Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- evidence or history of trauma
- focal neurological deficit
- headache
- signs of raised intracranial pressure (ICP)
- abnormal pupillary reflexes
Other diagnostic factors
- loss of consciousness/decreased alertness
- cognition changes
- dysphasia
- seizure
- loss of bowel and bladder continence
- localised weakness
- sensory changes
- otorrhoea
- rhinorrhoea
Risk factors
- recent trauma
- coagulopathy and anticoagulant use
- advanced age (>65 years)
- excessive alcohol use
- intracranial hypotension (e.g., secondary to cerebral shunt or cerebrospinal fluid [CSF] leak)
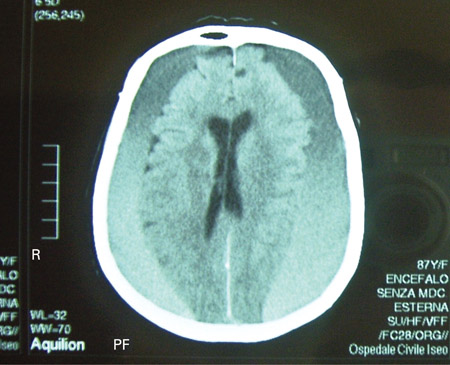
Diagnostic investigations
Treatment algorithm
Contributors
Authors
Christopher P. Robinson, DO, MS
Associate Professor of Neurology and Neurosurgery
Division of Neurocritical Care
Vice Chair of Clinical Operations
Neurology Clerkship Director
University of Florida College of Medicine
Florida
FL
Disclosures
CPR has received compensation for serving as an expert witness.
Acknowledgements
Dr Christopher P. Robinson would like to gratefully acknowledge Dr Andrew W. Grande, Dr Stephen J. Haines, Dr Praveen R. Baimeedi, Dr Jason S. Hauptma, and Dr Neil A. Martin, previous contributors to this topic.
Disclosures
AWG, SJH, PRB, JSH, and NAM declare that they have no competing interests.
Peer reviewers
Nathan J. Ranalli, MD
Resident
Department of Neurosurgery
University of Pennsylvania School of Medicine
Philadelphia
PA
Disclosures
NJR declares that he has no competing interests.
Marek Ma, MD
Instructor
Emergency Medicine
Department of Emergency Medicine Administrative Offices
University of Pennsylvania
Philadelphia
PA
Disclosures
MM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Expert Panel on Neurological Imaging; Shih RY, Burns J, Ajam AA, et al. ACR Appropriateness Criteria® head trauma: 2021 update. J Am Coll Radiol. 2021 May;18(5S):S13-36.Full text Abstract
American College of Surgeons. Best practice guidelines: the management of traumatic brain injury. 2024 [internet publication].Full text
National Institute for Health and Care Excellence. Head injury: assessment and early management. May 2023 [internet publication].Full text
Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury, Fourth Edition. Neurosurgery. 2017 Jan 1;80(1):6-15.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available here.
Use of this content is subject to our disclaimer