Differentials
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Aanhoudende hoest bij kinderen in de eerste lijnPublished by: Werkgroep Ontwikkeling Richtlijnen Eerste Lijn (Worel)Last published: 2017La toux prolongée chez l’enfant en première ligne de soinsPublished by: Groupe de Travail Développement de recommmandations de première ligneLast published: 2017Asthma
SIGNS / SYMPTOMS
Dyspnoea, expiratory wheeze, nasal polyposis.
INVESTIGATIONS
spirometry may show evidence of impaired lung function (FEV₁ <80% of predicted; FEV₁/FVC ratio <80% of predicted); peak expiratory flow shows >20% variability; fractional exhaled nitric oxide >40 parts per billion (ppb) in a corticosteroid-naive adult; methacholine bronchial challenge test may be useful in excluding asthma.
Bronchiectasis
SIGNS / SYMPTOMS
Sputum production (may be bloody), haemoptysis, dyspnoea, fever, crackles or rhonchi on lung auscultation.
INVESTIGATIONS
Chest x-ray may be normal or show obscured haemidiaphragm, thin-walled ring shadows with or without fluid levels, tram lines, or tubular or ovoid opacities.
Gastro-oesophageal reflux disease
SIGNS / SYMPTOMS
Heartburn, indigestion, cough with phonation, on eating, on bending over, or on first becoming ambulatory in the morning; may coexist with upper airway cough syndrome (UACS).
INVESTIGATIONS
Proton-pump inhibitor trial relieves symptoms; atypical symptoms (e.g., hoarseness) warrant further investigation (e.g., endoscopy may show oesophagitis).
COPD
SIGNS / SYMPTOMS
History of smoking.
Dyspnoea that occurs with or without wheezing and coughing.
Examination may show barrel chest, hyper-resonance to percussion, and distant breath sounds.
INVESTIGATIONS
FEV₁/FVC<0.7; low oxygen saturation on pulse oximetry; FBC may show polycythaemia (haematocrit >55%), anaemia, and leukocytosis; chest x-ray shows hyperinflation.
Other causes of chronic cough
SIGNS / SYMPTOMS
Includes interstitial lung disease, ACE inhibitor use, and eosinophilic bronchitis.
Symptoms vary depending on the condition.
Interstitial lung disease: fatigue, weight loss, dyspnoea, crackles on lung auscultation.
ACE inhibitor use: Dry cough beginning within days/month of starting ACE inhibitor therapy, tickling/scratching sensation in the throat.
Non-asthmatic eosinophilic bronchitis: chronic non-productive cough.
INVESTIGATIONS
Interstitial lung disease: chest x-ray shows basilar, peripheral, bilateral, asymmetric, or reticular opacities.
ACE inhibitor use: Resolution of cough on stopping ACE inhibitor.
Non-asthmatic eosinophilic bronchitis: eosinophilia on broncho-alveolar lavage (BAL) differential count; fractional exhaled nitric oxide raised; therapeutic response to corticosteroids present.
Allergic rhinitis
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Rhinorrhoea/persistent clear nasal discharge.
Sneezing.
Intermittent nasal blockage.
Nasal pruritus.
Conjunctivitis.
Unilateral nasal symptoms, facial pain, thick green discharge, recurrent nosebleeds, or persistent loss of smell warrant further assessment.[36]
INVESTIGATIONS
Allergen skin-prick testing: wheal and flare reaction after specific allergen is introduced into the skin.
Specific aeroallergen radioallergosorbent test (RAST): positive.
These tests can establish the presence of atopy; however, it can be difficult to be certain that the chronic cough in UACS is arising from an allergic mechanism.
Non-allergic rhinitis (perennial)
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Occupational exposure or exposure to physical irritants.
Profound rhinorrhoea.
Unilateral nasal symptoms, facial pain, thick green discharge, nosebleeds, or loss of smell warrant further assessment.[36]
INVESTIGATIONS
Allergen skin-prick testing: negative.
Non-allergic rhinitis with eosinophilia (NARES)
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Nasal pruritus.
Ocular pruritus.
Excessive lacrimation.
INVESTIGATIONS
Nasal eosinophil smear: elevated.
Rhinitis medicamentosa
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
History of extended use of topical decongestants.
INVESTIGATIONS
No differentiating tests; diagnosis is clinical.
Rhinitis of pregnancy
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Pregnant.
INVESTIGATIONS
No differentiating tests; diagnosis is clinical.
Nasal polyps
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Chronic rhinosinusitis.
Nasal obstruction.
Nasal discharge.
Facial pain/pressure.
Loss or decreased sense of smell.
INVESTIGATIONS
Anterior rhinoscopy or nasal endoscopy: polyps visualised.
Chronic rhinosinusitis without nasal polyps
SIGNS / SYMPTOMS
Can coexist with upper airway cough syndrome (UACS) or be an exacerbating factor.
Facial pain/pressure.
Nasal obstruction.
Nasal discharge.
Headache.
May be clinically silent.
INVESTIGATIONS
CT sinus: opacification of involved sinuses, mucosal thickening, air-fluid levels, or anatomical abnormalities.[Figure caption and citation for the preceding image starts]: CT sinus demonstrating opacification.Image courtesy of Mr Hesham Saleh; used with permission [Citation ends].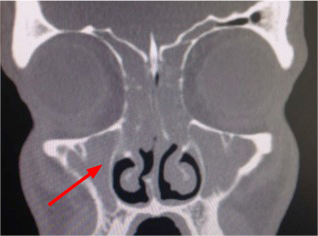
Use of this content is subject to our disclaimer