Differentials
Common
Sinus tachycardia
History
fever or other signs of infection; weight loss and/or agitation (suggestive of hyperthyroidism); causes of anxiety or stress; fatigue or malaise (suggestive of anaemia); drug use history; medication use and dosage changes; orthostatic symptoms (volume depletion); if palpitations are felt, they have a gradual onset and gradual resolution; postural orthostatic tachycardia syndrome (POTS) is characterised by an exaggerated heart rate and orthostatic symptoms in response to postural change, in the absence of orthostatic hypotension and cardiac causes of sinus tachycardia
Exam
regular tachycardic pulse; skin pallor (anaemia); lid lag, warm smooth skin (hyperthyroidism); hypotension or orthostasis (volume depletion); normal cardiac examination
1st investigation
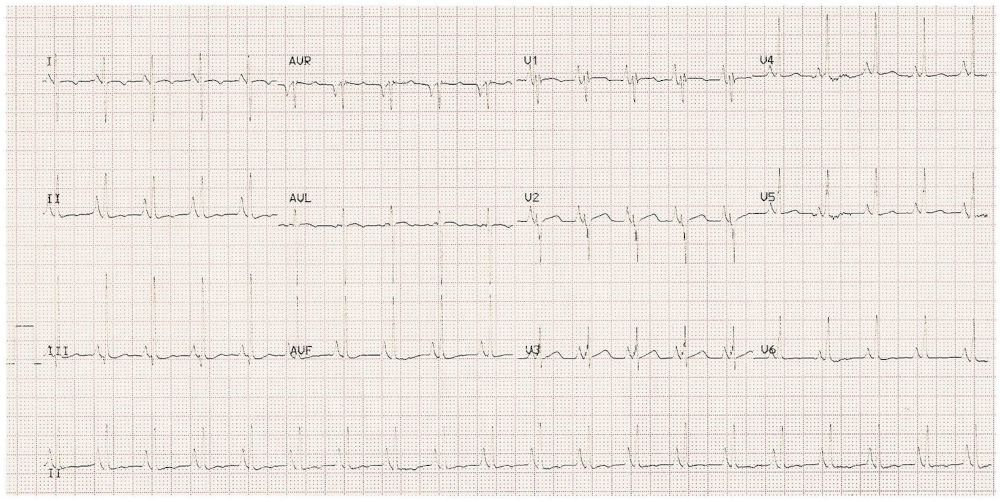
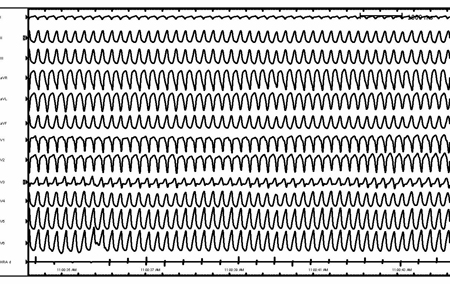
- 12-lead ECG:
regular narrow-complex tachycardia (heart rate >100 bpm); P wave before every QRS complex
More
Other investigations
- FBC:
leukocytosis if there is an infection; low Hb in anaemia
- TSH:
low in primary hyperthyroidism
- urea/creatinine ratio:
elevated urea/creatinine ratio with volume depletion
- urine and blood toxicology:
positive if drug use is the aetiology; may be negative in the case of withdrawal (such as with alcohol)
Acute atrial fibrillation
History
often asymptomatic but history can include irregular palpitations, malaise, fatigue, chest pain, or dyspnoea; may have history of alcohol misuse, use of stimulants or illicit stimulants, use of omega-3-acid ethyl esters in patients treated for hypertriglyceridaemia, hyperthyroidism, pulmonary embolism, heart failure, lung disease, hypertension, or diabetes
Exam
normal physical examination in the absence of other concomitant pathologies, except for the presence of an irregularly irregular pulse; signs of heart failure, lung disease, hyperthyroidism, hypertension, or diabetes may be found
1st investigation
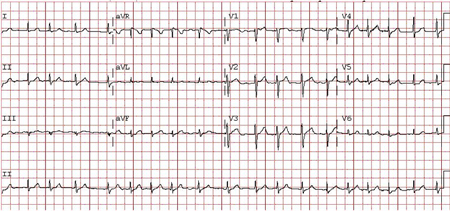
- 12-lead ECG:
P waves absent with an irregular ventricular rate
More
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
More - TSH:
low with hyperthyroidism
- urine and blood toxicology:
positive if drug use is the aetiology
- cardiac biomarkers:
positive with recent or ongoing atrial or ventricular ischaemia
Chronic atrial fibrillation
History
history can include palpitations, shortness of breath, fatigue, chest pain, dizziness, and stroke; due to rapidity of ventricular response, cerebral hypoperfusion can result in pre-syncope; may be asymptomatic; may have history of hypertension, coronary artery disease, congestive heart failure, rheumatic valvular disease, alcohol misuse, hyperthyroidism, or recent cardiothoracic surgery
Exam
normal physical examination in the absence of other concomitant pathologies, except for the presence of an irregularly irregular pulse; signs of heart failure, lung disease, hyperthyroidism, hypertension, or diabetes may be found
1st investigation
- 12-lead ECG:
P waves absent with an irregular ventricular rate
More
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
More - TSH:
low with hyperthyroidism
- urine and blood toxicology:
positive if drug use is the aetiology
- cardiac biomarkers:
positive with recent or ongoing atrial or ventricular ischaemia
Atrial flutter
History
palpitations, dyspnoea, fatigue, chest discomfort, or worsening exercise tolerance, or symptoms of heart failure; history of congenital heart disease; previous heart surgery; structural heart disease
Exam
