Haemorrhoids
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
initial presentation: non-pregnant
dietary and lifestyle modification
All patients should be offered information about lifestyle and dietary modification, specifically increased fibre intake and adequate fluids.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com
Consuming 25-30 g of fibre daily is recommended, either with high-fibre foods or with commercial fibre supplements, as well as drinking 6-8 glasses of fluids.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com These measures alone may be all that is necessary for those patients with mild symptoms.[12]Moesgaard F, Nielsen ML, Hansen JB, et al. High fiber diet reducing bleeding and pain in patients with hemorrhoids: a double-blind trial of Vi-Siblin. Dis Colon Rectum. 1982 Jul-Aug;25(5):454-6. http://www.ncbi.nlm.nih.gov/pubmed/6284457?tool=bestpractice.com Oral laxatives such as polyethylene glycol or docusate sodium may be given to patients who are unable to increase their dietary fibre intake.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Other basic treatments may include topical treatments and analgesics.[14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com
Straining or spending excessive time at stool should be discouraged.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Moist, gentle cleaning following a bowel movement is advised.
In the presence of suspicious symptoms, such as altered bowel habit (diarrhoea and/or constipation), abdominal pain, weight loss, iron-deficiency anaemia, or passage of blood clots and/or mucus, lower gastrointestinal endoscopy is performed.
rubber band ligation or sclerotherapy or infrared coagulation
Additional treatment recommended for SOME patients in selected patient group
Rubber band ligation is a simple and effective method of managing excess tissue and is the treatment of choice for grade 1 haemorrhoids that are unresponsive to conservative management.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Rubber band ligation is performed with the aid of an anoscope. A rubber band is placed on the redundant haemorrhoidal tissue, with care taken to place the bands above the dentate line. The tissue contained in the band necroses and sloughs in approximately 1 week; success rates for controlling haemorrhoidal disease are good.[15]Wrobleski DE, Corman ML, Veidenheimer MC, et al. Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum. 1980 Oct;23(7):478-82. http://www.ncbi.nlm.nih.gov/pubmed/7438950?tool=bestpractice.com Patients can experience transient bleeding or, extremely rarely, septic events. Anticoagulants should be withheld before performing rubber band ligation, and any bleeding after the procedure should be promptly evaluated.
Sclerotherapy and infrared coagulation can also be performed if grade 1 haemorrhoids are unresponsive to conservative management.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Both have similar effects and may require multiple treatment sessions to successfully ablate the tissue.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx Sclerotherapy and infrared coagulation may be more suitable for haemorrhoids that are too small for rubber band ligation.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com
Sclerotherapy involves injecting a chemical agent directly into the haemorrhoidal tissue to cause local tissue destruction and scarring. With the aid of an anoscope, 2-3 mL of a sclerosant (5% phenol, 5% quinine or urea) is injected into the submucosa of the haemorrhoidal apex.
Infrared coagulation uses infrared radiation applied directly to the haemorrhoid, which causes coagulation, scarring, and subsequent fixation of the internal haemorrhoidal tissue.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx
Both sclerotherapy and infrared coagulation are office procedures and do not require anaesthesia.
rubber band ligation or sclerotherapy or infrared coagulation or haemorrhoidal arterial ligation
Treatment recommended for ALL patients in selected patient group
Rubber band ligation is a simple and effective method of managing excess tissue and is the treatment of choice for grade 2 haemorrhoids that are unresponsive to conservative management.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Sclerotherapy, infrared coagulation, or haemorrhoidal arterial ligation can also be used to treat grade 2 haemorrhoids.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com
Rubber band ligation is performed with the aid of an anoscope. A rubber band is placed on the redundant haemorrhoidal tissue, with care taken to place the bands above the dentate line. The tissue contained in the band necroses and sloughs in approximately 1 week; success rates for controlling haemorrhoidal disease are good.[15]Wrobleski DE, Corman ML, Veidenheimer MC, et al. Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum. 1980 Oct;23(7):478-82.
