Investigations
1st investigations to order
plasma free metanephrines or 24-hour urine fractionated metanephrines and normetanephrines
Test
Measurement of plasma free metanephrines (also known as metadrenalines), or 24-hour urine fractionated metanephrines and normetanephrines (also known as normetadrenaline), is recommended in patients with suspected phaeochromocytoma.[26][46]
Blood sampling should be performed in the supine position.[47]
When measuring 24-hour urinary excretion, creatinine is measured to ensure the adequacy of the collection.
Some drugs may interfere with testing results (e.g., buspirone, cocaine, labetalol, levodopa, methyldopa, monoamine oxidase inhibitors [MAOIs], paracetamol, phenoxybenzamine, sotalol, sulfasalazine, sympathomimetics, tricyclic antidepressants); review patient drug history accordingly.[46]
Result
elevations 3 times above the upper limit of normal are diagnostic
genetic testing
Test
All patients with phaeochromocytomas should undergo genetic testing to identify potential hereditary tumour disorders that would necessitate more detailed evaluation and follow-up.[1][26][46][47][53] Patient engagement in a shared decision-making process is essential.[46]
Genetic testing may be guided by features such as a positive family history (premised upon pedigree or identification of a PPGL-susceptibility gene mutation); syndromic features; multifocal, bilateral, or metastatic disease.[3]
Result
may reveal familial disorders responsible for phaeochromocytoma such as Von Hippel-Lindau syndrome (VHL), multiple endocrine neoplasia type 2 (MEN2), or neurofibromatosis type 1 (NF1); other described gene mutations include SDHB, SDH complex assembly factor 2 (SDHAF2), transmembrane protein 127 (TMEM 127), SDH subunit A, MYC-associated factor X (MAX), and hypoxia-inducible factor 2-alpha (HIF2A)
Investigations to consider
FBC
Test
Erythrocytosis is a rare finding, secondary to overproduction of erythropoietin.[57]
Result
may reveal erythrocytosis
serum calcium
Test
Hypercalcaemia may be seen in patients with multiple endocrine neoplasia 2 (MEN2) who have concomitant primary hyperparathyroidism.
Result
may reveal hypercalcaemia
serum potassium
Test
Hypokalaemia can be seen in the setting of high catecholamines.
Result
may reveal hypokalaemia
chromogranin A
Test
Chromogranin A may be elevated in patients with a neuroendocrine tumour.
Reported sensitivity of 83% and specificity of 96% for identifying a phaeochromocytoma.[58]
Chromogranin A plus urinary fractionated metanephrines (also known as metadrenalines) has been suggested as a follow-up test for elevations of plasma metanephrines.[49]
Chromogranin A can be used as a screening tool to detect recurrence, especially in patients with normal preoperative metanephrine and normetanephrine (also known as normetadrenaline) levels.[53]
Result
elevated in patients with phaeochromocytomas and multiple other neuroendocrine tumours
clonidine suppression test
Test
Discriminates patients with mildly elevated test results for plasma normetanephrine (also known as normetadrenaline; attributable to increased sympathetic activity) from those with elevated test results due to a phaeochromocytoma or paraganglioma.[47][48]
Used when potential for false-positive urine or serum studies (metanephrines [also known as metadrenalines]/normetanephrines) is high (e.g., patients with decreased renal excretory function, in acute alcohol withdrawal, or if the patient is taking hydralazine or minoxidil).
Plasma metanephrine and normetanephrine levels are taken both before and after administration of clonidine.[48][59] Consult your local drug information source for guidance on dose.
Clonidine is a centrally acting alpha-2-adrenergic receptor agonist that suppresses the release of catecholamines from neurons; however, it does not affect catecholamine secretion from a phaeochromocytoma.
Result
lack of suppression of catecholamines
CT scan of the abdomen and pelvis
Test
Anatomical imaging (with CT, MRI, or both) is critical for surgical planning and should be performed for every patient.[24]
CT imaging is preferred.[46]
CT can detect adrenal phaeochromocytomas as small as 0.5 cm and extra-adrenal disease >1 cm in diameter. [Figure caption and citation for the preceding image starts]: Abdominal CT scan with mass in the left adrenal gland, compatible with a phaeochromocytomaAlface MM et al. BMJ Case Rep. 2015 Aug 4;2015:bcr2015211184; used with permission [Citation ends].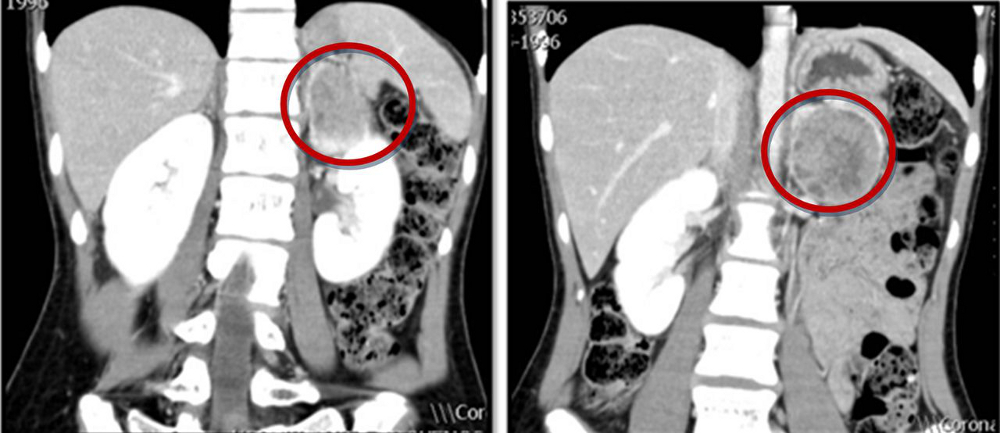
Localisation studies should only be undertaken after a biochemical abnormality is demonstrated.
