Approach
Characteristic features of symptomatic internal haemorrhoids are painless, bright red bleeding and intermittent protrusion from the rectum, which often follow a bowel movement.[1][13] Pain may accompany complication of haemorrhoids. The presence of altered bowel habit (diarrhoea and/or constipation), abdominal pain, weight loss, iron-deficiency anaemia, or passage of blood clots and/or mucus (especially if persistent) should arouse suspicion of other potential diagnoses such as anal fissure, anal fistula, proctitis, inflammatory bowel disease, or colorectal cancer.
Physical examination
Physical examination of the anorectal canal should be performed in the left lateral position (Sims), the prone jack-knife position, or the lithotomy position (also called the knee-chest position).[2][14] Examination should be approached very carefully, particularly if pain is the primary complaint. It begins with a visual inspection of the anal margin by gently spreading the buttocks, looking for external haemorrhoids, skin tags, or other anal pathology such as anal fissures, fistulas, or perianal masses. A prolapse may be made more visible if the patient is asked to strain. Assessment of the type of prolapse should allow the examiner to distinguish a haemorrhoidal prolapse (radial pattern) from a rectal prolapse (concentric pattern).
[Figure caption and citation for the preceding image starts]: Complete rectal prolapse with a concentric fold pattern (A, B) and prolapsed internal haemorrhoids with a radial fold pattern (C)Meher S. Pan Afr Med J. 2016 May 27; 24: 88; used with permission [Citation ends].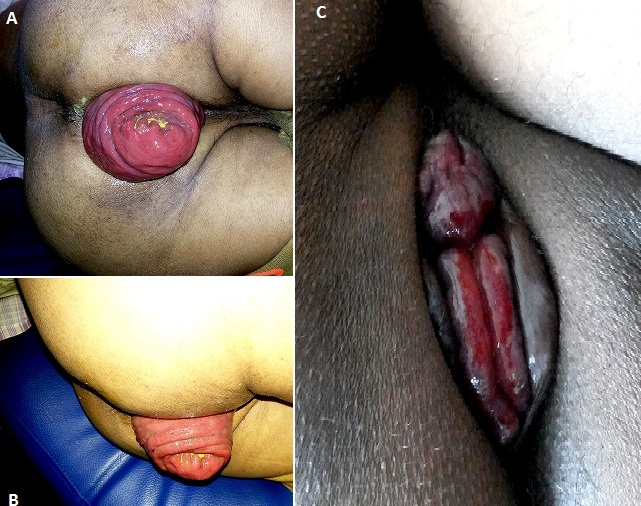
Unless the patient is in a lot of pain, a digital examination and an anoscopic examination can then be performed with either a lighted anoscope or an external light source.[13]
The anoscopic examination is a simple and safe technique, which enables a full view of the anal canal and all of the haemorrhoidal tissue. The alternative technique of using a retroflexed flexible endoscope is technically more demanding and requires a higher skill level.
Endoscopy
It is imperative to exclude serious or concomitant conditions of the colon and rectum (such as inflammatory bowel disease or colon cancer), especially in the presence of suspicious symptoms such as altered bowel habit (diarrhoea and/or constipation), abdominal pain, weight loss, iron-deficiency anaemia, or passage of blood clots and/or mucus (although it is safe to initiate first-line treatment for any obvious haemorrhoids).[13] Further investigations to exclude such conditions may include a flexible endoscopy¸ which can be either a limited colonoscopy (flexible sigmoidoscopy, performed following 1-2 enemas) or a full colonoscopy (after a full bowel preparation), depending on the patient’s age and risk profile.[2] Criteria for a complete colon evaluation include age ≥50 years, family history of colorectal cancer, and positive fecal immunochemical testing. See also Colorectal cancer (Screening).
Laboratory
A full blood count can be ordered if there is concern that the patient has experienced significant and prolonged rectal bleeding and if signs of anaemia are present. If microcytic or hypochromic anaemia is detected, further investigations such as a gastroscopy and full colonoscopy are warranted to determine the cause of anaemia.[2]
A stool test for occult haem, such as the fecal immunochemical test, is usually unnecessary if visible bleeding is reported. However, if no significant haemorrhoidal tissue is seen on examination and there is frank or occult evidence of bleeding, further investigations such as endoscopy are warranted to determine the source of bleeding.
Use of this content is subject to our disclaimer