Approach
History
Most cases occur in children younger than 12 months. Patients should be assessed first with a complete history and physical examination with a focus on the nature of abdominal pain (colicky/intermittent episodes versus constant), the presence of red currant jelly stools, and the presence or absence of vomiting. Almost all infants with intussusception present with abdominal pain and vomiting.[17] The classic symptom of red currant jelly stool or rectal bleeding is present in 35% to 73% of cases.[3][11][18] Progressive lethargy is often associated, and patients may have a history of a recent viral illness.[3]
Physical examination
Physical examination should begin with an assessment of haemodynamic stability. Abdominal examination may yield findings of a palpable abdominal mass, abdominal distention, or even peritonism.[1] The abdominal mass may be subtle and examination is best performed when the infant is settled in between colic bouts. The clinician may wish to examine for a mass when the child is on their carer's lap; the infant may be more settled, and the mass might be more readily palpable when the patient is prone or lateral.
Blood on digital rectal examination may be found but its absence does not refute the diagnosis. Hypovolaemic shock, suggestive of intestinal ischaemia or necrosis, is present in 5% to 10% of cases.[3]
Imaging studies
The finding of a target sign (variants according to appearance or imaging modality include bull’s eye sign, doughnut sign, crescent-in-doughnut sign, and multiple concentric ring sign) is characteristic of intussusception on plain-film abdominal x-rays or less commonly by computed tomography (CT).[1][19][Figure caption and citation for the preceding image starts]: Transverse sonogram of the abdomen showing the doughnut sign (concentric rings within the lumen of a distended loop of bowel)Adapted from the Student BMJ. 2008;16:76. Copyright 2010 by the BMJ Publishing Group; used with permission [Citation ends].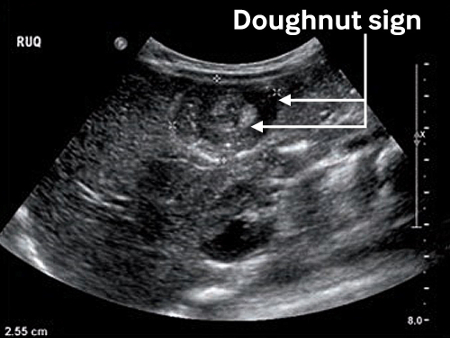
Plain abdominal films may be normal, although occasionally a partial intestinal obstruction may be seen. Other suggestive signs include the presence of a soft-tissue mass, an empty right lower quadrant, air in a dislocated appendix, and signs of a small-bowel obstruction.[20][21] If peritonitis is present, immediate surgical consultation is advised, and abdominal plain-film x-rays should be assessed for the presence of pneumoperitoneum. The presence of pneumoperitoneum is indicative of intestinal perforation as a complication of intussusception.
A contrast enema (air or contrast reagent) can be performed to diagnose intussusception but is contraindicated in the presence of pneumoperitoneum. Liquid or air enema remain the most specific and sensitive diagnostic tests and can localise the extent of the process. The diagnostic efficacy of liquid contrast and air enema may be comparable.[21] In one Cochrane review, air enema was seen to be more effective than liquid contrast for reducing intussusception, although the evidence base was deemed low quality.[22]
In many centres, ultrasound is favoured for the diagnosis of intussusception.[23] If the patient is clinically stable and perforation is not suspected, ultrasonography should be the initial diagnostic test for intussusception. Ultrasound has a reported diagnostic accuracy of up to 100%.[23] The presence of a 3 to 5 cm mass just deep to the right-sided abdominal wall with the characteristic doughnut sonographical appearance is diagnostic of intussusception. Ultrasound may also identify the presence or absence of a pathological lead point[24] (an associated anatomical abnormality of the intestine such as a luminal polyp or mass lesion that may lead to the development of intussusception).[25] Mesenteric blood flow can also be assessed by ultrasound, the absence of which is predictive of bowel-wall necrosis and irreducibility.[26]
[Figure caption and citation for the preceding image starts]: Abdominal x-ray showing impaired passage of barium at site of obstruction due to intussusceptionFrom the collection of Dr David J. Hackam; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Ultrasound image showing invagination of a segment of bowel into the adjacent segmentBMJ Case Reports 2009; doi:10.1136/bcr.04.2009.1730; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image showing invagination of a segment of bowel into the adjacent segmentBMJ Case Reports 2009; doi:10.1136/bcr.04.2009.1730; used with permission [Citation ends].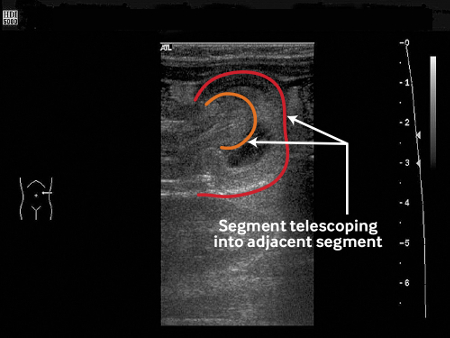 [Figure caption and citation for the preceding image starts]: Transverse sonogram of the abdomen showing the doughnut sign (concentric rings within the lumen of a distended loop of bowel)Adapted from the Student BMJ. 2008;16:76. Copyright 2010 by the BMJ Publishing Group; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Transverse sonogram of the abdomen showing the doughnut sign (concentric rings within the lumen of a distended loop of bowel)Adapted from the Student BMJ. 2008;16:76. Copyright 2010 by the BMJ Publishing Group; used with permission [Citation ends].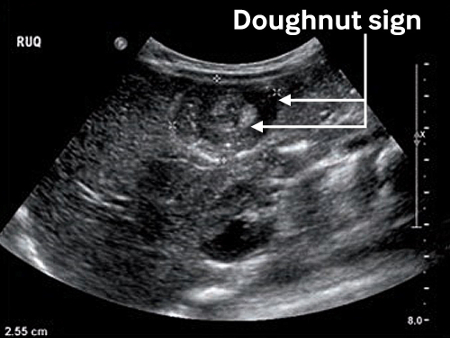
Use of this content is subject to our disclaimer