History and exam
Key diagnostic factors
common
presence of risk factors
Key risk factors include increased skin pigmentation, obesity, malabsorption syndromes, history of liver failure or chronic kidney disease, adults aged >50 years, history of benign or malignant tumour, and patients taking certain drugs; for example, glucocorticoids (e.g., dexamethasone), anticonvulsants (e.g., phenytoin, carbamazepine), antiretroviral therapy (ART; e.g., ritonavir), rifampicin, and St. John's wort.[82][76] Children and adults with inadequate sun exposure and who do not take a vitamin D supplement are also at high risk, as are neonates whose sole source of nutrition is breast milk and who receive no vitamin D supplementation.[3][68]
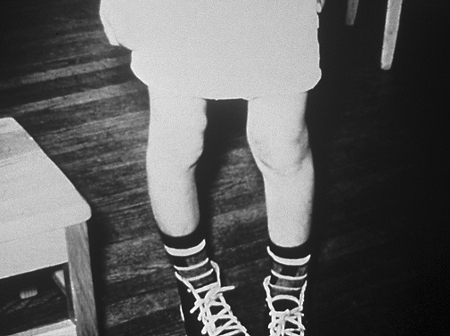
bowing of the legs
widening of the ends of the long bones
In children, vitamin D deficiency causes hypertrophy of the epiphyseal plates of the long bones, resulting in widening of the wrists. This can be verified with x-ray, which shows ragged poor mineralisation of the epiphyseal plates.[95][101][Figure caption and citation for the preceding image starts]: X-rays of a wrist from a child with vitamin D-deficiency rickets before (left panel) and after (right panel) treatment with vitamin DFrom the collection of M.F. Holick, PhD, MD; used with permission [Citation ends].
delayed tooth eruption and early dental caries
Occurs in children with rickets.[101]
chest deformity
throbbing, aching bone discomfort and/or irritability
Bone discomfort is typical of prolonged or severe vitamin D deficiency in adults (osteomalacia). Patients often report bone pain when sitting or lying down and describe the pain as unrelenting and throbbing.
In infants or young children with rickets, bone pain is usually expressed as irritability.[95][99][101]
head sweating
Can occur in children with severe vitamin D deficiency, due to an increase in neuromuscular activity.[101]
localised or generalised bone tenderness
Periosteal bone discomfort consistent with the diagnosis of osteomalacia can be elicited by pressing with a fair amount of force on the sternum, radius, and anterior tibia using thumb or forefinger.[7]
uncommon
rachitic rosary
frontal bossing
waddling gait
Due to pain in the hips, and is a sign of osteomalacia.
Other diagnostic factors
common
delayed growth
delayed achievement of motor milestones
fatigue and malaise
Common symptoms in patients with osteomalacia.[7]
uncommon
symptoms of hypocalcaemia
Include muscle cramps, muscle weakness, carpal pedal spasm, numbness, paraesthesias, tetany, and seizures.[95][101]
Can occur as a result of inherited disorders of vitamin D metabolism or chronic untreated vitamin D deficiency. Carpal pedal spasms and generalised seizures can occur due to increased neuromuscular irritability.[95][101]
Risk factors
strong
inadequate sunlight exposure
Sunlight is the major source of vitamin D for most humans. Therefore, avoiding sun exposure (e.g., with clothing which covers the majority of skin), being housebound, season, latitude, and time of day influence cutaneous vitamin D production.[3][15][78] Sunscreen with a sun protection factor of 30 when properly applied (2 mg/cm²) will absorb approximately 95% to 98% of incident ultraviolet B (UV-B) solar radiation, thereby reducing the production of vitamin D3 in the skin by 95% to 98%.[3][15] However, it should be noted that the exact impact on vitamin D production can vary based on factors such as the amount of sunscreen applied, the frequency of reapplication, the type of sunscreen, skin type, and the intensity of sun exposure.
