Investigations
1st investigations to order
high-resolution CT cervical spine
Test
Request an urgent high-resolution CT scan of the cervical spine in any patient who:[14][27]
Has an altered level of consciousness (Glasgow Coma Scale [GCS] <12 on initial assessment)
The patient has been intubated
A definitive diagnosis of C-spine injury is needed urgently (e.g., C-spine manipulation needed for surgery/anaesthesia)
There has been blunt polytrauma involving the head and chest, abdomen or pelvis in someone who is alert and stable
There is clinical suspicion of C-spine injury and any of:
Age 65 or over
Dangerous mechanism of injury
Focal peripheral neurological deficit
Paraesthesia in upper or lower limbs
Is identified by the Canadian C-spine rule as having:[13]
A high-risk factor for cervical spine injury
A low-risk factor for cervical spine injury AND they are unable to actively rotate their neck 45 degrees to both left and right.
[Figure caption and citation for the preceding image starts]: Canadian C-spine rule. A&E, accident and emergency department; GCS, Glasgow Coma Scale; MVC, Motor vehicle collision. ✝Adapted from Stiell IG, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001 17;286(15):1841-8. [Citation ends].
The UK’s National Institute for Health and Care Excellence recommends CT scanning first line in adults who are identified by the Canadian C-spine rule as requiring imaging.[14] Request a thin slice (2-3 mm) helical CT scan from the base of the skull (occiput) to at least all of T4 with both sagittal and coronal reconstructions.[27]
The CT scan should be performed within 1 hour of being requested to the radiology team or when the patient is sufficiently stable.[14] CT images should be interpreted immediately by a healthcare professional trained in this area (e.g., senior musculoskeletal radiologist).[13]
Consult with a neurosurgeon or spinal surgeon over any abnormalities on the CT cervical spine scan.[14]
[Figure caption and citation for the preceding image starts]: Common fracture patterns with severe cervical spine trauma. Top: axial CT image showing a cervical burst fracture at C5 level. Bottom: axial CT showing fracture dislocation at C6-C7 level.From the personal collection of Michael G. Fehlings [Citation ends].
Practical tip
Common cervical spine injuries include:
Odontoid fractures (common in older people)
Vertebral body compression/burst fractures
Hangman fractures (common in extension type injuries)
Bilateral facet dislocation (can occur in flexion type injuries)
[Figure caption and citation for the preceding image starts]: CT reconstruction demonstrating undisplaced odontoid fractureFrom the personal collection of Michael G. Fehlings [Citation ends].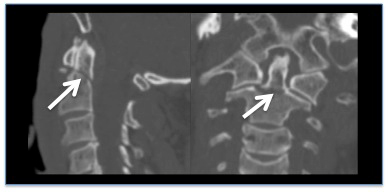
Practical tip
The risk of missing a cervical spine injury after a normal CT cervical spine is very low.[32]
Result
may show cervical spine vertebral misalignment, fracture, and pre-vertebral soft-tissue swelling
Investigations to consider
CT whole spine
Test
If a cervical spine injury or a fracture is identified, a CT scan of the whole spine is indicated to identify a concomitant thoracolumbosacral fracture.[13] See our topic Thoracolumbar spine trauma.
Result
may be normal; may show a concomitant thoracolumbosacral fracture
MRI cervical spine
Test
Refer urgently to a neurosurgeon or spinal surgeon any patient with clinical signs of a spinal cord injury (i.e., an abnormal neurological exam). An MRI of the spine is indicated (in addition to the CT) in these patients.[13][27]
[Figure caption and citation for the preceding image starts]: Common fracture patterns with severe cervical spine trauma. Top row: cervical burst fracture at C5 level. Top left: axial CT image showing a fracture of C5 vertebral body. Top right: mid-sagittal T2-weighted MRI showing retropulsion of the body of C5 with spinal cord compression, T2-weighted signal changes within the spinal cord, and T2-weighted signal changes within the posterior ligamentous complex indicating disruption of these ligaments. Bottom row: fracture dislocation C6-C7 level. Bottom left: axial CT through C6/C7 facet level. Bottom right: T2-weighted mid-sagittal MRI demonstrating spinal cord compression and T2-weighted signal change within the spinal cordFrom the personal collection of Michael G. Fehlings. [Citation ends].
Result
may show cervical disc herniation, anterior or posterior ligament disruption, cord compression, spinal canal compromise, and intramedullary T1- and/or T2-weighted hyperintensity and/or hypointensity
Use of this content is subject to our disclaimer