Result
inhomogeneous masses, often with a central area of low attenuation that represents haemorrhage or necrosis; the attenuation values are greater than 10 HU on unenhanced images
MRI of the abdomen and pelvis
Test
Anatomical imaging (with CT, MRI, or both) is critical for surgical planning and should be performed for every patient.[24]
MRI is an option for patients in whom radiation exposure should be limited or is contraindicated (e.g., children, pregnant or lactating women).[46]
MRI may be considered in patients with suspected metastatic phaeochromocytoma or paraganglioma; it can detect blood vessel invasion and liver metastases with greater sensitivity than CT.[26]
Localisation studies should only be undertaken after a biochemical abnormality is demonstrated.
Result
typically appear hyper-intense to the liver on T2-weighted images because of their high water content
18F-fluorodeoxyglucose (18F-FDG) PET/CT or somatostatin receptor-targeted (SSTR) PET/CT with 68Ga-DOTATATE tracer
Test
Anatomical imaging should be complemented by functional imaging unless risk of tumour metastases or multifocal disease is low (i.e., those without previous phaeochromocytoma or paraganglioma [PPGL] and hereditary syndrome, with an adrenergic biochemical phenotype and a single small adrenal phaeochromocytoma [<5 cm]).[50]
Functional imaging can improve detection when anatomical localisation is inconclusive, identify additional lesions in the setting of hereditary disease, and evaluate for metastatic disease.[51] The North American Neuroendocrine Tumor Society recommends SSTR PET/CT as first-line functional imaging when metastatic PPGL is suspected.[26]
18F-FDG PET/CT, and SSTR PET/CT with 68Ga-DOTATATE tracer (also known as PET/CT Ga-68 DOTATATEe scan), are more sensitive than I-123 metaiodobenzylguanidine (MIBG) scintigraphy in the setting of metastatic and multifocal phaeochromocytoma.[26][46] SSTR PET/CT with 68Ga DOTATATE is highly sensitive, and often the preferred imaging modality for the detection and localisation of phaeochromocytoma in patients with SDHB-associated metastatic disease.[52]
Result
uptake of 18F-FDG is high in catecholamine-producing tissues on 18F-FDG PET/CT; uptake of 68Ga-DOTATATE is high in tissues expressing somatostatin receptors (e.g., paraganglioma) on SSTR PET/CT with 68Ga-DOTATATE tracer
I-123 metaiodobenzylguanidine (MIBG) scintigraphy
Test
Anatomical imaging should be complemented by functional imaging unless risk of tumour metastases or multifocal disease is low (i.e., those without previous phaeochromocytoma or paraganglioma [PPGL] and hereditary syndrome, with an adrenergic biochemical phenotype and a single small adrenal phaeochromocytoma [<5 cm]).[50]
Functional imaging can improve detection when anatomical localisation is inconclusive, identify additional lesions in the setting of hereditary disease, and evaluate for metastatic disease.[51]
An I-123 MIBG scan is required if treatment with I-131 MIBG is being considered (e.g., patients with inoperable PPGL).[46][50]
I-123 MIBG scintigraphy is not recommended as a first-choice functional imaging study.[50]
[Figure caption and citation for the preceding image starts]: Metaiodobenzylguanidine (MIBG) scintigraphy identified hyperfixation in the left adrenal gland compatible with phaeochromocytomaAlface MM et al. BMJ Case Rep. 2015 Aug 4;2015:bcr2015211184; used with permission [Citation ends].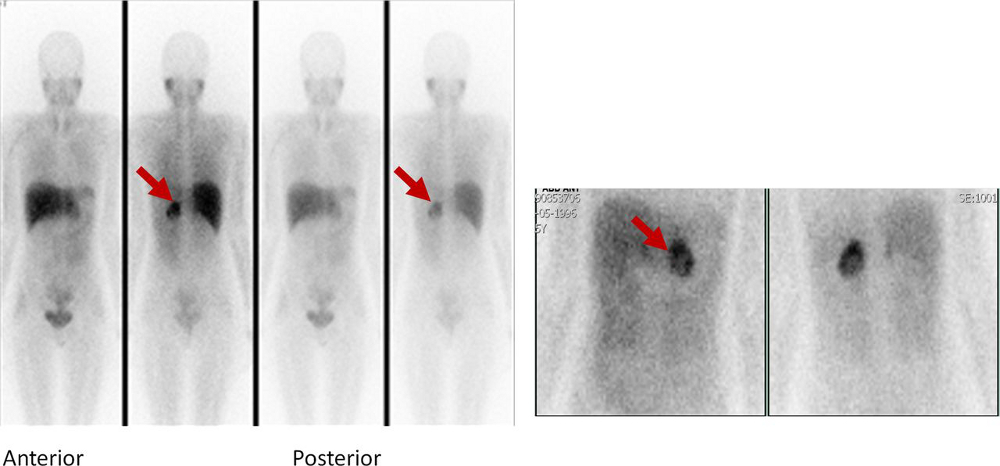
Result
I-123 MIBG uptake intensity is high in catecholamine-producing tissues
Use of this content is subject to our disclaimer