Approach
The diagnosis of sexual abuse and sexual assault is complex and has major ramifications; it is therefore important to follow diagnostic guidelines.
Initial assessment of child victims of sexual abuse includes psychosocial and medical components, and varies according to the child's pubertal status and the time elapsed since the most recent sexual contact. For all paediatric patients, providers must ensure that the child will be returning to a safe environment and that mandatory reporting to the relevant child protection agency has been done.
Patients may report sexual assault soon after the assault, or they may later seek medical care without necessarily disclosing why, unless specifically but sensitively asked. Post-assault medical care should include meeting healthcare needs, and in acute cases, evidence collection for medico-legal purposes if the patient consents. Good documentation is crucial, and can be supported by the availability of standardised forms for record-keeping.[38] Rape is a profoundly disempowering experience, and it is essential that care is provided in a way that supports individuals in reclaiming control over their lives.
Associated symptoms and behaviours
A child may display changes in their typical behaviour. The stress of sexual abuse may manifest as depressive symptoms, acting-out behaviour, or chronic medical complaints. The following may be signs of sexual abuse, although they are non-specific and the strength of association with child abuse is not quantified.
Sexual behaviour problems: many sexualised behaviours are developmentally normal. Sexual behaviours in children 12 years or younger that are not congruent with their developmental level or that are harmful to another person are termed problematic. Examples of behaviours that may be associated with sexual abuse include sexual behaviours that are coercive, persistently intrusive, or abusive.[39][40]
Symptoms of depression and post-traumatic stress disorder (PTSD): suicidal ideation should also be assessed.[41]
Chronic medical complaints: may be an indicator for child psychological stress.
Frequent or persistent genito-urinary complaints: may be an indicator of child psychological stress or sexually transmitted infection.
Children who are being sexually exploited may present with additional findings such as: unexplained or patterned injuries or tattoos; a history of running away from home; a false or changing history including a lack of identifying documents or home address; a history of multiple STIs or pregnancies; or possession of large amounts of cash. Suspicion should also be raised if there is a significant age difference between the patient and sexual partner, or if a person other than the patient insists on providing the history.[42]
Adults who have been sexually abused (as children or more recently) may present with emotional and psychological problems such as depression or substance misuse, or physical symptoms such as chronic pelvic pain.[14] After a sexual assault, individuals may experience a rape-trauma syndrome, which unfolds in two phases.[14] The acute phase, lasting days to weeks, involves physical symptoms like widespread pain, and emotional reactions such as anger, anxiety, guilt, and mood swings. The delayed phase, occurring in the weeks or months following the assault, may include flashbacks, nightmares, phobias, and physical symptoms such as somatic and gynaecological symptoms. Longer-term psychological problems include PTSD, depression, anxiety, eating disorders, sleep disorders, substance misuse, and thoughts or acts of self-harm or attempted suicide.[7][14][15][16][17][18]
Interviewing
Children and adults should be asked about possible sexual abuse and assault in a non-leading manner, with open-ended questions. Interviewing a child includes use of age-appropriate language and thorough documentation of the questions and the child's responses. It is preferable to record disclosures from both children and adults in their own words, rather than in a summary statement.[41] Interviewers should maintain professional and non-emotional reactions to the child’s answers.[43]
Physical examination when sexual abuse and assault is suspected
If child sexual abuse and assault is suspected, a referral to a hospital with a specialised abuse assessment clinic should be considered.[41] The American Academy of Pediatrics has set out detailed guidance for paediatricians carrying out anogenital examinations.[41] Physical examination findings are most often normal in victims of child sexual abuse.[44][45][46] However, sexual abuse may be among the differential diagnoses to consider if one of the following findings is noted on examination:
Vaginal discharge
Anogenital lesions or dermatological findings
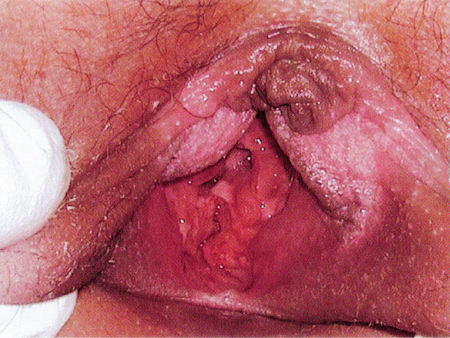
Hymenal abnormalities or anogenital trauma.[Figure caption and citation for the preceding image starts]: Absent hymen from 4 to 7 o'clock position in a sexually active 14-year-old girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].

