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.867/fullMostre-me a resposta[Evidência B]a26907fc-423b-47b2-9baa-43fb7efd6214ccaBComo a colangiopancreatografia retrógrada endoscópica (CPRE) precoce de rotina se compara ao tratamento conservador precoce em pessoas com pancreatite biliar aguda?
Em caso de ultrassonografia abdominal normal na presença de dor biliar, pode ser necessária uma tomografia computadorizada abdominal para avaliar diagnósticos alternativos (por exemplo, colangite aguda ou pancreatite biliar) e identificar possíveis complicações de colecistite aguda (por exemplo, enfisema da parede da vesícula biliar, formação de abscesso, perfuração).[1]European Association for the Study of the Liver. EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-81.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30032-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27085810?tool=bestpractice.com
[80]American College of Radiology. ACR appropriateness criteria: right upper quadrant pain. 2022 [internet publication].
https://acsearch.acr.org/docs/69474/Narrative
[95]Zhang J, Li NP, Huang BC, et al. The value of performing early non-enhanced CT in developing strategies for treating acute gallstone pancreatitis. J Gastrointest Surg. 2016 Mar;20(3):604-10.
http://www.ncbi.nlm.nih.gov/pubmed/26743886?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Ultrassonografia de vesícula biliar demonstrando colelitíase com sombreamento característicoCortesia de Kuojen Tsao; usado com permissão [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrassonografia de vesícula biliar demonstrando colelitíase com sombreamento característicoCortesia de Kuojen Tsao; usado com permissão [Citation ends].
 ]
[Evidência B]
]
[Evidência B]