Approach
Patients may present with signs and symptoms of nerve, venous, or arterial compression, or certain combinations thereof. Careful history and examination is essential. Provocative tests can support diagnosis. Imaging is tailored to the suspected subtype of thoracic outlet syndrome (TOS; neurological, venous, or arterial).
History and examination
Many historical factors can predispose patients to compression of the neurovascular components of the thoracic outlet: trauma (e.g., fracture of the clavicle), motor vehicle collisions, a fall on the outstretched arm, repetitive overhead activity, cervical or bony abnormalities (e.g., cervical ribs), and poor posture.[1][64]
There are many common examination findings and manoeuvres for diagnosing TOS; however, specific history and examination findings depend on the suspected type of TOS and the localisation of the compression.[1][3][4]
Nerve (brachial plexus) compression
Signs and symptoms include:
Pain in the head, neck, upper back, anterior chest, shoulder, arm, forearm, and/or hand
Paraesthesia in the arms, hands, and/or fingers (unilateral or bilateral)
Tenderness to palpation in the supraclavicular region, anterior chest wall, scalene muscles, trapezius, or pectoralis minor muscles
Patchy alterations in cutaneous sensation in the arm and hand, not following the distribution of a single peripheral nerve
A sense of motor weakness in the shoulder girdle, arm, and hand
Consistent aggravation of symptoms with elevation of the arm, especially to overhead positions
Diminished radial pulse with elevated arm positions may be present
Altered shoulder girdle mechanics, scapular dyskinesis, or possible winged scapula
Mild fluctuating soft tissue swelling in the supraclavicular space
Firm nontender palpable mass in the supraclavicular space (e.g., cervical rib)
Hand muscle atrophy, most pronounced in thenar eminence and interosseus muscles (Gilliatt-Sumner hand)
Possible sympathetic overactivity, including excessive cold or warm sensations, excessive sweating, and digital vasospasm with intermittent mottling discoloration in the upper extremity and hand (Raynaud's phenomenon)
Can sometimes mimic atypical chest pain ('pseudoangina'), when compression is caused by pectoralis minor[89][90]
Symptoms can range from mild and intermittent, to severe and disabling
Symptom duration of at least 3 months
Absence of other conditions which could cause similar symptoms (e.g., degenerative cervical spine disease, rotator cuff injuries, peripheral neuropathy syndromes)
Venous (subclavian and axillary) compression
Signs and symptoms include:
Spontaneous onset of swelling extending throughout the arm from shoulder to hand
Cyanosis, erythema, or dusky appearance of the upper extremity
Exercise fatigue and heaviness of the upper extremity
Symptoms may be related to repetitive upper extremity activity, overhead use, or heavy lifting
Intermittent episodes of upper extremity pain with vigorous upper extremity activity
Subcutaneous venous collateral distention around the shoulder
Possible presence of central venous catheters or cardiac pacemaker leads
No known coagulopathy, thrombophilia disorder, malignancy, recent coronavirus infection or vaccine, or use of prothrombotic medications
Pulmonary embolism may accompany deep vein thrombosis in up to 20% of patients with venous TOS, as shown by CT angiography of the chest, but the thrombus burden is typically small and not life-threatening
A chronic presentation of venous TOS may be seen in patients with long-standing symptoms of upper extremity venous congestion. These patients will have the same risk factors as those with an acute presentation, seeking medical attention after persistence of symptoms and/or the absence of a diagnosis.[91]
Arterial (subclavian and axillary) compression
Arterial TOS is clinically very important as the unattended outcomes can include advanced upper limb ischaemia, amputation of the hand or fingers, and vertebrobasilar stroke.
