Vitamin D deficiency is frequently underdiagnosed in children and adults, primarily because patients do not typically present with overt clinical signs and symptoms until the deficiency is severe and prolonged. In growing children, vitamin D deficiency will reduce bone mineral deposition (resulting in the skeletal manifestations of rickets), developmental delay, and delayed growth.[88]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-37.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
In adults, vitamin D deficiency causes a defect in mineralisation of the collagen matrix such that they present with signs and symptoms of osteomalacia (bone pain and tenderness, proximal muscle weakness reported as difficulty rising from a sitting position).[88]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-37.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
The hallmark for diagnosing vitamin D deficiency is the measurement of serum 25-hydroxyvitamin D.[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
Although several inherited or acquired disorders of vitamin D metabolism do not result in a serum 25-hydroxyvitamin D level of <50 nanomoles/L (<20 nanograms/mL), they are still considered causes of vitamin D deficiency and usually present in the same manner, often with more severe skeletal deformities and metabolic bone disease.[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[9]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
History
Establish risk factors for vitamin D deficiency when taking a history.
Groups at high risk for vitamin D deficiency include:[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[15]Wacker M, Holick MF. Sunlight and vitamin D: a global perspective for health. Dermatoendocrinol. 2013 Jan 1;5(1):51-108.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897598
http://www.ncbi.nlm.nih.gov/pubmed/24494042?tool=bestpractice.com
[26]Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. 2020 Jul 15;12(7):2097.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400911
http://www.ncbi.nlm.nih.gov/pubmed/32679784?tool=bestpractice.com
[74]Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000 Sep;72(3):690-3. [Erratum in: Am J Clin Nutr. 2003 May;77(5):1342.]
http://ajcn.nutrition.org/content/72/3/690.full
http://www.ncbi.nlm.nih.gov/pubmed/10966885?tool=bestpractice.com
[76]Gröber U, Kisters K. Influence of drugs on vitamin D and calcium metabolism. Dermatoendocrinol. 2012 Apr 1;4(2):158-66.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3427195
http://www.ncbi.nlm.nih.gov/pubmed/22928072?tool=bestpractice.com
[89]MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985 Oct;76(4):1536-8.
https://www.jci.org/articles/view/112134/pdf
http://www.ncbi.nlm.nih.gov/pubmed/2997282?tool=bestpractice.com
[90]Gallagher JC, Peacock M, Yalamanchili V, et al. Effects of vitamin D supplementation in older African American women. J Clin Endocrinol Metab. 2013 Mar;98(3):1137-46.
http://www.ncbi.nlm.nih.gov/pubmed/23386641?tool=bestpractice.com
[91]Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008 Aug;88(2):558S-64S.
https://www.sciencedirect.com/science/article/pii/S0002916523241131?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/18689402?tool=bestpractice.com
Neonates who receive breast milk as their sole nutrition with no vitamin D supplementation
Children and adults with darker and black skin
Patients with malabsorption syndromes (coeliac disease, cystic fibrosis, short bowel syndrome, inflammatory bowel disease, Whipple's disease), including those who have undergone gastric bypass surgery
Children and adults who are institutionalised, exposed to minimal sunlight, who always wear sun protection before going outdoors, or who live in cold climates
Adult >50 years of age (have reduced synthetic capacity to make vitamin D in their skin)
People with obesity (BMI >30 kg/m² (requirement of 2-3 times more vitamin D than the general population to satisfy vitamin D requirements)
People who take certain prescription or non-prescription drugs including glucocorticoids, anticonvulsants antiretroviral therapy (ART), rifampicin, or St. John's wort
Children who do not receive at least 600 IU/day of vitamin D from diet and supplements, and adults who do not receive at least 1500-2000 IU/day of vitamin D from diet and supplements, may be vitamin D-deficient or -insufficient (see Primary prevention).[17]Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020 Nov;74(11):1498-513.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7091696
http://www.ncbi.nlm.nih.gov/pubmed/31959942?tool=bestpractice.com
[85]Heaney RP, Armas LA, French C. All-source basal vitamin D inputs are greater than previously thought and cutaneous inputs are smaller. J Nutr. 2013 May;143(5):571-5.
