Recommendations
Key Recommendations
Assess the patient using the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach.[50]
Look for the key signs and symptoms of long bone fractures: pain, swelling, impaired function of the extremity, and guarding against limb movement. Deformity indicates a displaced fracture.
Assess and document neurological and vascular status, and repeat the assessment after the initial management, such as reduction manoeuvres or applying a splint.[51]
Signs indicating a vascular injury include:
Rapid diagnosis is crucial. If arterial injuries to the extremities are suspected, refer the patient immediately to an orthopaedic surgeon and a surgeon capable of performing nerve or vascular repair.[53]
Check for other injuries, including significant head injury. If you suspect a head injury, arrange imaging as appropriate and inform the appropriate subspecialty team. See Assessment of acute traumatic brain injury.
Assess the patient’s pain regularly. Use a pain assessment scale suitable for the person's age, developmental stage, and cognitive function. Continue to regularly assess the pain using the same scale.[17]
Assess and document any needs around safeguarding, falls risk, comorbidities, and the nature and classification of the fracture.[17]
Order plain x-rays in all patients with suspected lower limb fracture (see fracture sites in the Full recommendations section below for more on which x-rays to order).
Assess the patient for compartment syndrome. In patients with long bone fractures, compartment syndrome is seen most commonly following fractures of the tibia and forearm.[54] Key findings indicating compartment syndrome include pain out of proportion to the associated injury and pain on passive movement of the muscles of the involved compartments.[54] See Compartment syndrome of extremities.
Assess the patient using the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach.[50]
Look for the key signs and symptoms of long bone fractures; these usually manifest with pain, swelling, and impaired function of the extremity. Deformity indicates a displaced fracture. The patient may guard against any movement of the affected limb (e.g., during physical examination).
In a patient with a femoral shaft fracture:
Follow Advanced Trauma Life Support (ATLS)/Advanced Cardiac Life Support (ACLS) guidelines.[55][56]
Assess haemoglobin and type and cross-match the patient ready for possible transfusion.
Assess and document neurological and vascular status.[51]
Signs indicating a vascular injury include:
Do not exclude vascular injury based on capillary return or Doppler signal. The patient will require further investigation (such as CT angiography or standard angiography, depending on availability) or surgical exploration if any of the above signs of vascular injury persist after restoration of limb alignment and joint reduction.[52]
Repeat the assessment after the initial management, such as reduction manoeuvres or applying a splint.[51]
Assess the patient for other injuries, including significant head injury. If you suspect a head injury, arrange imaging as appropriate and inform the appropriate subspecialty team. See Assessment of acute traumatic brain injury.
Imaging
In adults with multiple injuries, and complex or open fractures, use a whole-body CT (including a vertex to toes scanogram followed by a vertex to mid-thigh CT scan).[51][52] Use the findings of this to direct further CT of the limbs.[52]
Do not routinely use whole-body CT in children under 16.[52]
Order plain x-rays in all patients with suspected lower limb fracture (see fracture sites below for more on which x-rays to order).
In addition to x-rays, and depending on the type of fracture and cause, in some patients you may consider:
Non-contrast CT MRI
Ultrasound duplex scanning
Angiography (CT or standard)
Dual-energy x-ray absorptiometry bone density scan
Triple phase bone scan.
For further information, see the fracture types in the sections below and in Investigations.
Compartment syndrome
Assess the patient for compartment syndrome. In patients with long bone fractures, compartment syndrome is seen most commonly following fractures of the tibia and forearm.[54] Clearly document:[54]
The time and mechanism of injury
Time of evaluation
Level of pain
Level of consciousness
Response to analgesia and whether a regional anaesthetic has been given.
Key findings indicating compartment syndrome include pain out of proportion to the associated injury and pain on passive movement of the muscles of the involved compartments.[54] Although the classic signs of acute compartment syndrome are loss of distal pulses, pallor, increased pain with passive stretch of tissues distal to the fracture site, paraesthesias, and poikilothermia, these signs are more often indicative of arterial ischaemia than acute extremity compartment syndrome.[57] A high index of suspicion is therefore needed.[54] Palpable pulses distal to the involved compartment do not rule out compartment syndrome. Absent pulses are usually due to systemic hypotension, arterial occlusion, or vascular injury.[54] See Compartment syndrome of extremities.