Signs and symptoms include:
Dull ache, numbness, or pain in the upper extremity, at rest or with activity (e.g., claudication)
Early fatigability with arm activity or elevation (e.g., dead arm sensation)
Pallor and/or coolness of the upper extremity
Acute upper limb ischaemia with rest pain
Digital ulceration, non-healing wounds, and/or gangrene
Possible sympathetic overactivity, including excessive cold or warm sensations, excessive sweating, and digital vasospasm with intermittent mottling discoloration in the upper extremity and hand
May be asymptomatic
Blood pressure discrepancy (e.g., 20 mmHg difference) between upper extremities
Diminished radial pulse with arm elevation, possible in resting position if arterial thrombosis
Palpable supraclavicular mass (e.g., cervical rib)
Possible prominent supraclavicular pulse to palpation (e.g., subclavian artery aneurysm)
Possible supraclavicular systolic bruit, accentuated with arm elevation
Possible vertebrobasilar stroke due to retrograde embolisation from subclavian artery
Combined forms of neurovascular compression
Findings of both arterial TOS and neurogenic TOS may arise in some patients with cervical ribs.
Findings of neurogenic TOS may develop in some patients with venous TOS as a result of brachial plexus irritation related to perivenous inflammation and venous thrombosis.
Patients with a history of clavicular fracture may develop any form of TOS.
Neurogenic TOS and arterial TOS may be associated with sympathetic overactivity that can result in more severe symptoms of excessive upper extremity pain, cutaneous hypersensitivity, temperature alterations, sweating, and digital vasospasm because of the additive or synergistic effects of sympathetic stimulation.
Complex regional pain syndrome (CRPS) may also arise in patients with neurogenic TOS or arterial TOS and may substantially complicate diagnosis and management.
The 'double crush' phenomenon may occur when there is nerve compression at two or more sites along the path of a peripheral nerve. This synergistically enhances symptom intensity, beyond that expected from a single site of nerve compression.[92][93][94][95]
[Figure caption and citation for the preceding image starts]: Schematic diagram summarising the factors involved in thoracic outlet compression and the resulting signs and symptomsFrom the collection of Dr Robert W Thompson (adapted from Dr Chaney Stewman); used with permission [Citation ends].
Provocative manoeuvres
Numerous provocative physical examination manoeuvres exist to reproduce brachial plexus impingement in assessing possible neurogenic TOS.[1][4][96] These manoeuvres produce subjective symptoms of pain and paraesthesias if positive or abnormal. Some of these manoeuvres are based on dampening or obliteration of the radial pulse, which can be associated with brachial plexus compression at the scalene triangle, but positional dampening of the radial pulse is not uncommon in asymptomatic individuals and cannot be used to establish a diagnosis of neurogenic TOS.[1][18][97] No single provocative manoeuvres can establish or exclude a diagnosis of neurogenic TOS and all exhibit variable results.[98][99][100][101][102][103] The following manoeuvres therefore remain non-specific and cannot be used in isolation for the diagnosis of TOS, but instead are used in combination as confirmatory testing, in conjunction with patient history and other diagnostic testing. The most commonly used manoeuvres include the following:
Upper limb tension test (ULTT): A series of tests of all tissues in the upper limb with a preferential focus on the cervical nerve roots, brachial plexus, and median nerve. This involves bilateral shoulder abduction to 90°, lateral rotation of the shoulders, extension at the elbows, and neck lateral flexion away from or toward the side tested. Symptoms may be reproduced with shoulder abduction alone, and expected to be aggravated with wrist extension and alleviated with wrist flexion.[1][64][100]
Elevated arm stress test (EAST; Roos test): Both arms are placed at right angles to the shoulder, with the forearms at right angles to the upper arms (the 'surrender' position). Both hands are repeatedly opened and closed as fast as possible to see if the characteristic symptoms are reproduced (usually within 1 minute for a positive test). Another variation can be used to determine the duration the patient is able to continue the test before having to drop the affected arm, with more than 3 minutes considered a negative test. Approaches to standardise the test and quantify the outcomes may be fruitful.[1][4][104][105]
Adson (scalene) test: The patient takes and holds a deep breath, extends the neck fully, and turns the head toward the affected side. This tightens the anterior and middle scalene muscles, thus decreasing the interspace and magnifying pre-existing compression of the brachial plexus and subclavian artery. The principal endpoint is a reproduction of the characteristic symptoms of pain, numbness, and tingling, and dampening or obliteration of the palpable radial pulse.
Costoclavicular test (Halsted test or military brace): The shoulders are drawn downward and backward. This narrows the costoclavicular space by approximating the clavicle to the first rib and thus tends to compress the neurovascular bundle.