normal physical examination except for a rapid pulse (usually regular, but can be irregular with AV block); suggestive of heart failure: jugular venous distension, lung crackles, and lower-extremity oedema; hypotension in the context of rapid atrial flutter may provoke more urgent cardioversion
1st investigation
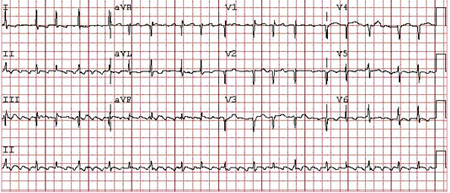
- 12-lead ECG:
typical atrial flutter characterised by regular narrow-complex tachycardia with regular sawtooth flutter waves best seen in leads II, III, aVF (type 1 flutter), atrial rates 240 to 340 bpm with ventricular rates most commonly 150 bpm (2:1 conduction); atypical atrial flutter characterised by flutter-wave morphology without the characteristic sawtooth pattern
More
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
Atrial tachycardia
History
sudden-onset palpitations, dizziness, dyspnoea, lightheadedness, or chest pressure or tightness; may have symptoms of infection or hyperthyroidism; may be on digoxin; may have taken stimulants
Exam
normal physical examination except for a rapid pulse (if the rhythm is occurring at that time); no orthostatic hypotension
1st investigation
- 12-lead ECG:
regular narrow-complex tachycardia (rate 100-250 bpm); an abnormal P-wave axis suggests an ectopic atrial focus; at faster rates there may be variable AV block
More
Other investigations
- serum digitalis level:
elevated if digitalis toxicity
More - TSH:
low in primary hyperthyroidism
- serum potassium:
low level can exacerbate atrial tachycardia
- toxicology screen:
stimulants such as cocaine can cause atrial tachycardia
AV nodal re-entrant tachycardia
History
episodic tachycardia with abrupt onset and termination; can be associated with symptoms of chest discomfort, dyspnoea, dizziness, or anxiety; in the differentiation between narrow-complex regular tachycardias, a sensation of a regular rapid pounding in the neck is highly suggestive of AV node re-entry
Exam
normal physical examination except for a rapid regular pulse
1st investigation
- 12-lead ECG:
regular narrow-complex tachycardia (rate 150-250 bpm) without apparent P waves before each QRS complex; a retrograde P wave may be seen negative in the inferior leads
More
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
AV re-entry tachycardia/Wolff-Parkinson-White syndrome
History
episodic tachycardia with abrupt onset and termination; can be associated with symptoms of chest discomfort, dyspnoea, dizziness, syncope, or anxiety
Exam
normal physical examination except for a rapid regular pulse; suggestive of secondary cardiomyopathy: S3 gallop, right ventricular (RV) heave, laterally displaced point of maximal impulse, and other signs of heart failure (elevated jugular venous pressure, lung crackles, lower-extremity oedema)
1st investigation
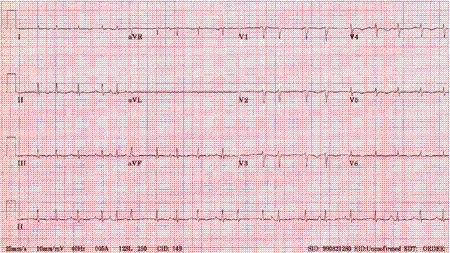
- 12-lead ECG:
when in sinus rhythm, a short PR interval with a delta wave, secondary ST-T changes, and a wide QRS complex is the classic Wolff-Parkinson-White (WPW) pattern; if this finding is associated with palpitations, it is called WPW syndrome; a bypass tract that conducts retrograde only is called a concealed bypass tract and will have a sinus-rhythm ECG with a normal PR interval, narrow QRS, and no pre-excitation (i.e., no delta wave at baseline)
More
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
More
Multifocal atrial tachycardia
History
patients may report palpitations and malaise; history of pulmonary disease is highly suggestive of multifocal atrial tachycardia (MAT)
Exam
rapid irregular pulse; signs of pulmonary disease or hypoxia
1st investigation
- 12-lead ECG:
narrow-complex tachycardia with at least 3 discrete P-wave morphologies
More
Other investigations