http://www.ncbi.nlm.nih.gov/pubmed/7438950?tool=bestpractice.com
Patients can experience transient bleeding or, extremely rarely, septic events. Anticoagulants should be withheld before performing rubber band ligation, and any bleeding after the procedure should be promptly evaluated.[Figure caption and citation for the preceding image starts]: Rubber band on redundant haemorrhoidal tissueKurt G. Davis, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Bands placed above the dentate lineKurt G. Davis, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Bands placed above the dentate lineKurt G. Davis, MD [Citation ends].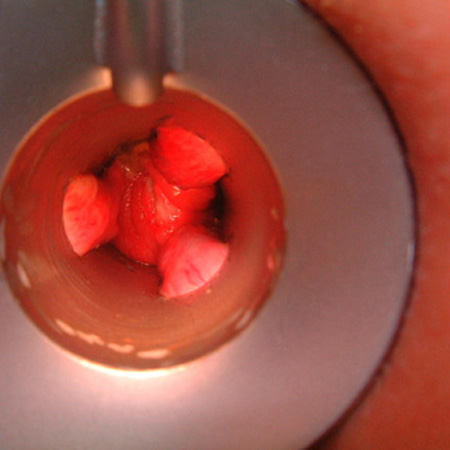 [Figure caption and citation for the preceding image starts]: AnoscopeKurt G. Davis, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: AnoscopeKurt G. Davis, MD [Citation ends].
Sclerotherapy and infrared coagulation may be more suitable for haemorrhoids that are too small for rubber band ligation (which may include grade 1 to 2 haemorrhoids). Both have similar effects and may require multiple treatment sessions to successfully ablate the tissue.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx
Sclerotherapy involves injecting a chemical agent directly into the haemorrhoidal tissue to cause local tissue destruction and scarring. With the aid of an anoscope, 2-3 mL of a sclerosant (5% phenol, 5% quinine or urea) is injected into the submucosa of the haemorrhoidal apex.
Infrared coagulation uses infrared radiation applied directly to the haemorrhoid, which causes coagulation, scarring, and subsequent fixation of the internal haemorrhoidal tissue.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx
Both sclerotherapy and infrared coagulation are office procedures and do not require anaesthesia.
Haemorrhoid artery ligation (also known as transanal haemorrhoidal de-arterialisation) uses a custom-designed proctoscope coupled with a Doppler transducer to identify and ligate the terminal branches of superior rectal artery above the dentate line (resulting in haemorrhoidal shrinkage). The procedure is commonly done under a short general anaesthetic and multiple ligations may be required.[16]Giordano P, Overton J, Madeddu F, et al. Transanal hemorrhoidal dearterialization: a systematic review. Dis Colon Rectum. 2009 Sep;52(9):1665-71. http://www.ncbi.nlm.nih.gov/pubmed/19690499?tool=bestpractice.com [17]Wallis de Vries BM, van der Beek ES, de Wijkerslooth LR, et al. Treatment of grade 2 and 3 hemorrhoids with Doppler-guided hemorrhoidal artery ligation. Dig Surg. 2007;24(6):436-40. https://www.karger.com/Article/FullText/108326 http://www.ncbi.nlm.nih.gov/pubmed/17855782?tool=bestpractice.com Patients with grade 2 or 3 haemorrhoids who were randomised to haemorrhoidal arterial ligation experienced fewer recurrences at 1 year than patients treated with rubber band ligation.[18]Brown S, Tiernan J, Biggs, et al. The HubBLe Trial: haemorrhoidal artery ligation (HAL) versus rubber band ligation (RBL) for symptomatic second- and third-degree haemorrhoids: a multicentre randomised controlled trial and health-economic evaluation. Health Technol Assess. 