https://www.sciencedirect.com/science/article/pii/S0022316622011683?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/23514768?tool=bestpractice.com
[86]Hamid Z, Riggs A, Spencer T, et al. Vitamin D deficiency in residents of academic long-term care facilities despite having been prescribed vitamin D. J Am Med Dir Assoc. 2007 Feb;8(2):71-5.
http://www.ncbi.nlm.nih.gov/pubmed/17289534?tool=bestpractice.com
In mild or early disease, patients may be completely asymptomatic. Decreased growth and delayed achievement of motor milestones are common childhood presentations of rickets. In adults with severe or prolonged vitamin D deficiency, symptoms of osteomalacia typically include throbbing, aching bone discomfort that can be localised or generalised.[88]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-37.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
In addition, easy fatiguability and malaise are common symptoms. Patients may also report difficulty in rising from a sitting position (due to proximal muscle weakness), and a waddling gait. Patients with oncogenic osteomalacia usually present with non-specific symptoms of muscle weakness and aching bone pain.[8]Jan de Beur SM, Minisola S, Xia WB, et al. Global guidance for the recognition, diagnosis, and management of tumor-induced osteomalacia. J Intern Med. 2023 Mar;293(3):309-28.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10108006
http://www.ncbi.nlm.nih.gov/pubmed/36511653?tool=bestpractice.com
Physical examination
Children
Rickets occurs as a consequence of poor global mineralisation of the skeleton, and is characterised by delayed growth, bone pain, and bone deformities.[9]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
These abnormalities usually manifest between 6 months and 2 years of age. Type of deformity depends on the biomechanical situation of the extremities at the time when the structural weakness develops. Bone deformities of the forearms and posterior bowing of the distal tibia can occur in infants (due to muscle tension), whereas exaggerated physiological bowing of the legs (genu varum) is a finding in toddlers who have started walking (due to gravity pushing on the lower limbs). Older children may have valgus or windswept (valgus deformity of one leg and varus deformity of the other) deformities of the legs. Other bony deformities that may occur include knob-like projections along the ribcage (rachitic rosary), frontal bossing, and widening of the ends of the long bones, especially the wrists. Muscle traction on the softened ribcage is responsible for chest deformation leading to pectus carinatum, thoracic asymmetry, and a widening of the thoracic base. Tooth development is impaired, with delayed eruption and early dental caries. Head sweating may be evident due to increased neuromuscular activity. Infants or young children may seem irritable as a result of associated bone pain. Features of hypocalcaemia may be present as a result of inherited disorders of vitamin D metabolism or chronic untreated vitamin D deficiency. These include muscle cramps, muscle weakness, carpal pedal spasm, numbness, paraesthesias, tetany, and seizures.[88]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-37.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
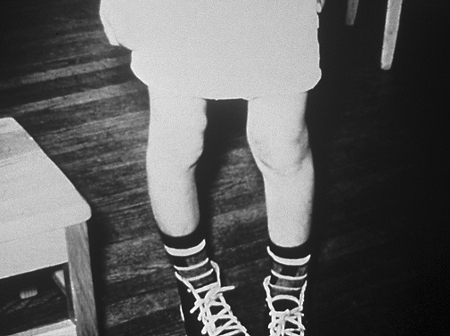
See Rickets.[Figure caption and citation for the preceding image starts]: Inward or outward bowing of the legs is a typical sign of classic ricketsCDC [Citation ends].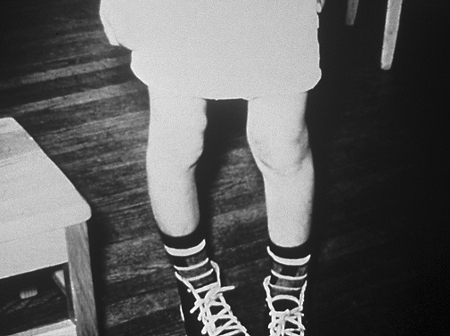
Adults
In adults with vitamin D deficiency, the growth plates are closed and there is enough mineral in the skeleton to prevent the gross skeletal deformities that are seen in children. Physical examination may reveal localised or generalised bony tenderness. Pressing with thumb or forefinger on the sternum, radius, and anterior tibia and eliciting wincing bone pain is a classic sign of periosteal bone discomfort associated with osteomalacia.[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
Pain in the hips may result in a waddling gait, and proximal muscle weakness is often seen; this is diagnosed by watching the patient get up from a sitting position with difficulty.