- chest x-ray:
signs of obstructive pulmonary disease
More - serum potassium:
low level can predispose to MAT
- serum magnesium:
low level can predispose to MAT
- serum creatinine:
elevated; chronic renal failure can predispose to MAT
Junctional ectopic tachycardia
History
postoperative junctional ectopic tachycardia (JET) is commonly seen following cardiac surgery and may at times lead to haemodynamic compromise due to the loss of A-V synchrony; congenital JET usually presents within the first 4 weeks of life and manifests with symptoms of heart failure; the tachycardia usually has a gradual onset or 'warm up' pattern
Exam
often a regular rapid pulse; intermittent cannon A waves can be seen with atrioventricular dissociation in either type of JET; congenital JET can have physical signs of congestive heart failure due to tachycardia-mediated cardiomyopathy within the first 4 weeks of life
1st investigation
- 12-lead ECG:
narrow-complex QRS morphology similar to baseline with gradual QRS acceleration beyond the sinus rate; may have intermittent atrial capture beats
Other investigations
- transthoracic echocardiography:
depressed left ventricular systolic function
- chest x-ray:
cardiomegaly or pulmonary congestion
Monomorphic ventricular tachycardia with prior myocardial infarction
History
history of significant coronary artery disease or structural heart disease; symptoms are abrupt in onset or termination, and can be mild (such as dizziness, diaphoresis, dyspnoea, palpitations) or more severe, including syncope, angina, or cardiogenic shock
Exam
rapid regular pulse, often with variable intensity depending on the degree of atrioventricular (AV) dissociation; during haemodynamically tolerated slow VT, cannon A waves, resulting from AV dissociation, are highly suggestive of ventricular tachyarrhythmia; examine for signs of heart failure (right ventricular heave, laterally displaced point of maximal impulse, increased jugular vein pressure, S3 gallop, lung crackles, peripheral oedema, ascites), which may predispose the patient to VT
1st investigation
- 12-lead ECG:
presence of AV dissociation; intermittent fusion or capture beats, concordance in the precordial leads and an initial R wave or a positive complex in lead aVR is highly suggestive of ventricular tachycardia; in sinus rhythm, Q waves or ST-segment changes suggestive of ischaemia or injury
More
Other investigations
- transthoracic echocardiography:
depressed left ventricular systolic function or wall motion abnormalities can be seen
- serum potassium:
hypo- or hyperkalaemia can predispose to VT
- serum magnesium:
hypomagnesaemia can predispose to VT
- cardiac biomarkers:
elevated with new ischaemia or infarction
- exercise stress testing:
may indicate ischaemia
More - event monitor:
intermittent tachyarrhythmias
More - electrophysiological studies:
can demonstrate dissociation between atrial and ventricular depolarisation in addition to localisation of its origin
More
Monomorphic ventricular tachycardia with non-ischaemic cardiomyopathy
History
symptoms are abrupt in onset or termination; intermittent palpitations can be associated with dizziness, diaphoresis, or dyspnoea; may be triggered by emotional stress or exercise; symptoms suggestive of ischaemic heart disease
Exam
rapid regular pulse, often with variable intensity depending on the degree of AV dissociation; during haemodynamically tolerated slow VT, cannon A waves, resulting from AV dissociation, are highly suggestive of ventricular tachyarrhythmia
1st investigation
- 12-lead ECG:
wide-complex monomorphic tachycardia (rate commonly 140-180 bpm) with evidence of AV dissociation; no ischaemic changes present