Wright manoeuvres: Simulating a lazy hand raise (externally rotate and abduct arm to 180° and flex at elbow).
Hyperabduction test: Hyperabduction of the arm to 180° tightens the scalene triangle and pulls the components of the neurovascular bundle around the pectoralis minor tendon, the coracoid process, and the head of the humerus.
Stretch test: The arm is abducted 90° with elbow extension, palm facing forward, and thumb pointing up to the ceiling. This stretches the plexus. A positive test is an uncomfortable pulling sensation of the inner arm, sometimes extending into the forearm or hand, on abduction. The patient may develop paraesthesias or heaviness of the extremity. The patient then laterally flexes the head to the opposite side. A positive test of lateral flexion is exacerbation of the symptoms.
[Figure caption and citation for the preceding image starts]: The Adson maneuver tightens the anterior and middle scalene muscles, decreasing interspace and magnifying pre-existing compression of the brachial plexus and subclavian artery. The patient takes and holds a deep breath, extends the neck fully, and turns the head toward the affected side. Obliteration or decrease in the radial pulse indicates neurovascular compression at the thoracic outletReprinted with permission from Netter Images [Citation ends].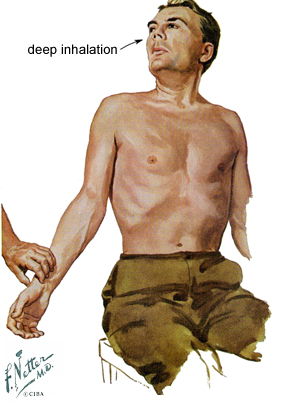
Imaging
Bony abnormalities are present in 5% to 10% of patients with neurogenic TOS and in almost all patients with arterial TOS, occurring as partial or complete cervical ribs (articulated with the first rib), hypoplastic first ribs, bridging fusion between the first and second ribs, first rib fractures, or clavicular deformities.[106][107] An initial chest x-ray and/or cervical spine x-ray can reveal these abnormalities and is the initial diagnostic test for all patients with TOS.[1][108]
[Figure caption and citation for the preceding image starts]: Cervical ribs. Chest radiographs demonstrating a patient with a partial cervical rib on the right side (A) and a patient with a complete cervical rib on the left side (B)From the collection of Robert W. Thompson, MD; used with permission [Citation ends].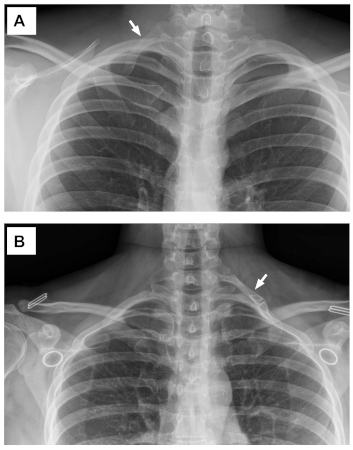
Plain radiographs or MRI of the cervical spine are important in the assessment of potential neurogenic TOS, to help exclude degenerative spine disease as an alternative or concomitant source of symptoms. MRI of the shoulder may be used in some patients to exclude or identify significant shoulder pathology. Contrast-enhanced MRI of the brachial plexus (neurography) can also be considered, as it can provide anatomical detail of soft tissues and may help identify other abnormalities, such as congenital fibrous bands.[4][108][109][110] While brachial plexus MRI and neurography may reveal structural anomalies and/or perineural inflammatory changes to support a diagnosis of neurogenic TOS, many anatomical variations are below the resolution of imaging studies. With the exception of an overt osseous abnormality (e.g., cervical rib), imaging findings do not generally impact the type of surgical treatment that might be performed for neurogenic TOS.[1][106][107][110][111] Images are obtained with the patient in both neutral and shoulder abduction positions to best localise any areas of nerve impingement. Vascular laboratory imaging studies (e.g., arterial or venous ultrasound) are often performed but do not contribute to establishing a diagnosis of neurogenic TOS.[97] It is important to reiterate that negative imaging studies cannot be used to exclude a clinical diagnosis of neurogenic TOS.
