Investigations
1st investigations to order
oesophagogastroduodenoscopy
Test
Oesophagogastroduodenoscopy (OGD) is the initial diagnostic test of choice to visually assess the oesophagus. OGD should be ordered in all patients with suspected eosinophilic oesophagitis (EoO).[2][3]
Endoscopic signs are non-specific (and not formally part of the diagnostic criteria), but can be highly suggestive of EoO.[1] The US guidelines recommend using endoscopic scoring system (e.g., EoO Endoscopic Reference Score) to quantify macroscopic abnormalities at every endoscopy.[3][82] The EoO Endoscopic Reference Score accounts for the five most typical EoO endoscopic features: oedema, rings, exudates, furrows, and strictures.[84]
Endoscopy can appear normal in a number of patients (most commonly children).[82][Figure caption and citation for the preceding image starts]: Endoscopic findings including white plaques, linear furrows, and oedemaFrom the collection of Dr Evan S. Dellon [Citation ends]. [Figure caption and citation for the preceding image starts]: Endoscopic findings including oesophageal rings, linear furrows, oedema, mild white plaques, and narrowingFrom the collection of Dr Evan S. Dellon [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopic findings including oesophageal rings, linear furrows, oedema, mild white plaques, and narrowingFrom the collection of Dr Evan S. Dellon [Citation ends].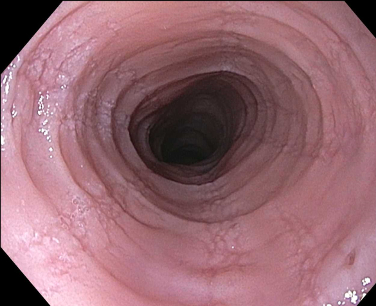
Result
fixed oesophageal rings; focal oesophageal strictures; diffuse oesophageal narrowing; oedema or congestion of the mucosa with loss of normal vascular markings; linear furrows; white plaques or exudates (which correlate with the histological finding of eosinophilic microabscesses); crêpe-paper mucosa (mucosa fragility where the oesophageal mucosa tears from insufflation or passage of the scope); may be normal in some cases
oesophageal biopsy
Test
Biopsies are obtained during oesophagogastroduodenoscopy. At least six endoscopic biopsies from two oesophageal levels are recommended.[3][82] Eosinophilic infiltrate in eosinophilic oesophagitis (EoO) is patchy, and an increasing number of biopsies maximises diagnostic sensitivity.[3][86][87][88][89][90] The American College of Gastroenterology (ACG) recommends quantifying eosinophil counts on oesophageal biopsies from every endoscopy.[3]
If a patient presents with food bolus obstruction, sufficient biopsies should be taken at the time of endoscopy to ensure a diagnosis of EoO is not missed - if the obstruction has spontaneously cleared or insufficient diagnostic biopsies have been obtained at the index endoscopy, elective endoscopy should be arranged before discharge.[2]
Recommendations in the UK also specify that biopsies be taken from targeted (taken from visibly abnormal areas) and non-targeted areas.[2]
On histological examination, the convention is to quantify the peak eosinophil count in the most inflamed area of the oesophageal epithelium.[1][3] The standard size of a high-power field is 0.3 mm², and UK guidelines recommend an updated peak eosinophil count of ≥15 per 0.3 mm² is used.[2]
Other supporting histological features include basal zone hypertrophy, lamina propria fibrosis, surface layering of eosinophils, eosinophil degranulation, and eosinophil microabscesses.[91] These, and several other features, have been developed into an EoO Histological Scoring System (HSS).[91][Figure caption and citation for the preceding image starts]: Oesophageal biopsy showing a diffuse eosinophilic epithelial infiltrate as well as basal cell hyperplasia and spongiosisFrom the collection of Dr Evan S. Dellon [Citation ends]. UK guidelines recommend that concomitant histological features be included in the histological description, with the peak eosinophil count, to aid diagnosis of EoO.[2]
UK guidelines recommend that concomitant histological features be included in the histological description, with the peak eosinophil count, to aid diagnosis of EoO.[2]
Result
peak eosinophilic count ≥15 eosinophils per high-power microscopy field (or ≥15 eosinophils per 0.3 mm²); concomitant features, including basal cell hyperplasia, oedema (sponginosis), eosinophil microabscesses, layering and degranulation, and subepithelial sclerosis, may be present
FBC with differential
Test
A mild to moderate peripheral eosinophilia may be seen in eosinophilic oesophagitis.