Adolescents develop pubertal changes along a predictable progression. Secondary sexual characteristics are classified according to sexual maturity rating (SMR). Pre-adolescent or (pre-pubertal) children have not yet begun puberty and are SMR stage 1. Adolescents are at SMR stage 3 and over. The distinction between pre-pubertal children and adolescents is clinically important due to effects on physical examination, evaluation, and treatment. For example, speculum examinations should not be used in pre-pubertal children in the office setting.[41]
In adult women who have been sexually assaulted, injuries are found in about half of cases and are seen more commonly in older victims.[47][48][49] Non-genital injuries are more common than genital injuries.[50] The absence of injury does not imply consent or exclude penetration, even in women who deny previous sexual activity. Evidence of sexually transmitted infections in these patients may represent the assailant’s secretions or previous sexual contact.
Acute presentation: ≤72 hours since abuse or assault
Psychosocial assessment should include:
Evaluation of discharge arrangements, typically carried out in conjunction with the relevant child protection agency, is indicated to ensure that the child or adult will be returning to a safe environment
Referral for psychological/social services is also recommended.
Medical evaluation (with consent) should include:
Complete physical examination to assess for possible injuries or other medical conditions. Children who have been sexually abused and assaulted may be at risk of other types of abuse and neglect. It is therefore recommended that a thorough general physical examination should follow the anogenital examination.[41]
Collection of forensic evidence specimens. Samples such as a mouth swab for the perpetrator’s DNA, and urine and blood for toxicology should be collected as soon as possible following sexual assault when indicated. In cases of sexual abuse involving pre-pubertal children, evidence is more likely to be found on objects present at the assault (e.g. bedding or clothing) than on the child's body.
Baseline testing for HIV and syphilis.
Baseline measurement of liver function tests, full blood count, serum urea, and serum creatinine prior to commencement of HIV post-exposure prophylaxis.
Pregnancy test for females of reproductive age.
Testing for sexually transmitted infections (STIs)
Individuals may be tested for STIs at the time of presentation. However, detection of an STI may represent an infection acquired before the assault and/or infection in the assailant’s secretions (which would nonetheless be indications for treatment).[51] Empirical prophylactic treatment is recommended in adolescents and adults, as compliance with follow-up visits is traditionally poor.[51] Prophylactic treatment is not generally offered to pre-pubertal children due to the decreased transmission rates of STIs and the evidentiary value of a positive test in a child who cannot legally consent.[38][51]
In adults and adolescents, tests should include the following: Neisseria gonorrhoeae, Chlamydia trachomatis, Trichomonas vaginalis, syphilis, and HIV.[51][52] If ulcers or vesicles are present, specimens for viral culture or molecular testing for herpes simplex virus should be collected.[51] If vaginal discharge is present, testing for bacterial vaginosis, Candida, and aerobic culture should be done. Tests for syphilis and HIV may not be positive until 3-6 months after infection.