If venous TOS is suspected, upper extremity Duplex ultrasound is the most useful and readily available first test.[1][108] This can demonstrate axillary-subclavian vein thrombosis if the clot has extended past the clavicle, but ultrasound may miss central subclavian vein occlusion or stenosis in more than 20% of patients.[112] Duplex ultrasound is therefore very specific in establishing a diagnosis but given the 21% false-negative rate it cannot be used to exclude venous TOS.[112][113] If the patient has presented within several weeks of the onset of symptoms, it is most efficient to proceed directly to catheter-based contrast venography (regardless of the results of ultrasound), which can image the axillary-subclavian vein with a high degree of accuracy and allows immediate catheter-directed treatment by thrombolysis, mechanical (suction) thrombectomy, and balloon angioplasty.[79][108] Venography can also be easily performed with different arm positions to demonstrate positional compression of the subclavian vein. The efficacy of thrombolysis/thrombectomy is significantly reduced the patient has presented with symptoms lasting more than several weeks, in which case cross-sectional imaging of the axillary-subclavian vein can also be accomplished by either CT angiography or MR angiography.[106][108][113] These studies are best conducted with contrast injected into the opposite arm and images obtained with the affected arm at rest and in an overhead position.
[Figure caption and citation for the preceding image starts]: Upper extremity venography. (A): Initial venogram showing thrombotic occlusion of the axillary-subclavian vein. (B): Completion venogram after catheter-directed thrombolysis and suction thrombectomy, with restoration of a patent axillary-subclavian vein and residual venous stenosis at the level of the first ribFrom the collection of Dr. Robert W. Thompson; used with permission [Citation ends].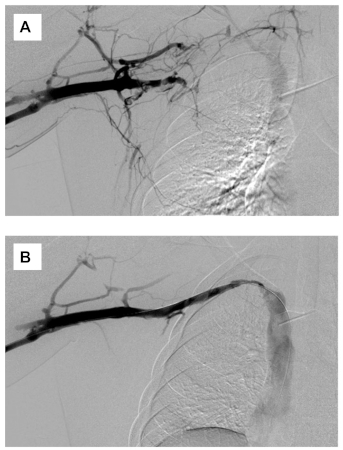
If arterial TOS is suspected, the presence of a cervical rib or other bony abnormality can be easily assessed by CXR. Vascular Doppler ultrasound studies are useful to analyse dynamic flow in the axillary and subclavian arteries and detect any thrombosis, stenosis, or aneurysmal changes.[1][108] CT angiography is recommended to demonstrate arterial compression.[1][108] MR angiography may identify the cause and severity of arterial TOS, and guide surgical or endovascular management.[108] Conventional arteriography may also be performed but has been largely replaced by alternative imaging for diagnosis and is mostly used during surgery for arterial TOS.
The principal risk of subclavian artery aneurysms stems from thromboembolism rather than rupture. Even relatively small aneurysms can lead to critical upper extremity ischaemia or vertebrobasilar stroke due to the dynamic nature of these vessels during upper extremity activity. Therefore, the presence of a mural thrombus, which significantly increases the potential for embolism, is a more critical factor in risk assessment than the size of the aneurysm.[1][18]
[Figure caption and citation for the preceding image starts]: Subclavian artery aneurysms. (A and B): Plain chest radiograph showing complete cervical rib on the right side (arrow) and an image from CT angiogram showing a subclavian artery aneurysm arising immediately past the point of arterial compression by the cervical rib (arrow). (C and D): Plain chest radiograph showing complete cervical rib on the right side (arrow) and a 3-D reconstruction from a CT angiogram demonstrating a subclavian artery aneurysm immediately past the point of arterial compression by the cervical rib (oval highlight). CR: cervical ribFrom the collection of Dr. Robert W. Thompson; used with permission [Citation ends].