Living above or below a latitude of 35° either markedly reduces or completely eliminates any vitamin D production from sunlight exposure in the winter.[15]
Vitamin D photosynthesis depends on many factors including genetics, age, health, and personal and cultural behaviour.[78] Particularly susceptible groups include older people (especially if institutionalised) and women and children who are confined to the home, or who wear clothing that covers the entire body and face.[15]
increased skin pigmentation
Melanin efficiently absorbs UV-B solar radiation. Therefore, an increase in the melanin content in the epidermis results in a decrease in the production of vitamin D. As a result, this can cause a decrease in circulating concentrations of 25-hydroxyvitamin D compared to skin that has little or no melanin pigmentation and designated as skin type 1 and 2 based on the Fitzpatrick skin type scale.[15][66]
age >50 years
Ageing does not affect vitamin D absorption from the diet, but it does decrease the ability of the skin to produce vitamin D.[15][67]
The increase in the blood concentration of vitamin D following UV-B radiation exposure is at least threefold higher in young adults aged 20-30 years, compared with older adults aged 62-80 years.[15]
inadequate dietary and supplemental vitamin D intake
There are high levels of inadequacy of vitamin D intake within populations around the globe, in part due to variability in availability of vitamin-D rich food sources and differences in the practice of food fortification between countries.[16] Most estimates do not include the contribution from vitamin D-containing dietary supplements.[7][16]
Infants receiving breast milk as their sole source of nutrition, without vitamin D supplementation, are most susceptible.[68]
malabsorption
Patients with coeliac disease, cystic fibrosis, Crohn's disease, Whipple's disease, or short bowel syndrome, or who have undergone gastric bypass surgery, are unable to absorb or poorly absorb vitamin D.[71]
Severe liver failure is associated with vitamin D deficiency.[72] Intestinal malabsorption of vitamin D due to cholestasis is one of the potential mechanisms for vitamin D deficiency in chronic liver disease.[73] When >90% of the liver fails, it is incapable of producing enough 25-hydroxyvitamin D.[3][7]
obesity
Body fat stores vitamin D. However, when BMI is >30 kg/m² adipose tissue sequesters vitamin D, thus increasing the risk for vitamin D deficiency.[74]
use of certain drugs
Includes the use of glucocorticoids (e.g., dexamethasone), anticonvulsants (e.g., phenytoin, carbamazepine), antiretroviral therapy (ART; e.g., ritonavir), rifampicin, and St. John's wort. These drugs activate the steroid and xenobiotic receptors, which results in activation of the enzymatic machinery destroying 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D.[76]
genetic mutations
Inherited disorders of vitamin D metabolism and 1,25-dihydroxyvitamin D recognition are rare.[9]
Vitamin D-dependent rickets type 1 is caused by mutations of genes that generate 25-hydroxyvitamin-1-hydroxylase or 25-hydroxylase.[10]
Vitamin D-dependent rickets type 2 is caused by a mutation of the vitamin D receptor (VDR) gene.[10]
X-linked hypophosphataemic rickets and autosomal-dominant hypophosphataemic rickets are caused by the enhanced production or decreased metabolism of fibroblast growth factor 23. This results in hyperphosphaturia, severe hypophosphataemia, and reduction in the conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D.[12]
history of benign or malignant tumour
Whether benign or malignant, some tumours can produce fibroblast growth factor 23, causing hypophosphataemia and low levels of serum 1,25-dihydroxyvitamin D, with consequent oncogenic osteomalacia and pronounced biochemical and skeletal manifestations.[8]
chronic kidney disease
The kidneys activate vitamin D in order to regulate calcium metabolism. Therefore, patients with chronic kidney disease with a GFR of <50% of normal are unable to produce enough 1,25-dihydroxyvitamin D for this purpose. This results in secondary hyperparathyroidism and metabolic bone disease.
granulomatous disorders
Patients with granuloma-forming diseases, including sarcoidosis and tuberculosis, are at risk for vitamin D deficiency due to its enhanced destruction. Macrophages in the granuloma can cause increased metabolism of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D, resulting in increased expression of the enzyme 24-hydroxylase, which in turn increases the destruction of both 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D, resulting in vitamin D deficiency.[7]
primary hyperparathyroidism
High PTH levels can cause increased metabolism of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D, resulting in increased expression of the enzyme 24-hydroxylase, which in turn increases the destruction of both 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D, resulting in vitamin D deficiency.[7]
hyperthyroidism
Enhances the metabolism of 25-hydroxyvitamin D, resulting in reduced levels.[7]
Use of this content is subject to our disclaimer