Culture for the isolation of N gonorrhoeae, C trachomatis, and T vaginalis has been the standard due to its high specificity. However, the appropriate media is often not readily available, and some have a relatively short shelf-life. Consequently, nucleic acid amplification tests (NAATs) are increasingly used, but note that testing protocols vary according to location of practice, and consultation with an expert (e.g., a microbiologist or genitourinary consultant) is recommended before using NAAT and in the event of a positive test result to ensure accuracy of testing and correct interpretation of results, particularly in view of their potential medicolegal significance.[51][52]
For pre-pubertal children, the decision to obtain genital or other specimens for STI testing should be made on an individual basis based on the history of the assault.[51] However, site-specific testing based on history may not be reliable, particularly in pre-verbal children or children unable to provide details of the event. Some guidelines recommend universal testing of all three sites (urogenital, rectal, and pharyngeal) in all children presenting for sexual abuse, as this may identify infections that would be missed otherwise.[52][53][54][55] Due to the low prevalence of N gonorrhoeae and C trachomatis infection in children, false positive NAATs can occur, and all positive results should be confirmed with input from an appropriate consultant (e.g., a genitourinary and/or microbiology clinician).[51][52]
Hepatitis B
Consider testing for hepatitis B depending on risk factors and vaccination status.[51][52] Note that a test for hepatitis antibodies to determine the need for hepatitis B immunoglobulin or vaccine should not delay the administration of hepatitis B vaccine or immunoglobulin. If required, hepatitis B vaccine may be provided up to 3 weeks after the assault as the hepatitis B virus has a long incubation period.[38] If there is no history or proof of completion of a full hepatitis B vaccination series, immediate hepatitis B immunoglobulin should be administered in addition to vaccination if the assailant is hepatitis B surface antigen positive.[51] Arrangements should be made for subsequent doses of hepatitis B vaccine to be given.
Hepatitis C
Consider testing for hepatitis C depending on risk factors.[52]
Forensic examination
A forensic examination should be strongly considered for any child, adolescent, or adult, and undertaken as soon as practicable. The recommended timing of the examination depends on the sample type and local jurisdictions; paediatricians should familiarise themselves with their relevant policy. Most protocols recommend that forensic evidence should be collected if less than 72 hours have passed since the assault but some are as late as 168 hours.[16][41][56]
Initial history includes a general medical and social history. All individuals in the room at the time of questioning regarding the sexual assault should be noted. Questions should be carefully documented, non-leading, and open-ended, and responses noted verbatim in the chart.
A complete but sensitive examination should be performed, including a thorough examination of the skin to note any traumatic findings. Ideally the anogenital examination is performed with a colposcope (or comparable magnification device) that has a photographic capability. All injuries should be carefully documented using agreed nomenclature and body diagrams. The supine frog-leg position is used for the genital examination of pre-pubertal girls; abnormal hymenal findings may be confirmed using the prone knee-chest position if necessary, although as this position carries the potential for increased vulnerability and discomfort for children, it is preferable to avoid it if possible. Adolescent girls and women are generally examined in the lithotomy position. The use of labial traction greatly enhances visualisation of the hymen.[Figure caption and citation for the preceding image starts]: Acute vaginal trauma in an 11-year-old victim of abduction and rapeGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Supine frog-leg position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Supine frog-leg position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].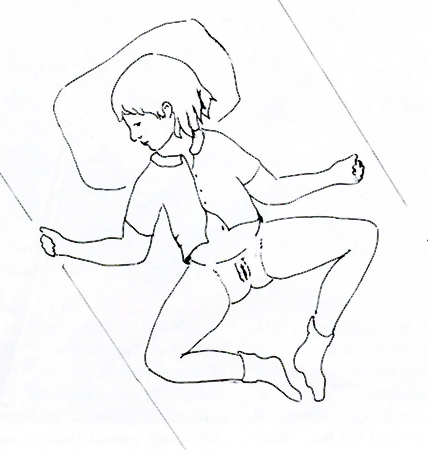 [Figure caption and citation for the preceding image starts]: Knee-chest position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Knee-chest position for examination of a pre-pubertal girlGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].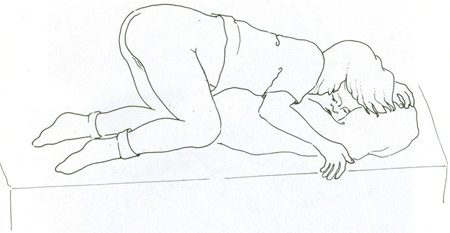 [Figure caption and citation for the preceding image starts]: Labial traction techniqueGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Labial traction techniqueGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Normal annular hymenGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Normal annular hymenGirardet RG, et al. Curr Probl Pediatr Adolesc Health Care. 2002;32:211-246. Used with permission [Citation ends].