Laboratory investigations
The diagnosis of vitamin D deficiency and insufficiency in both adults and children is made by determining the serum 25-hydroxyvitamin D concentration.[79]Institute of Medicine. Dietary reference intakes for calcium and vitamin D. 2011 [internet publication].
https://www.nap.edu/catalog/13050/dietary-reference-intakes-for-calcium-and-vitamin-d
[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
Testing is recommended for those with symptoms of deficiency, as well as for those with an established clinical indication for vitamin D testing; for example, hypocalcaemia, osteomalacia, or following a fall.[4]Demay MB, Pittas AG, Bikle DD, et al. Vitamin D for the prevention of disease: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2024 Jul 12;109(8):1907-47.
https://academic.oup.com/jcem/article/109/8/1907/7685305?login=false
http://www.ncbi.nlm.nih.gov/pubmed/38828931?tool=bestpractice.com
[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
[81]National Institute for Health and Care Excellence. Vitamin D: supplement use in specific population groups. Aug 2017 [internet publication].
https://www.nice.org.uk/guidance/ph56
Furthermore, some clinicians also measure serum 25-hydroxyvitamin D in select people at increased risk for vitamin D deficiency.[81]National Institute for Health and Care Excellence. Vitamin D: supplement use in specific population groups. Aug 2017 [internet publication].
https://www.nice.org.uk/guidance/ph56
See History.
A 25-hydroxyvitamin D concentration of ≤50 nanomolesl/L (≤20 nanograms/mL) is typically associated with a normal serum calcium, low-normal serum phosphorus, normal or high-normal 1,25-dihydroxyvitamin D, and a high-normal or elevated intact PTH concentration.[79]Institute of Medicine. Dietary reference intakes for calcium and vitamin D. 2011 [internet publication].
https://www.nap.edu/catalog/13050/dietary-reference-intakes-for-calcium-and-vitamin-d
[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
[92]Silverberg SJ. Vitamin D deficiency and primary hyperparathyroidism. J Bone Miner Res. 2007 Dec;22 Suppl 2:V100-4.
http://www.ncbi.nlm.nih.gov/pubmed/18290710?tool=bestpractice.com
[93]Yalla N, Bobba G, Guo G, et al. Parathyroid hormone reference ranges in healthy individuals classified by vitamin D status. J Endocrinol Invest. 2019 Nov;42(11):1353-60.
http://www.ncbi.nlm.nih.gov/pubmed/31273631?tool=bestpractice.com
A 25-hydroxyvitamin D concentration between 52 and 72 nanomoles/L (21 and 29 nanograms/mL) is typically associated with a normal concentration of serum calcium and phosphorus, a normal 1,25-dihydroxyvitamin D, and usually a normal or slightly elevated intact PTH.[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
[93]Yalla N, Bobba G, Guo G, et al. Parathyroid hormone reference ranges in healthy individuals classified by vitamin D status. J Endocrinol Invest. 2019 Nov;42(11):1353-60.
http://www.ncbi.nlm.nih.gov/pubmed/31273631?tool=bestpractice.com
Measuring the serum concentration of 1,25-dihydroxyvitamin D is of no value in determining vitamin D status because it circulates at a concentration 1000 times lower than 25-hydroxyvitamin D, has a half-life of only 4 hours (compared with the 2-3 weeks for 25-hydroxyvitamin D), and secondary hyperparathyroidism enhances its production, which is the reason why patients who are vitamin D deficient can still maintain a normal serum concentration of 1,25-dihydroxyvitamin D. Many physicians who obtain a serum 1,25-dihydroxyvitamin D level find it normal and conclude that the patient cannot be vitamin D-deficient. However, this measurement is of great value in distinguishing the inherited or acquired disorders of vitamin D metabolism.[7]Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81.