Have a high index of suspicion. The patient with acute compartment syndrome would not be expected to have most or all of these signs/symptoms, especially early in the course. Negative predictive value is high, but positive predictive value of these signs separately is low.[58]
Symptoms may evolve over time, so repeat the physical examinations and continue to monitor at-risk patients for compartment syndrome.
In patients with a fractured tibia, the National Institute for Health and Care Excellence (NICE) in the UK recommends assessing and recording clinical symptoms and signs in hospital for 48 hours after injury or fixation.[52] In practice, patients may be discharged the following day if they are comfortable.
Consider continuous compartment pressure monitoring in hospital when clinical symptoms and signs cannot be readily identified, such as in a patient in intensive care.
Advise patients how to self-monitor for symptoms of compartment syndrome when they leave hospital.[52]
Practical tip
Patients with dementia may exhibit withdrawal from attempted pressure or motion to the affected area, lack of use of the involved extremity, and non-specific signs such as decreased appetite, new or worsened incontinence, or depression.
Pathological or insufficiency fractures
Pathological or insufficiency fractures may occur at lower than normal physiological loads.[59] The patient may present with sudden onset of pain, rapid swelling, ecchymosis, and impaired function of the limb. Insufficiency fractures warrant a work-up for metabolic bone disease. Discovery of a lytic lesion or other evidence of neoplasia requires an appropriate work-up for malignancy.
In adults, if an x-ray suggests the possibility of bone sarcoma, refer the patient on a suspected cancer pathway.[60]
In children and young people (up to 24 years of age), consider a very urgent referral (for an appointment within 48 hours) for specialist assessment if an x-ray suggests the possibility of bone sarcoma. In children and young people with unexplained bone swelling or pain, consider a very urgent direct access x-ray to assess for bone sarcoma.[60]
If the fracture is unexplained, consider a diagnosis of myeloma and arrange a full blood count and blood tests for calcium and plasma viscosity or erythrocyte sedimentation rate.[60] If serum free light chain testing is not available, use a Bence-Jones test to check for free light chains contained in urine.[60] See Multiple Myeloma.
Humeral shaft fractures commonly result from direct trauma to the humerus and falls onto the outstretched hand.[23][24] Less commonly, extreme muscle contraction, electrocution injury, or seizure may lead to humeral shaft fracture.[25]
In displaced fractures, deformity is common, with the arm appearing shortened. Palpate for point tenderness and bony crepitus at the fracture site.
Perform a thorough neurovascular examination, as neurovascular compromise may occur. The radial nerve, and the brachial artery and vein are at greatest risk of compromise.
Order plain x-rays of the humerus:
Include at least two 90° orthogonal views (anteroposterior and lateral)
Ensure the films encompass the glenohumeral and elbow joints to evaluate for associated injury in these areas.
Fractures proximal to the pectoralis major insertion tend to result in the proximal fragment being internally rotated and abducted by rotator cuff forces. If the fracture is distal to the pectoralis major insertion but proximal to the deltoid insertion, the pull of the pectoralis major and arm adductors displace the proximal fragment medially, while the deltoid pulls the distal fragment laterally. Fractures distal to the deltoid insertion show abduction and flexion of the proximal fragment, with proximal displacement of the distal fragment.
Proximal humeral shaft fractures
Proximal humeral shaft fractures are typically seen in older people after a fall on the outstretched hand. Direct trauma and seizures may also lead to these fractures.[26] Most of these fractures are impacted; displacement and angulation are usually minimal. The surgical neck and greater tuberosity are the most common fracture sites.
Consider a dislocated shoulder (presenting with severe shoulder pain, swelling, and impaired range of motion) as a differential diagnosis or as an associated condition.
Deformity is uncommon unless associated dislocation is present, but swelling may make this hard to discern.
Perform a thorough examination to determine any further injury to the rest of the shoulder girdle, and consider damage to the axillary artery or circumflex humeral arteries.
Practical tip
Perform a neurovascular examination, including testing sensation over the regimental patch and deltoid motor function to assess for injury to the axillary nerve.
Order plain x-rays, including anteroposterior, axillary lateral, and scapular 'Y' views to evaluate for fracture and dislocation. If you suspect vascular injury, arrange further imaging with angiography and an orthopaedic and vascular surgery consultation.