More
Other investigations
- transthoracic echocardiography:
may demonstrate cardiomyopathy
More - TSH:
can be elevated or low because both hyper- and hypothyroidism can result in non-ischaemic cardiomyopathy
- serum potassium:
hypo- or hyperkalaemia can predispose to VT
- serum magnesium:
hypomagnesaemia can predispose to VT
- exercise stress testing:
may induce ventricular tachyarrhythmias or demonstrate underlying ischaemia
- event monitor:
intermittent tachyarrhythmias
More - electrophysiological studies:
presence of inducible VT, multiple VT morphologies, fractionated diastolic electrograms during VT, or regions of low amplitude and prolonged duration suggest arrhythmogenic right ventricular cardiomyopathy (versus idiopathic right ventricular tachycardia)
More
Ventricular fibrillation
History
often seen, but not limited to, patients with associated ischaemic heart disease and ongoing ischaemia; associated with rapid haemodynamic collapse and syncope; may have recent history of progressive angina, previous cardiac arrest, severe valvular disease, or depressed left ventricular systolic function
Exam
pulse absent; dramatic haemodynamic collapse and loss of consciousness
1st investigation
- 12-lead ECG:
rapid dysmorphic irregular rhythm without clear QRS morphologies
More
Other investigations
- serum potassium:
hypo- or hyperkalaemia can predispose to VT
- serum magnesium:
hypomagnesaemia can predispose to VT
- cardiac biomarkers:
elevated with new ischaemia
- toxicology screen:
screen for cocaine or serum levels of antiarrhythmics
- transthoracic echocardiography:
may show depressed systolic function or wall-motion abnormalities suggestive of ischaemia or infarction
- coronary angiography:
coronary artery disease
More - electrophysiological studies:
presence of inducible VT or VF can help identify higher risk patients
More
Polymorphic ventricular tachycardia with normal QT interval
History
dizziness, diaphoresis, dyspnoea, palpitations, syncope, and angina; a family history of juvenile sudden death or stress-induced syncope should raise suspicion for catecholaminergic polymorphic VT
Exam
peripheral pulses may have variable intensity depending on degree of AV dissociation; often associated with severe hypotension; cannon A waves, also resulting from AV dissociation, are highly suggestive of ventricular tachyarrhythmia
1st investigation
- 12-lead ECG:
wide-complex tachycardia with continuously varying QRS morphology; baseline ECG with a normal QT interval
More
Other investigations
- TSH:
normal
- serum potassium:
hypo- or hyperkalaemia can predispose to VT
- serum magnesium:
hypomagnesaemia can predispose to VT
- cardiac biomarkers:
positive cardiac biomarkers with new ischaemia
- toxicology screen:
screen for cocaine, digitalis levels, and serum levels of tricyclic antidepressants
- transthoracic echocardiography:
may show depressed systolic function or wall-motion abnormalities suggestive of ischaemia or infarction
- exercise stress testing:
positive with catecholaminergic VT or can demonstrate ischaemia
- genetic screening:
can provide a diagnosis or help with familial screening for inherited mutations (such as mutations in genes for the cardiac ryanodine receptor or calsequestrin 2 in catecholaminergic VT)
Idiopathic ventricular tachycardia: structurally normal heart
History
intermittent palpitations that can be associated with dizziness, diaphoresis, or dyspnoea; may be triggered by emotional stress, exercise, caffeine intake, and menstrual variation; attention to symptoms that suggest ischaemic heart disease; often seen in postoperative states or after an acute coronary event followed by reperfusion