http://www.ncbi.nlm.nih.gov/pubmed/17634462?tool=bestpractice.com
[94]Clements MR, Davies M, Hayes ME, et al. The role of 1,25-dihydroxyvitamin D in the mechanism of acquired vitamin D deficiency. Clin Endocrinol (Oxf). 1992 Jul;37(1):17-27.
http://www.ncbi.nlm.nih.gov/pubmed/1424188?tool=bestpractice.com
Children
A serum 25-hydroxyvitamin D concentration of <25 nanomoles/L (<10 nanograms/mL) is usually associated with overt skeletal manifestations of vitamin D-deficiency rickets.[95]Charoenngam N, Ayoub D, Holick MF. Nutritional rickets and vitamin D deficiency: consequences and strategies for treatment and prevention. Expert Rev Endocrinol Metab. 2022 Jul;17(4):351-64.
http://www.ncbi.nlm.nih.gov/pubmed/35852141?tool=bestpractice.com
[96]Rios-Leyvraz M, Thacher TD, Dabas A, et al. Serum 25-hydroxyvitamin D threshold and risk of rickets in young children: a systematic review and individual participant data meta-analysis to inform the development of dietary requirements for vitamin D. Eur J Nutr. 2024 Apr;63(3):673-95.
https://link.springer.com/article/10.1007/s00394-023-03299-2
http://www.ncbi.nlm.nih.gov/pubmed/38280944?tool=bestpractice.com
[97]Mughal MZ. Rickets. Curr Osteoporos Rep. 2011 Dec;9(4):291-9.
http://www.ncbi.nlm.nih.gov/pubmed/21968816?tool=bestpractice.com
[98]Rios-Leyvraz M, Martino L, Cashman KD. The relationship between vitamin D intake and serum 25-hydroxyvitamin D in young children: a meta-regression to Inform WHO/FAO vitamin D intake recommendations. J Nutr. 2024 Jun;154(6):1827-41.
https://www.sciencedirect.com/science/article/pii/S0022316624002347?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/38685317?tool=bestpractice.com
The serum calcium can be normal or low and the serum phosphorus is usually low-normal or low.[99]Elder CJ, Bishop NJ. Rickets. Lancet. 2014 May 10;383(9929):1665-76.
http://www.ncbi.nlm.nih.gov/pubmed/24412049?tool=bestpractice.com
The serum alkaline phosphatase and intact PTH levels are usually elevated. A child with pseudovitamin D-deficiency rickets usually has a normal 25-hydroxyvitamin D level with hypocalcaemia, hypophosphataemia, elevated alkaline phosphatase, and intact PTH levels with a low or undetectable level of 1,25-dihydroxyvitamin D. A child with vitamin D-resistant rickets has all the biochemical manifestations of pseudovitamin D-resistant rickets, with the exception that the serum 1,25-dihydroxyvitamin D is markedly elevated. Children with X-linked hypophosphataemic rickets and autosomal-dominant hypophosphataemic rickets have a normal serum 25-hydroxyvitamin D and calcium, a low level of serum phosphorus, and an inappropriately low or low-normal level of 1,25-dihydroxyvitamin D.[3]Hossein-Nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013 Jul;88(7):720-55.