Consider CT or MRI for definitive diagnosis of subtle fractures (non-displaced greater tuberosity fractures, sometimes even displaced lesser tuberosity fractures), for better evaluation of articular surface involvement in humeral head fractures, or for preoperative planning. Three-dimensional CT reconstruction has been advocated as a way to better visualise the exact anatomy of these injuries.[61]
Several classification systems exist for proximal humerus fractures, with the Neer system being the most widely used.[4] Newer classification systems have added articular surface orientation and other fracture characteristics.[5][6] See Classification under Aetiology.
Radial shaft fractures usually result from a fall onto an outstretched or pronated wrist, or from a direct blow.[27] Because of the deforming muscle forces that act on these fractures, they are often dorsally angulated and are inherently unstable.
The patient typically presents with pain and swelling over the mid to distal radius down into the wrist. Deformity may be noted in displaced fractures. In distal radius fractures, the classic 'dinner fork' deformity with dorsal angulation at the fracture site (resulting from dorsal displacement from falling on a pronated hand) may be noted. The fracture site and the distal radioulnar joint are tender to palpation.
Document the mechanism of injury and clinical findings, including skin integrity, assessment of circulation, and sensation.[62]
In children, assess the limb on presentation, including the status of the radial pulse, digital capillary refill time, and the individual function of the radial, median, and ulnar nerves. Administer effective analgesia and record pain scores frequently, to ensure that pain relief is maintained throughout.[63]
Order anteroposterior and lateral x-ray views, centred at the wrist, ensuring that the entire radius and ulna, along with the wrist and elbow joints, are clearly visualised.[62] In children, orthogonal x-rays should be available to allow proper diagnosis and planning.[62] Consider the type of fracture and any possible dislocation based on the fracture site and the history.
Nightstick fractures: these isolated fractures of the mid shaft of the ulna usually result from a person trying to ward off a blow from a heavy, blunt object (e.g., a night stick or truncheon).
The patient typically presents with pain and swelling over the affected area.
Point tenderness at the fracture site is noted, but deformity is uncommon.
X-rays of the radius and ulna will confirm the injury.
Monteggia fracture/dislocation: an ulnar fracture involving the proximal third of the shaft, and there may be associated dislocation of the radial head at the elbow.
These fractures are rare and usually due to a fall onto an outstretched hand, with the elbow extended and pronated.[28]
The patient presents with pain and swelling at the proximal ulna, with variable deformity depending on the exact nature of the injury.
Associated injury to the radial nerve or posterior interosseous nerves may result in abnormal sensation at the dorsum of the thumb and second and third fingers. Wrist and thumb extension may also be weak.
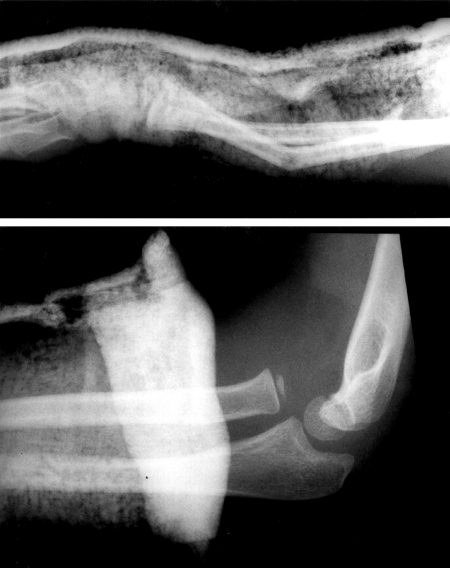
[Figure caption and citation for the preceding image starts]: Radiographs showing dislocated radial head with distal third bone forearm fracturesPeter VK, Emerg Med J 2002;19:88-9; used with permission [Citation ends].
Practical tip
For a Monteggia fracture/dislocation, request plain films, including the entire radius and ulna, along with the wrist and elbow joints. The radial head dislocation may be subtle, so it is important that the examiner closely inspects the radiographs for this injury. In the uninjured elbow, a line drawn through the axis of the proximal radial shaft and radial head (McLaughlin line) should bisect the capitellum.
Fractures at the junction of the mid and distal thirds of the shaft are often complicated by injury to the distal radioulnar joint; such injuries are often referred to as Galeazzi fractures.
Concomitant fractures of both the radius and the ulna are usually the result of high-energy trauma from a blow, fall, or motor vehicle accident.
Pain and swelling at the fracture site can be accompanied by deformity.
Injury to the radial, median, or ulnar nerves may occur, along with vascular injury.