Forensic evidence collection kits are available in most hospital emergency departments, and include packets in which to send specimens of blood, hair strands and combings, and fingernail, pharyngeal, genital, and anal swabs to a forensic laboratory. In some countries, forensic examination and aftercare are provided in specialist sexual assault centres. The clothing worn at the time of the assault, as well as associated bedding and other samples such as tampons, may also contain forensic evidence.[38]
Non-acute presentation: >72 hours after abuse or assault
Psychosocial assessment is the same as for patients presenting <72 hours after the abuse or assault. The medical and forensic evaluation (with consent) should include the following investigations:
Complete physical examination to assess for possible injuries or other medical conditions.
A forensic examination, if indicated by regional or national protocols. Recommendations about the timeframe within which collection of forensic evidence specimens (cervical and vaginal samples) from post-pubertal females can be performed differ between regions. Most protocols recommend that forensic evidence should be collected if less than 72 hours have passed since the assault, but some are as late as 168 hours.[16][41][56] When indicated, a forensic examination should be carried out in the same way as for patients presenting <72 hours after the abuse or assault.
Testing for C trachomatis and N gonorrhoeae and T vaginalis.[51][52]
If ulcers or vesicles are present, a specimen for viral culture or DNA for herpes simplex virus should be collected.[51]
If vaginal discharge is present, testing for bacterial vaginosis, candida, and aerobic culture should be performed.[51][52]
Serological testing for HIV and syphilis. These tests may not be positive until 3-6 months after infection.
Testing for pregnancy in females of reproductive age.[Figure caption and citation for the preceding image starts]: Example of the use of a body diagram to record injuriesWelch J, Mason F. BMJ 2007;334:1154-1158 [Citation ends].
The clinical significance of physical findings in children
The classification scheme proposed by Joyce Adams et al may be used to determine the significance of physical findings.[55]
Normal variants include:
A range of hymenal configurations such as annular, crescentic, imperforate, micro-perforate, septate, and redundant hymens; hymens with tags, mounds, bumps, or notches (above 3 and 9 o’clock regardless of depth, or below these positions if not extending to the base); a smooth or asymmetric posterior rim; and a hymen that appears narrowed but is normal. Additional normal findings include periurethral or vestibular bands, intravaginal or external hymenal ridges, diastasis ani, perianal skin tags, hyperpigmentation of genital or perianal tissues, and dilation of the urethral opening. Midline features such as a groove in the fossa, perineal groove, median raphe, and linea vestibularis are also normal. The pectinate/dentate line may be visible during full anal dilation caused by flatus or stool, and reflex anal dilation can occur during examination due to positioning or traction. Anal dilation may reveal normal structures like the dentate line, anal columns, and crypts, which can be mistaken for injury but are not indicative of trauma.
Findings commonly caused by conditions other than trauma or sexual contact include:
Erythema, inflammation, fissuring, and maceration of the perianal, perineal, or vulvar tissues, often related to poor hygiene or irritant dermatitis; increased vascularity of the vestibule and hymen; labial adhesions; and friability of the posterior fourchette. Other findings include non-STI-related vaginal discharge, anal fissures, venous congestion or pooling in the perianal region, and complete or immediate anal dilation. The latter may occur in children with predisposing factors such as constipation or encopresis, children under sedation or anaesthesia, or children with impaired neuromuscular tone.
Infections not related to sexual contact include erythema, inflammation, and fissuring due to bacterial, fungal, viral, or parasitic infections acquired through non-sexual routes. Common pathogens include Streptococcus (Groups A and B), Staphylococcus sp., Escherichia coli, and Shigella. Genital ulcers may also result from viral infections such as Epstein-Barr virus.