http://www.mayoclinicproceedings.org/article/S0025-6196(13)00404-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23790560?tool=bestpractice.com
[9]Chanchlani R, Nemer P, Sinha R, et al. An overview of rickets in children. Kidney Int Rep. 2020 Jul;5(7):980-90.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335963
http://www.ncbi.nlm.nih.gov/pubmed/32647755?tool=bestpractice.com
Adults
For adults, there are no overt skeletal deformities because the growth plates are closed. Instead, vitamin D deficiency causes secondary hyperparathyroidism, with a normal or mildly elevated alkaline phosphatase, normal calcium, and low or low-normal fasting phosphorus. The hallmark of oncogenic osteomalacia is a low serum phosphorus level (usually 0.39 to 0.52 mmol/L [1.2 to 1.6 micrograms/dL]) and an inappropriately low-normal or low level of serum 1,25-dihydroxyvitamin D.[8]Jan de Beur SM, Minisola S, Xia WB, et al. Global guidance for the recognition, diagnosis, and management of tumor-induced osteomalacia. J Intern Med. 2023 Mar;293(3):309-28.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10108006
http://www.ncbi.nlm.nih.gov/pubmed/36511653?tool=bestpractice.com
Serum calcium and intact PTH levels are usually normal, whereas 25-hydroxyvitamin D level is low or normal.
Imaging
In asymptomatic patients, plain-film radiographs are usually unnecessary, but x-rays of the knees and wrists should be performed when rickets or osteomalacia is suspected.[88]Uday S, Högler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020 Oct;152(4):356-37.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061584
http://www.ncbi.nlm.nih.gov/pubmed/33380700?tool=bestpractice.com
Widening of the epiphyseal plate, and loss of definition of the zone of provisional calcification at the epiphyseal/metaphyseal interface, are early signs of rickets. Looser's pseudofractures, which lie perpendicular to the cortical margins with the characteristic sclerotic borders, are a pathognomonic finding in osteomalacia. Classic metaphyseal lesions also known as bucket-handle fractures can be observed at the growth plates of long bones.[95]Charoenngam N, Ayoub D, Holick MF. Nutritional rickets and vitamin D deficiency: consequences and strategies for treatment and prevention. Expert Rev Endocrinol Metab. 2022 Jul;17(4):351-64.
http://www.ncbi.nlm.nih.gov/pubmed/35852141?tool=bestpractice.com
[100]Modest JM, Sheth H, Gohh R, et al. Osteomalacia and renal osteodystrophy. R I Med J (2013). 2022 Oct 3;105(8):22-7.
http://rimed.org/rimedicaljournal/2022/10/2022-10-22-fractures-modest.pdf
http://www.ncbi.nlm.nih.gov/pubmed/36173905?tool=bestpractice.com
[101]Holick MF, Lim R, Dighe AS. Case records of the Massachusetts General Hospital. Case 3-2009. A 9-month-old boy with seizures. N Engl J Med. 2009 Jan 22;360(4):398-407.
http://www.ncbi.nlm.nih.gov/pubmed/19164191?tool=bestpractice.com
[102]Ayoub DM, Hyman C, Cohen M, et al. A critical review of the classic metaphyseal lesion: traumatic or metabolic? AJR Am J Roentgenol. 2014 Jan;202(1):185-96.
https://www.ajronline.org/doi/10.2214/AJR.13.10540
http://www.ncbi.nlm.nih.gov/pubmed/24370143?tool=bestpractice.com
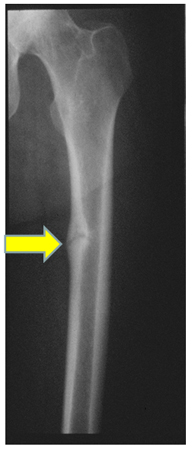
[Figure caption and citation for the preceding image starts]: X-rays of a wrist from a child with vitamin D-deficiency rickets before (left panel) and after (right panel) treatment with vitamin DFrom the collection of M.F. Holick, PhD, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a 'pseudofracture' (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a 'pseudofracture' (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].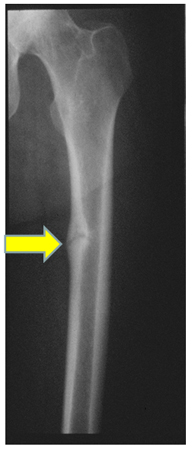
Adults with chronic vitamin D deficiency may have low bone density, leading to osteopenia and osteoporosis. A dual-energy x-ray absorptiometry (DEXA) scan should therefore be performed to assess bone density; it also aids in tracking disease progression.
 [Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a 'pseudofracture' (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a 'pseudofracture' (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD [Citation ends].