Exam
peripheral pulses are regular and may have variable intensity depending on degree of AV dissociation; cannon A waves are also due to AV dissociation and are highly suggestive of ventricular tachyarrhythmia
1st investigation
- 12-lead ECG:
wide-complex monomorphic tachycardia (rate commonly 90-120 bpm) with evidence of AV dissociation; no ischaemic changes present
More
Other investigations
- transthoracic echocardiography:
normal
- TSH:
normal
- serum potassium:
normal
- serum magnesium:
normal
- exercise stress testing:
may induce ventricular tachyarrhythmias during or after exercise, or demonstrate underlying ischaemia
More - event monitor:
can record intermittent tachyarrhythmias
Uncommon
Sinus node re-entry tachycardia
History
rarely symptomatic, though patients may report intermittent rapid palpitations with abrupt onset or termination
Exam
normal physical examination, though the patient may have a rapid regular pulse
1st investigation
- 12-lead ECG:
abrupt onset of narrow-complex tachycardia (rate 100-150 bpm) with P-wave morphology similar to baseline
More
Other investigations
Inappropriate sinus tachycardia
History
often asymptomatic; symptoms can include palpitations, fatigue, exercise intolerance, anxiety, or panic attacks; no history suggestive of hyperthyroidism, infection, anaemia, volume depletion
Exam
normal physical examination except for a rapid pulse; specific attention to rule out causes of secondary sinus tachycardia such as hyperthyroidism, infection, anaemia, volume depletion (test for orthostatic hypotension)
1st investigation
- 12-lead ECG:
regular narrow-complex tachycardia (heart rate >100 bpm); P-wave morphology is the same as sinus rhythm.
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
- 24-hour Holter monitor:
elevated heart rate at rest, exaggerated heart rate elevation for degree of exertion, no change in P-wave morphology
- TSH:
normal
- FBC:
normal
Permanent junctional reciprocating tachycardia
History
asymptomatic, though may present with palpitations or symptoms secondary to tachycardia-mediated cardiomyopathy, including malaise, oedema, and dyspnoea
Exam
normal physical examination, may have a rapid regular pulse; assess for impaired left ventricular systolic function, which may suggest a tachycardia-mediated cardiomyopathy with S3 gallop, right ventricular heave, laterally displaced point of maximal impulse, or other signs of heart failure (elevated jugular venous pressure, lower-extremity oedema)
1st investigation
- 12-lead ECG:
narrow-complex tachycardia (rate 120-200 bpm); negative P waves in the inferior leads, with a long RP interval due to slow retrograde atrial activation; usually initiated by a premature atrial contraction
Other investigations
- transthoracic echocardiogram:
rules out structural heart disease
Torsades de pointes
History
may report intermittent palpitations, syncope, seizures, or cardiac arrest; may have family history of juvenile sudden death and/or a history of using QT-prolonging medication; aetiology usually secondary to either congenital or acquired QT interval prolongation
Exam
variable peripheral pulse intensity and cannon A waves, resulting from AV dissociation, though often no pulse is palpable given haemodynamic compromise; sensorineural deafness is associated with Jervell and Lange-Nielsen syndrome (autosomal recessive long-QT syndrome); neurological examination may show focal deficits or other causes for elevated intracranial pressure
1st investigation
- 12-lead ECG:
wide-complex tachycardia with continuously varying QRS morphology; baseline ECG with a wide QT interval
