History and exam
Key diagnostic factors
common
disclosure of inappropriate contact
Disclosure of any inappropriate contact should prompt a complete sexual abuse or assault evaluation and report to the appropriate child protective agency. It is preferable to record the disclosure of abuse in the patient's own words, rather than in a summary statement.[41]
uncommon
acute or residual (healing) anogenital trauma (any change); evidence of hymenal trauma (in children)
Injuries to the labia, penis, scrotum, or perineum are suggestive of trauma in children, unless a timely and plausible explanation is provided by the child and/or carer, such as an accidental anogenital straddle, crush, or impalement injury, or a history of surgical intervention (supported by a review of medical records). A thorough history can help with diagnosis.[55] Hymenal bruising, petechiae, abrasions, or partial/complete lacerations of any depth are also suggestive of trauma in children.[55][Figure caption and citation for the preceding image starts]: Absent hymen from 4 to 7 o'clock position in a sexually active 14-year-old girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Acute vaginal trauma in an 11-year-old victim of abduction and rapeGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Acute vaginal trauma in an 11-year-old victim of abduction and rapeGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].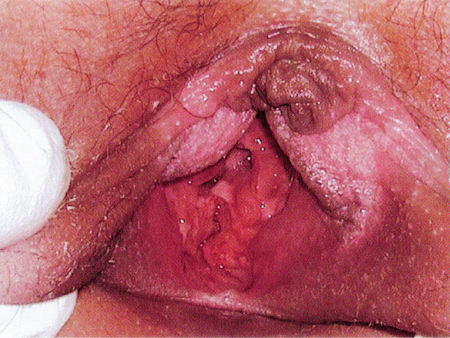
The majority of sexually abused children have normal genital examination findings. Even in cases of confirmed sexual abuse, normal genital findings are common.[44]
sexually transmitted infections
In children, confirmation of certain infections (HIV, syphilis, gonorrhoea, chlamydia, trichomonas) is diagnostic of sexual contact once perinatal (and percutaneous, in the case of HIV) transmission is excluded, while others (herpes simplex virus, anogenital condyloma acuminatum) are suspicious for sexual contact.[41][51] Bacterial vaginosis is inconclusive for sexual contact. In sexually active adults, it is often difficult to determine whether infections resulted from sexual assault or were pre-existing.
Other diagnostic factors
common
normal genital findings
The majority of sexually abused children and approximately half of assaulted adult women have normal genital examination findings. Even in cases of confirmed sexual abuse, normal genital findings are common.[44]
emotional and psychological sequelae
After a sexual assault, individuals may experience a rape-trauma syndrome, which unfolds in two phases.[14] The acute phase, lasting days to weeks, involves physical symptoms like widespread pain, and emotional reactions such as anger, anxiety, guilt, and mood swings. The delayed phase, occurring in the weeks or months following the assault, may include flashbacks, nightmares, and phobias.
Long-term psychological outcomes include post-traumatic stress disorder (PTSD), depression, anxiety, eating disorders, and sleep disorders.[7][15][16][17][18] In children, mental health disturbances may manifest as behavioural changes. Behavioural changes include internal or depressive symptoms, and external acting-out behaviours.
uncommon
anogenital lesions
Warts, ulcers, and bruises or petechiae may be indicative of sexual contact or trauma and warrant further investigation.[41][55]
Molluscum contagiosum, rashes, haemangiomas, nevi, lichen sclerosus, and urethral prolapse can be confused with signs of sexual abuse or assault. A repeat examination after 1-2 weeks may aid diagnosis, as these lesions will probably persist, whereas physical signs of sexual abuse will resolve or heal over time.
Anal fissures and tags are non-specific findings that may result from trauma to the anus or other conditions. Peri-anal laceration with exposure of tissue below the dermis is indicative of blunt force penetrating trauma.
Anogenital condyloma acuminata raises suspicion of sexual contact.[41][51] Human papillomavirus may be acquired from birth but present months or even years later. Lesions appearing for the first time in a child older than 5 years of age may be more likely to be the result of sexual transmission.
Anogenital ulcerations may be due to herpes simplex virus. Once herpes simplex infection is confirmed, the possibility of sexual abuse should be investigated.[41][51]
non-genital injuries
May be associated with sexual abuse or assault. For instance, acute trauma to oral tissues. In adults, non-genital injuries are more common than genital injuries.[50] A thorough history and complete physical examination can help determine the aetiology.
vaginal or penile discharge
This is a non-specific finding that should prompt testing for sexually transmitted infections as well as routine culture for other infections. Vaginal discharge is common in non-abused and abused girls and women.
Bacterial vaginosis is inconclusive for sexual contact.[41][51]
Once infection with gonorrhoea, chlamydia, or trichomoniasis is confirmed, this is diagnostic of sexual contact if perinatal transmission is excluded.[41][51][55]
harmful behaviours
sexual behaviour problems in children
chronic medical complaints in children
May indicate child psychological stress.
frequent or persistent genitourinary complaints
May indicate child psychological stress or sexually transmitted infection.
hymenal notches
Notching of the hymen may result from trauma but there is no consensus on the degree of significance in sexual abuse.[55]
Indeterminate findings include: hymenal notches or clefts at or below the 3 or 9 o’clock positions. Specifically, notches or clefts that nearly reach the base of the hymen but are not complete transections, and complete clefts or suspected transections to the base of the hymen at the 3 or 9 o'clock location. These findings should be interpreted with caution and confirmed through additional examination techniques.[55]
Notching may be confirmed in pre-pubertal girls using the knee-chest position if necessary, and in older girls by using a cotton swab or other device.[Figure caption and citation for the preceding image starts]: Knee-chest position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].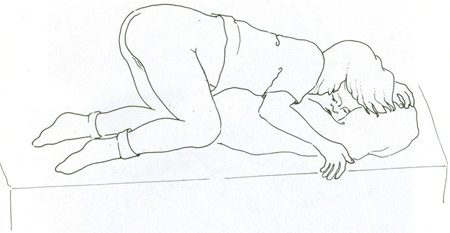
Risk factors
weak
sexual abuse of other children in the home
Sexual abuse of other children in the home should prompt sexual abuse evaluation. The strength of association of sexual abuse of other children in the home to sexual abuse of the presenting child is unclear.[19]
childhood exposure to intimate partner violence
single-parent household
adolescents and young women
Adolescents and young women are the most likely groups to be sexually assaulted.[5]
learning or physical disability
mental health issues
poverty or homelessness
sex workers
Sex workers are at increased risk of sexual assault.[25]
living in institutions or areas of conflict
People living in institutions or in areas of conflict are at increased risk of sexual assault. A history of sexual assault is more prevalent among incarcerated women than among the general female population.[26]
Use of this content is subject to our disclaimer