2016 Nov;20(88):1-150. https://www.journalslibrary.nihr.ac.uk/hta/hta20880/#/abstract http://www.ncbi.nlm.nih.gov/pubmed/27921992?tool=bestpractice.com However, symptom scores and complications did not differ between treatment groups, and patients treated with haemorrhoidal arterial ligation had more early postoperative pain.[18]Brown S, Tiernan J, Biggs, et al. The HubBLe Trial: haemorrhoidal artery ligation (HAL) versus rubber band ligation (RBL) for symptomatic second- and third-degree haemorrhoids: a multicentre randomised controlled trial and health-economic evaluation. Health Technol Assess. 2016 Nov;20(88):1-150. https://www.journalslibrary.nihr.ac.uk/hta/hta20880/#/abstract http://www.ncbi.nlm.nih.gov/pubmed/27921992?tool=bestpractice.com
rubber band ligation or haemorrhoidal arterial ligation or stapled haemorrhoidopexy
Treatment recommended for ALL patients in selected patient group
Rubber band ligation remains a reasonable choice for grade 3 haemorrhoids.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com However, patients with large grade 3 haemorrhoids (in addition to patients refractory to or who cannot tolerate outpatient procedures; patients with large, symptomatic external tags; or patients with grade 4 haemorrhoids) are candidates for surgery (haemorrhoidectomy, stapled haemorrhoidopexy, haemorrhoid artery ligation).[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx
Rubber band ligation is performed with the aid of an anoscope. A rubber band is placed on the redundant haemorrhoidal tissue, with care taken to place the bands above the dentate line. The tissue contained in the band necroses and sloughs in approximately 1 week; success rates for controlling haemorrhoidal disease are good.[15]Wrobleski DE, Corman ML, Veidenheimer MC, et al. Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum. 1980 Oct;23(7):478-82.
http://www.ncbi.nlm.nih.gov/pubmed/7438950?tool=bestpractice.com
Alternatively, rubber bands can be placed at the same time as a colonoscopy.[15]Wrobleski DE, Corman ML, Veidenheimer MC, et al. Long-term evaluation of rubber ring ligation in hemorrhoidal disease. Dis Colon Rectum. 1980 Oct;23(7):478-82.
http://www.ncbi.nlm.nih.gov/pubmed/7438950?tool=bestpractice.com
Patients can experience transient bleeding or, extremely rarely, septic events. Anticoagulants should be withheld before performing rubber band ligation, and any bleeding after the procedure should be promptly evaluated.[Figure caption and citation for the preceding image starts]: Rubber band on redundant haemorrhoidal tissueKurt G. Davis, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Bands placed above the dentate lineKurt G. Davis, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Bands placed above the dentate lineKurt G. Davis, MD [Citation ends].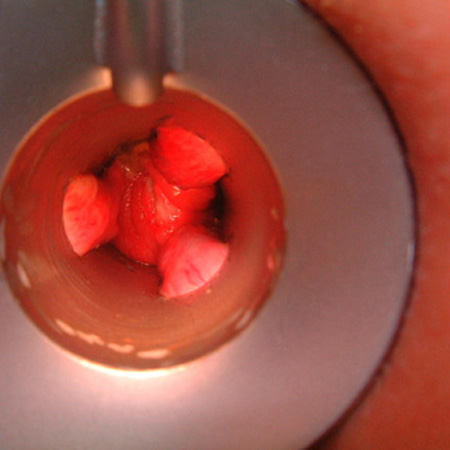 [Figure caption and citation for the preceding image starts]: AnoscopeKurt G. Davis, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: AnoscopeKurt G. Davis, MD [Citation ends].