More
Other investigations
- TSH:
normal
- serum potassium:
hypo- or hyperkalaemia can predispose to VT
- serum magnesium:
hypomagnesaemia can predispose to VT
- cardiac biomarkers:
positive cardiac biomarkers with new ischaemia
- transthoracic echocardiography:
heart failure or ventricular hypertrophy predispose to drug-induced TdP
- exercise stress testing:
lack of appropriate QTc interval shortening
- genetic screening:
genetic mutation specific to the syndrome
More
Bidirectional ventricular tachycardia
History
assessment is time-critical, as delay in treatment may be fatal; digitalis toxicity or history of syncope in patient; history of sudden death in family members
Exam
rapid regular pulse, if palpable, due to hypotension; signs of hypoperfusion may be present, including changes in mental status
1st investigation
- 12-lead ECG:
wide-complex tachyarrhythmia with alternating morphologies (often with an alternating axis shift) and a regular R-R interval
More
Other investigations
- digitalis level:
elevated
Accelerated idioventricular rhythm
History
gradual onset and termination; symptoms consistent with acute myocardial infarction or history of angina; increased risk after thrombolytics or percutaneous coronary intervention for cardiac ischaemia; history of digitalis use should be investigated, as accelerated idioventricular rhythm (AIVR) can suggest digitalis toxicity
Exam
bradycardia or mild tachycardia is possible with possible irregular rhythm (intermittent sinus capture); patient may be hypotensive given the lack of atrioventricular synchrony, and there may be evidence of AV dissociation (cannon A waves or carotid pulse intensity variation)
1st investigation
- 12-lead ECG:
wide-complex rhythm (HR 40-120 bpm) with gradual acceleration beyond the sinus rate; may have intermittent sinus capture beats
Other investigations
- transthoracic echocardiography:
may demonstrate regional wall-motion abnormalities or valvular dysfunction
- serum potassium:
hypokalaemia predisposes to AIVR
- serum magnesium:
hypomagnesaemia predisposes to AIVR
- serum urea:
if elevated can predispose to digoxin toxicity
- serum creatinine:
if elevated can predispose to digoxin toxicity
- digoxin level:
elevated
More
Postural orthostatic tachycardia syndrome
History
symptoms of orthostatic intolerance include: palpitations, lightheadedness, blurred vision, exercise intolerance (which may also be a non-orthostatic feature of POTS), presyncope and syncope, tremor, generalised weakness, fatigue (which may also be a non-orthostatic feature of POTS); non-orthostatic symptoms include: dyspnoea, gastrointestinal symptoms, exercise intolerance, fatigue, headache, sleep disturbance, cognitive impairment, chest pain, bladder disturbance; may be symptoms of associated comorbidities, such as those of Ehlers-Danlos syndrome and autoimmune diseases, particularly Hashimoto’s thyroiditis and celiac disease
Exam
irregular heart rate, tachycardia, increased respiratory rate, generalised weakness; may be signs of associated comorbidities, such as those of Ehlers-Danlos syndrome and autoimmune diseases, particularly Hashimoto’s thyroiditis and celiac disease
1st investigation
- 10 minute standing test:
heart rate typically increases by ≥30 bpm (≥40 bpm in patients aged 12 to 19 years old) after changing position from supine to standing, and no orthostatic hypotension (sustained drop in systolic blood pressure by ≥20 mmHg)
More
Other investigations
- 24-hour Holter monitor:
demonstrates the association between tachycardia and orthostatic changes
More
Use of this content is subject to our disclaimer