Findings due to other conditions which can be mistaken for abuse include:
Erythema, inflammation, and fissuring, of the perianal, perineal, or vulvar tissues due to irritant dermatitis (e.g., Jacquet’s); inflammatory findings such as aphthous ulcers, inflammatory bowel disease (anal fissures or tags, rectal discharge), and Behçet’s disease (painful ulcers); and dermatological conditions such as lichen sclerosus, folliculitis, vitiligo, angiokeratomas, and haemangiomas. Painful ulcers may result from immunological causes such as pyoderma gangrenosum. Multifactorial or idiopathic findings include urethral or rectal prolapse and anal funnelling.
Indeterminate findings include:
Complete and immediate anal dilation involving both sphincters without other predisposing factors (e.g., constipation or encopresis, sedation or anaesthesia, or impaired neuromuscular tone), and a notch or cleft in the hymen ring, at or below the 3 or 9 o’clock positions. Specifically, notches or clefts that nearly reach the base of the hymen but are not complete transections, and complete clefts or suspected transections to the base of the hymen at the 3 or 9 o'clock location. These findings have been associated with a history of sexual abuse in some studies, but at present, there is no expert consensus as to how much weight they should be given with respect to abuse. The final two findings listed should be interpreted with caution and confirmed through additional examination techniques.
Infections that can be spread by both sexual transmission and non-sexual transmission include molluscum contagiosum in the genital or anal area, condyloma acuminatum (human papillomavirus) in the genital or anal area, and herpes simplex virus types 1 and 2, diagnosed by culture or nucleic acid amplification testing (NAAT) in oral, genital, or anal sites. Gardnerella vaginalis, though associated with sexual activity, is also found in pre-pubertal and adolescent vaginal flora. Mycoplasma genitalium and Ureaplasma urealyticum are typically sexually transmitted in adolescents, but their prevalence and transmission in younger children are not well understood.
Findings caused by trauma (suggestive but not diagnostic of abuse) include:
Acute trauma to genital or anal tissues: Lacerations or bruising of the labia, penis, scrotum, or perineum; lacerations of the posterior fourchette or vestibule (not involving the hymen); hymenal bruising, petechiae, abrasions, or partial/complete lacerations of any depth; vaginal lacerations; and perianal bruising or lacerations exposing tissue below the dermis.
Residual or healing injuries: Scarring of the perianal area or posterior fourchette/fossa (rare and difficult to diagnose without prior documentation of a previous injury at the same location); healed hymenal transections or complete clefts (a defect below the 3 to 9 o’clock location extending to or through the base with no tissue remaining); and signs of female genital mutilation, such as loss of clitoral or labial structures or characteristic scarring.
Acute oral trauma: Unexplained injuries or petechiae to the lips or palate, especially near the junction of the hard and soft palate.
Infections caused by sexual contact, if confirmed by testing and perinatal transmission has been excluded, include:
Genital, rectal, or pharyngeal infection with N gonorrhoeae or C trachomatis; T vaginalis detected in vaginal secretions or urine; syphilis; and HIV (if other routes of transmission such as through blood or contaminated needles have been excluded).
Findings diagnostic of sexual contact include:
Positive pregnancy test
Semen identified in forensic specimens taken directly from a child's body.
Trauma in adults
Injuries have been reported in about half of adults reporting sexual assault; they are more common in older women.[47][48][49] Non-genital injuries are more common than genital injuries.[50] The absence of injury does not imply consent or exclude penetrative intercourse, even in people who deny previous sexual activity.
Injuries are usually minor but may need treatment. They should be documented: for example, using a body diagram to record measurements, a description, and position in relation to anatomical sites.
Major injuries, for example, head trauma, are rare but may be life-threatening, and their management must take precedence over forensic examination. Occasionally someone may present with vaginal or anal bleeding following penetration with a penis or foreign body. Such individuals should be assessed in an acute hospital setting with resuscitation facilities, and may require examination under anaesthesia and operative repair.
Use of this content is subject to our disclaimer