Nerve conduction studies
Upper extremity electrodiagnostic studies (nerve conduction velocity and electromyography) can be useful in evaluation of patients with suspected neurogenic TOS, primarily to help rule-out alternative or concomitant diagnoses (e.g., carpal or cubital tunnel syndrome or cervical radiculopathy).[1][4][107] Although such studies are usually normal in patients with neurogenic TOS due to the dynamic nature of brachial plexus compression, some patients with neurogenic TOS can exhibit findings of brachial plexus compression neuropathy that helps to solidify or reinforce the clinical diagnosis. Most patients with possible neurogenic TOS should therefore have upper extremity electrodiagnostic testing, primarily to exclude other conditions.
Pathognomonic findings on nerve conduction studies in the appropriate clinical context for neurogenic TOS include reduced motor amplitude of the median nerve, as well as reduced sensory amplitude of the medial antebrachial cutaneous and ulnar nerves.[5] Specifically, the median motor compound muscle action potential (recording thenar muscle, commonly the abductor pollicis brevis) is very low in amplitude, whereas the median sensory nerve action potential (recording the second digit) is normal. Additionally, the medial antebrachial cutaneous sensory nerve (supplying the medial forearm) action potential is either absent or very low in amplitude.[6][114] The ulnar sensory nerve action potential (recording fifth digit) is slightly to moderately low in amplitude. The electromyogram should evaluate all muscles innervated by cervical nerve roots and the brachial plexus, including paraspinal muscles. Studies should be performed bilaterally for comparison between limbs. Interpreting areas of any abnormality can help identify the area(s) of compression.
Muscle blocks
Targeted muscle blocks can help reinforce the clinical diagnosis of neurogenic TOS and help to predict potential responses to surgical intervention.[1] Positive muscle blocks are a useful adjunct in diagnosis and prognosis of neurogenic TOS but are not a requirement for diagnosis or treatment. Patients with a strong clinical diagnosis of neurogenic TOS and a negative scalene/pectoralis muscle block can still have an excellent response to surgical treatment.[115] Specifically, under electrophysiological or imaging guidance (ultrasound, CT, or MRI), a local anaesthetic solution is injected into the anterior scalene and/or pectoralis minor muscles.[116] Such muscle blocks can provide temporary symptom relief of symptoms if due to brachial plexus compression at the interscalene triangle or the pectoralis minor space, by interrupting muscle spasm. In addition to helping confirm the clinical diagnosis, positive muscle blocks can demonstrate reversibility of symptoms and are thought to predict potential responsiveness to surgical treatment.[117][118]
Scalene/pectoralis minor muscle blocks can be especially useful in high-performance overhead athletes suspected to have neurogenic TOS, with symptoms that arise only while engaged in their sport. Having the athlete undertake sport-related activity immediately following the muscle injection may allow the effects to be assessed more accurately than if only evaluated at rest.[119] Using the EAST following the muscle injection is another way to quantify the results.[120]
Other tests
Full blood count, coagulation, and thrombophilia studies are often performed in patients with venous TOS and in some patients with arterial TOS. These tests include prothrombin time, partial thromboplastin time, INR, antiphospholipid antibodies, and studies for hereditary thrombophilias such as antithrombin-III deficiency, Protein C deficiency, Protein S deficiency, Factor V Leiden mutation, prothrombin G20210A mutation, and methylenetetrahydrofolate reductase (MTHFR) mutation. Such studies can help identify patients with an underlying hypercoagulable state or thrombophilia, which may influence the type and duration of anticoagulation treatment.[121] Importantly, the presence of a thrombophilia or hypercoagulable condition does not necessarily exclude the diagnosis of venous TOS, as both disorders may co-exist.
In suspected neurogenic TOS, it is important to assess the level of functional disability related to upper extremity symptoms, with respect to impact on work, school, recreation, and daily activities, preferably using one or more patient-reported survey instruments by which this can be quantified.[1] The most frequently used instruments are the QuickDASH score (11-item short form of the Disabilities of the Arm, Shoulder, and Hand instrument) and the Cervical-Brachial Symptom Questionnaire (CBSQ).[117][122][123][124] Other patient-reported outcomes measures (PROMs) may also be valuable, including visual analogue scores to measure pain, self-rated depression scores, and quality-of-life measures such as the Short Form Health Survey-12 (SF-12) (with mental and physical components).[122][125][126][127]
Use of this content is subject to our disclaimer