In a small study of patients with grade 3 or small grade 4 haemorrhoids, rubber band ligation and stapled haemorrhoidopexy (in which prolapsing haemorrhoids are relocated within the anal canal, rather than excised) were equally effective in controlling symptomatic prolapse, but rubber band ligation was associated with an increased risk of recurrent bleeding.[19]Peng BC, Jayne DG, Ho YH. Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Dis Colon Rectum. 2003 Mar;46(3):291-7. http://www.ncbi.nlm.nih.gov/pubmed/12626901?tool=bestpractice.com Stapled haemorrhoidopexy was associated with increased pain and analgesia use at 2-week and at 2-month follow-up; the two treatment groups did not differ with respect to patient satisfaction or quality of life.[19]Peng BC, Jayne DG, Ho YH. Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Dis Colon Rectum. 2003 Mar;46(3):291-7. http://www.ncbi.nlm.nih.gov/pubmed/12626901?tool=bestpractice.com However, guidelines recommend against routine use of stapled haemorrhoidopexy as a first-line surgical option due to an increased risk of complications and recurrence.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx Patients should be informed of the potential for symptomatic recurrence following stapled haemorrhoidopexy.[20]Acheson AG, Scholefield JH. Management of haemorrhoids. BMJ. 2008 Feb 16;336(7640):380-3. http://www.ncbi.nlm.nih.gov/pubmed/18276714?tool=bestpractice.com [21]Jayaraman S, Colquhoun PH, Malthaner RA. Stapled versus conventional surgery for hemorrhoids. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD005393. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005393.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/17054255?tool=bestpractice.com
surgical haemorrhoidectomy
Treatment recommended for ALL patients in selected patient group
Surgical haemorrhoidectomy is the most effective first-line approach for grade 4 internal haemorrhoids.[13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com One network meta-analysis that included patients undergoing elective surgery for grade 3 to 4 haemorrhoids found that conventional haemorrhoidectomy was associated with greater postoperative pain but fewer haemorrhoid recurrences than stapled haemorrhoidopexy.[22]Simillis C, Thoukididou SN, Slesser AA, et al. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg. 2015 Dec;102(13):1603-18. http://www.ncbi.nlm.nih.gov/pubmed/26420725?tool=bestpractice.com A large, open-label pragmatic trial of 777 patients referred to hospital for surgical treatment of haemorrhoids (including grade 4) found that patients who received stapled haemorrhoidopexy had less short-term pain.[24]Watson AJ, Hudson J, Wood J, et al. Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): a pragmatic, multicentre, randomised controlled trial. Lancet. 2016 Nov 12;388(10058):2375-85. http://www.ncbi.nlm.nih.gov/pubmed/27726951?tool=bestpractice.com [25]Watson AJ, Cook J, Hudson J, et al. A pragmatic multicentre randomised controlled trial comparing stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease: the eTHoS study. Health Technol Assess. 2017 Nov;21(70):1-224. https://www.journalslibrary.nihr.ac.uk/hta/hta21700#/full-report http://www.ncbi.nlm.nih.gov/pubmed/29205150?tool=bestpractice.com However, recurrence rates, symptoms, re-interventions and quality-of-life measures all favoured traditional haemorrhoidectomy.[24]Watson AJ, Hudson J, Wood J, et al. Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): a pragmatic, multicentre, randomised controlled trial. Lancet. 2016 Nov 12;388(10058):2375-85. http://www.ncbi.nlm.nih.gov/pubmed/27726951?tool=bestpractice.com [25]Watson AJ, Cook J, Hudson J, et al. A pragmatic multicentre randomised controlled trial comparing stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease: the eTHoS study. Health Technol Assess. 2017 Nov;21(70):1-224. https://www.journalslibrary.nihr.ac.uk/hta/hta21700#/full-report http://www.ncbi.nlm.nih.gov/pubmed/29205150?tool=bestpractice.com
For external haemorrhoids, or combined internal and external haemorrhoids with severe symptoms, surgical excision may be the only effective treatment option. This involves excision under either a general or regional anaesthetic. Asymptomatic external haemorrhoids do not warrant invasive treatment but may be observed while the patient follows dietary and lifestyle modification.
In thrombosis of external haemorrhoids, minimally invasive procedures such as de-roofing may be required for symptom relief, which can be done under topical, regional, or general anaesthetic.