Grossly raised peripheral eosinophil count is rarely seen and suggests the patient should be evaluated for other systemic causes.
Result
may show peripheral eosinophilia
Investigations to consider
barium swallow (oesophagram)
Test
Consider in paediatric patients presenting with dysphagia to assess potential fibrostenotic disease.[3][79] In particular, it is recommended that a barium swallow is performed before dilation if the anatomy or calibre of the oesophagus cannot be clearly defined by oesophagogastroduodenoscopy.[79]
Result
determine length of oesophageal strictures; evaluate the severity of narrow calibre oesophagus; determine oesophageal anatomy
Emerging tests
unsedated transnasal endoscopy
Test
A less invasive method that can be used particularly in children for sampling the oesophagus. In two small studies, it has been well-tolerated with only topical anaesthetic in both children and adults. Studies have found that it is safe, well-tolerated, and can provide the endoscopic and histological measures to assess response.[92][93][94] Combining it with virtual reality distraction may facilitate more efficient diagnosis and treatment of eosinophilic oesophagitis (EoO).[95][96]
Result
endoscopic signs of EoO
oesophageal string test
Test
Minimally invasive oesophageal sampling technique where a capsule containing a string is swallowed, and the string that is attached to the capsule is held outside of the mouth.[3] The capsule dissolves and the string remains in the oesophagus where it absorbs inflammatory factors related to eosinophilic oesophagitis.
After an hour, the string is removed and sent to a specialised laboratory where the inflammatory factors can be measured.
Initial studies showed that these factors correlate extremely well with the same factors measured in oesophageal biopsies, and further work indicates the oesophageal string test may provide a safe and minimally invasive way of disease monitoring.[97][98]
Result
elevated levels of eosinophil granule protein and other inflammatory factors
cytosponge
Test
Minimally invasive oesophageal sampling technique where a capsule containing a sphere-shaped cytology mesh (sponge) is swallowed, and an attached string retained outside of the mouth.
After 5 minutes, the capsule dissolves, which releases the sponge, and the string is used to pull the sponge through the oesophagus where it collects a tissue sample before it is removed from the mouth.[3] The sample can then be assessed for levels of oesophageal eosinophils in a standard pathology laboratory.
One preliminary study showed excellent correlation between the eosinophil levels in the sponge sample and in matched endoscopic biopsy samples.[99] Studies indicate that cytosponge is a safe, well tolerated, and accurate way to assess histological activity, but the findings need to be validated in larger studies.[100][101]
Result
increased levels of oesophageal eosinophils
oesophageal physiological testing
Test
Several studies have shown that mucosal impedance is lower in eosinophilic oesophagitis (EoO) than in other oesophageal conditions such as erosive and non-erosive reflux disease and achalasia, and that this low impedance is seen throughout the entire oesophagus.[63][65][102]
A minimally invasive approach to measurement of mucosal impedance is not currently available.
UK guidelines recommend oesophageal physiological testing for patients with EoO who remain symptomatic even though they have received appropriate treatment, have no evidence of fibrostenotic disease at endoscopy and are in histological remission.[2]
Result
lower impedance pattern is suggestive of EoO
eosinophilic oesophagitis (EoO) diagnostic panel
Test
A 94-gene expression panel that uses a single oesophageal biopsy to yield a summary gene expression score. This score has been shown to discriminate EoO cases from non-EoO controls (including patients with GORD) with a high degree of accuracy.[60][103]
This test is currently being commercialised and ongoing studies are evaluating the role of this test in diagnostic algorithms.
Result
gene expression score suggestive of EoO
Use of this content is subject to our disclaimer