Femoral shaft fractures are generally caused by high-energy trauma, such as a motor vehicle accident, or fall from a height.
Spiral fractures of the femoral shaft may occur as a result of a twisting injury.
Comminuted and open fractures may occur from high-energy injuries or penetrating trauma.
Perform a secondary survey (head-to-toe examination) for other signs of injury. It takes a great force to break a large bone like the femur, therefore other serious injuries are often present too.
The patient with an acute femoral shaft fracture presents with severe pain of the involved extremity and is unable to walk. The thigh may appear markedly swollen, and deformity is often present.
Manage the patient with a femoral shaft fracture using an Advanced Trauma Life Support (ATLS)/Advanced Cardiac Life Support (ACLS) approach.[55][56]
Assess haemoglobin and type and cross-match the patient ready for possible transfusion.
A large amount of blood (around 1.0-1.5 litres) can be lost into the thigh before it becomes clinically apparent. Patients can become hypotensive and go into hypovolaemic shock from these injuries.[64] An expanding haematoma indicates severe vascular injury.
Frequently monitor vital signs. Check distal pulses. They may be weak or absent, as a result of either hypotension or acute compartment syndrome.
Perform serial neurovascular examinations to monitor for signs of developing compartment syndrome.[54] See Compartment syndrome of extremities.
Once the patient has been haemodynamically stabilised (and appropriate analgesia has been given - see Management recommendations), order plain anteroposterior and lateral x-rays of the femur. These fractures are usually significantly displaced and angulated.
There are several classification systems for femoral shaft fractures. One of the most common is the Winquist-Hansen system.[9][10] See Classification under Aetiology.
Tibial shaft fractures may result from direct trauma (usually causing transverse or comminuted fractures) or indirect twisting forces (usually causing spiral or oblique fractures).[31]
In an acute tibial shaft fracture, the patient presents with severe pain and inability to bear weight. Massive swelling and ecchymosis may occur, and open fractures are relatively common.
Apply a long leg splint for protection and comfort.
Request full-length anteroposterior and lateral x-rays of the tibia and fibula (including the knee and ankle).
Consult the orthopaedic team to consider the best choice for the individual patient.[65]
The AO Foundation classification system of tibial shaft fractures is the most widely used system.[11] See Classification under Aetiology.
Check for compartment syndrome in the first 48 hours after injury in patients with a tibial fracture.[52] See Compartment syndrome of extremities.
High-energy trauma may result in simultaneous fracture of both the tibial and fibular shafts. They may occur with a twisting injury.[Figure caption and citation for the preceding image starts]: X-ray showing a segmental fracture of the tibia and fibula [Citation ends].
The patient presents with severe pain, deformity, and inability to bear weight. Massive swelling and skin wounds from fracture fragments may be noted. Acute compartment syndrome may occur, so repeated neurovascular examination is crucial.
Apply a splint and request full tibia/fibula x-rays, including the knee and ankle joints. Emergency orthopaedic consultation is required.
Isolated fibular fractures are typically caused by a direct blow to the outer aspect of the leg, or from an external rotation force at the ankle. In the latter situation, the force damages the distal tibiofibular syndesmosis, medial malleolus, and/or deltoid ligament of the ankle. The force is then transmitted proximally through the interosseous membrane and up the fibular shaft, until it exits at the proximal fibula. This is referred to as a Maisonneuve fracture. In this case, the fibular fracture itself usually heals well with conservative management, but this should serve as a warning of a severe injury to the ankle structures (which generally require operative intervention).[66] See Ankle fractures.
In a patient with a suspected fibula fracture, evaluate for additional injuries, such as tibial fracture, ligamentous injury of the knee, and ankle fractures or instability. The common peroneal nerve runs over the proximal aspect of the fibula and may be injured by a proximal fibular fracture. This may lead to a foot drop and/or paraesthesias at the lateral aspect of the leg and dorsum of the foot. Request anteroposterior and lateral x-rays of the full length of the tibia and fibula (including the knee and ankle joints). More directed radiographic evaluation of the knee or ankle is indicated if the physical examination reveals evidence of injury at these locations.
Upper limb stress fractures
Humeral stress fractures are rare and primarily occur as a result of overuse among throwing athletes. Gymnasts, weightlifters, and other athletes who place repetitive high-impact or high-torque loads on the humerus have also been known to sustain these injuries. The person typically experiences gradually progressive arm pain with activity, but the completion of the fracture can be dramatic. Severe pain, swelling, and deformity of the shaft may be accompanied by neurovascular injury, especially to the radial nerve.[67][68] As such, it is important that an athlete complaining of persistent arm soreness be evaluated for a stress fracture before completion of the fracture occurs.
Stress fractures of the radius and ulna are uncommon and primarily occur among athletes who repetitively load the bones with high forces (e.g., gymnasts).[29][30]
Femoral stress fractures
Femoral stress fractures generally have an indolent presentation. Typically the pain is felt with impact activity (e.g., running) and tends to get progressively worse over time. Pain is usually noticed in the groin or buttocks for a femoral neck stress fracture, along the thigh in a femoral shaft stress fracture, and around the knee in a distal femoral stress fracture.
Some counterintuitive data have suggested that bisphosphonate use may actually increase the risk of femoral shaft stress or insufficiency fracture, while decreasing the risk of other fractures.[69][70]
Observe the patient’s gait. A patient with a femoral stress fracture may have an antalgic gait, but gross inspection of the hip and thigh is usually unremarkable.
Perform a musculoskeletal examination:
A fulcrum test (levering the femoral shaft over the examiner's forearm, which is placed underneath the femoral shaft) may reproduce symptoms in a femoral neck or proximal shaft stress fracture.
Internal rotation of the hip often reproduces pain in a patient with a femoral neck stress fracture.
A hop test (hopping on one or both legs) usually produces pain as well.
Maintain a high index of suspicion for these injuries, as the finding on examination may be subtle.[71]
Practical tip
Palpation rarely causes tenderness, although vague tenderness over the thigh may sometimes be mistaken for evidence of a muscle strain.
A patient suspected of having a femoral neck stress fracture should be made non-weight bearing immediately. Refer the patient for urgent x-rays of the hip and proximal femur.
If the films reveal a tension side fracture, a frank fracture line, or a displaced fracture, arrange an urgent orthopaedic referral for consideration of operative intervention.
If the films reveal sclerosis at the compression side, consider following up the patient with serial radiographs and having them progress to partial then full weight bearing as tolerated. Seek advice from an orthopaedic consultant.
If the films are negative (common early on in the evolution of the fracture), an MRI can be used to detect the fracture.
If the x-rays are negative but the MRI is positive, conservative management is reasonable. Full return to impact activity can take several months.[72]
Evaluate bone mineral density in patients suspected of having osteopenia/osteoporosis using dual-energy x-ray absorptiometry [DXA] scanning. However, if the DXA scan measures the femoral neck after bony healing has occurred, a falsely normal or even high bone mineral density may be reported. Thus, the contralateral femoral neck should be used for the DXA if possible.
Tibial and fibular stress fractures
Stress fractures of the tibia are relatively common in impact athletes, such as runners and basketball players, and in military personnel.[32][33]
They generally present with gradually progressive pain with impact and weight-bearing activities. Eventually, they may also cause pain at rest. They most commonly occur at the posteromedial tibial border, with anterior tibial crest stress fractures occurring less often.
Inspection is usually unremarkable, but palpation reveals point tenderness at the fracture site. A healing stress fracture may be evinced by a palpable callus. Pain upon tuning fork vibration in the area of the fracture is felt to be fairly specific but not very sensitive. Pain is reproduced by having the patient jog, hop, or, in more severe cases, walk.
Stress fractures of the fibula are uncommon but typically occur in runners and ballet dancers.
Imaging in stress fractures
MRI and triple phase bone scan (TPBS) are much more sensitive for early detection of stress fractures than x-rays. MRI is generally the preferred choice. It is much more specific than TPBS, does not expose the patient to ionising radiation, and provides additional information about the surrounding tissues.[73] MRI allows for more specific evaluation of marrow oedema and the surrounding soft tissue, which helps in the diagnosis of any intra-articular pathology.
X-rays may be negative early in the course of the injury. In a tibial stress fracture, x-rays later tend to show periosteal thickening, sclerosis, and callus formation. With anterior tibial stress fractures, x-rays may reveal the 'dreaded black line', a horizontal radiolucency in the anterior tibial cortex. These injuries tend to heal more slowly than the more common posteromedial stress fractures, and they have a higher rate of non-union.[74]
Use of this content is subject to our disclaimer