Early haemorrhoidectomy is likely to increase speed of symptom resolution, reduce the chance of recurrence, and provide longer periods of remission compared to conservative management alone.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [28]Greenspon J, Williams SB, Young HA, et al. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004 Sep;47(9):1493-8. http://www.ncbi.nlm.nih.gov/pubmed/15486746?tool=bestpractice.com
initial presentation: pregnant
dietary and lifestyle modification
All patients should be offered information about lifestyle and dietary modification, specifically increased fibre intake, adequate fluids, and not straining or spending excessive time sitting at stool.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com Moist, gentle cleaning following a bowel movement is advised. These measures alone may be all that is necessary for those patients with mild symptoms.[12]Moesgaard F, Nielsen ML, Hansen JB, et al. High fiber diet reducing bleeding and pain in patients with hemorrhoids: a double-blind trial of Vi-Siblin. Dis Colon Rectum. 1982 Jul-Aug;25(5):454-6. http://www.ncbi.nlm.nih.gov/pubmed/6284457?tool=bestpractice.com
A non-operative approach is recommended during pregnancy, with basic treatment including laxatives, topical treatments, and analgesics.[2]Gallo G, Martellucci J, Sturiale A, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol. 2020 Feb;24(2):145-64. https://link.springer.com/article/10.1007/s10151-020-02149-1 http://www.ncbi.nlm.nih.gov/pubmed/31993837?tool=bestpractice.com [14]van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology: guideline for haemorrhoidal disease. Colorectal Dis. 2020 Jun;22(6):650-62. http://www.ncbi.nlm.nih.gov/pubmed/32067353?tool=bestpractice.com
Pregnant and postnatal women have a higher incidence of haemorrhoids, but symptoms typically resolve spontaneously after birth.[29]Staroselsky A, Nava-Ocampo AA, Vohra S, et al. Hemorrhoids in pregnancy. Can Fam Physician. 2008 Feb;54(2):189-90. https://www.cfp.ca/content/54/2/189.long http://www.ncbi.nlm.nih.gov/pubmed/18272631?tool=bestpractice.com
surgical haemorrhoidectomy
Additional treatment recommended for SOME patients in selected patient group
Surgery is rarely an appropriate intervention for pregnant women as haemorrhoidal symptoms often resolve spontaneously after birth, but it may be considered in extreme circumstances.[29]Staroselsky A, Nava-Ocampo AA, Vohra S, et al. Hemorrhoids in pregnancy. Can Fam Physician. 2008 Feb;54(2):189-90. https://www.cfp.ca/content/54/2/189.long http://www.ncbi.nlm.nih.gov/pubmed/18272631?tool=bestpractice.com [30]De Schepper H, Coremans G, Denis MA, et al. Belgian consensus guideline on the management of hemorrhoidal disease. Acta Gastroenterol Belg. 2021 Jan-Mar;84(1):101-20. https://www.ageb.be/ageb-journal/ageb-volume/ageb-article/1884 http://www.ncbi.nlm.nih.gov/pubmed/33639701?tool=bestpractice.com
treatment failure of rubber band ligation, sclerotherapy, infrared coagulation, haemorrhoidal arterial ligation, or stapled haemorrhoidopexy
surgical haemorrhoidectomy
Surgical haemorrhoidectomy is the best treatment for patients with combined internal and external haemorrhoids or for any patient who has failed conservative treatment options for their internal haemorrhoids. Early haemorrhoidectomy is likely to increase speed of symptom resolution, reduce the chance of recurrence, and provide longer periods of remission compared to conservative management alone.[1]Wald A, Bharucha AE, Limketkai B, et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol. 2021 Oct 1;116(10):1987-2008. https://journals.lww.com/ajg/Fulltext/2021/10000/ACG_Clinical_Guidelines__Management_of_Benign.13.aspx http://www.ncbi.nlm.nih.gov/pubmed/34618700?tool=bestpractice.com [13]Hawkins AT, Davis BR, Bhama AR, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2024 May 1;67(5):614-23. https://journals.lww.com/dcrjournal/fulltext/2024/05000/the_american_society_of_colon_and_rectal_surgeons.5.aspx [28]Greenspon J, Williams SB, Young HA, et al. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004 Sep;47(9):1493-8. http://www.ncbi.nlm.nih.gov/pubmed/15486746?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer