Investigations
1st investigations to order
CXR
Test
CXR is appropriate for initial imaging, but it is typically more useful in the differential diagnosis.[43]
Guidelines recommend CXR for patients with relevant symptoms and signs (e.g., dyspnoea, chest pain, and weight loss).[43][44][45][46]
CXR use is limited by poor visualisation of the pleura (that will miss subtle abnormalities).[43]
Result
unilateral pleural effusion, irregular pleural thickening, reduced lung volumes, and/or parenchymal changes related to asbestos exposure (e.g., lower zone linear interstitial fibrosis)
CT chest and upper abdomen (with contrast)
Test
If clinical suspicion is high, CT scan with intravenous contrast should be obtained for diagnosis and initial staging of mesothelioma.[44][46][47]
CT with contrast is more sensitive than CXR or CT without contrast, and provides greater detail of the pleura, lungs, and mediastinum.[43][44][47][48]
Differentiating benign from malignant pleural abnormalities with CT alone is not reliable.[Figure caption and citation for the preceding image starts]: Computed tomography scan of the lung showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].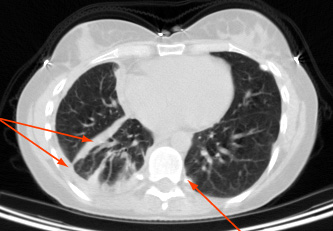 [Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].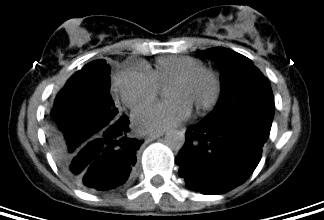
Result
pleural thickening and/or discrete pleural plaques, pleural and/or pericardial effusions; enlarged hilar and/or mediastinal lymph nodes; chest wall invasion and/or spread along needle tracts can occur
Investigations to consider
thoracentesis
Test
A thoracentesis is performed when a patient presents with clinically symptomatic pleural effusion or imaging studies confirm pleural effusion, with or without other pleural abnormalities.
The sensitivity of cytology for mesothelioma is relatively low and typically requires further pathological assessments.[52]
Video demonstrating how to perform a pleural aspiration
Result
exudate; may show malignant cells within the pleural fluid
PET/CT scan
Test
Used to help with initial staging and in the evaluation of pleural metastases.[43][47] PET/CT can distinguish benign pleural abnormalities from malignant processes.[50]
When performed from the skull base to upper thighs, PET/CT can help define the extent of intrathoracic and mediastinal disease and can detect any regional or distant metastases.[43][47][Figure caption and citation for the preceding image starts]: Positron emission tomography scan showing hypermetabolic right-sided pleural mesotheliomaFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
Can be omitted when surgical resection is not being considered.[47]
Result
evaluates location and extent of primary tumour; evaluates for distant metastases
pleural biopsy
Test
Biopsies improve clinical staging, confirm the histological diagnosis and subtype (epithelioid, sarcomatoid, biphasic), and provide material for further studies, such as molecular profiling.[47]
Cytology of pleural fluid obtained via transthoracic needle aspiration biopsy (typically using CT guidance) facilitates pathological confirmation of malignancy. This is not, however, as reliable for diagnosis as a tissue core specimen. Pleural biopsies performed during video-assisted thoracoscopic surgery (VATS) exploration are recommended.[45][47]
When performing a biopsy, aim to do so at the site intended for subsequent definitive resection to reduce the risk of implantation in the chest wall.[47]
Biopsy three distant sites when possible.[45]
Open pleural biopsy, using the smallest incision possible (ideally ≤6 cm), is reserved for when the thoracoscopic approach is not possible.[47]
Result
specimen for pathological diagnosis
video-assisted thoracoscopic surgery (VATS)
Test
VATS is used to evaluate the pleural lining of the lung and to obtain optimal biopsies.[45][47] Aim to limit the number of incisions to less than two.[47] When initial PET/CT or CT suggests contralateral disease, thoracoscopic biopsy can be used for confirmation.[47]
When performing a biopsy, aim to do so at the site intended for subsequent definitive resection to reduce the risk of implantation in the chest wall.[47]
Biopsy three distant sites when possible.[45]
Open pleural biopsy, using the smallest incision possible (ideally ≤6 cm), is reserved for when the thoracoscopic approach is not possible.[47]
Result
pleural thickening or discrete plaques; lymphadenopathy
immunohistochemistry
Test
Recommended for pathological diagnoses of all primary diagnoses.[44][47]
Studies should use selected immunohistochemistry markers expected to be positive in mesothelioma (i.e., calretinin, cytokeratin 5/6, D2-40, and nuclear WT1), and markers expected to be negative in mesothelioma (i.e., carcinoembryonic antigen [CEA], claudin 4, and thyroid transcription factor-1 [TTF-1]).[2][53][54]
Other immunohistochemistry markers can be used to help exclude differential diagnoses, diagnose mesothelioma, or guide prognosis (e.g., BAP1, MTAP, CDKN2A/p16).[2][47]
Result
positive results for certain markers (i.e., calretinin, cytokeratin 5/6, D2-40, and nuclear WT1) make mesothelioma more likely; positive results for other markers (i.e., CEA, claudin 4, TTF-1) make mesothelioma less likely; patients with an epithelioid mesothelioma subtype, together with loss of BAP1 and retained p16 expression, have prolonged survival
germline testing
Test
All patients with mesothelioma should be offered germline testing with appropriate pretest genetic counselling.[47]
Pathogenic or likely pathogenic germline variants in BAP1 are associated with improved survival in patients with mesothelioma.[2][47]
BAP1 a tumour suppressor, is implicated in the pathogenesis of not only mesothelioma but also uveal melanoma, cholangiocarcinoma, and clear cell renal cell carcinoma.[2][47] Patients with a positive germline testing result should be screened for these secondary cancers and their relatives should be offered genetic counselling.[2][47]
Result
positive for BAP1; other genes of interest should be assessed based on local policies
chest MRI
Test
Not recommended for initial imaging. Chest MRI, preferably with intravenous contrast, is used to resolve ambiguous findings on CT and to assess tumour invasion into the diaphragm, chest wall, mediastinum, and other areas.[43][47][51]
MRI can differentiate between benign fibrous mesothelioma (low signal intensity on T2-weighted images) and pleural mesothelioma (high signal intensity).
MRI is not as reliable as biopsy and will seldom alter management.
Result
degree of tumour extension, especially to the chest wall and diaphragm
cervical mediastinoscopy
Test
Mediastinoscopy, especially in patients with abnormal lymph nodes on CT scan or PET, should be considered before surgery.
Mediastinal (N2) lymph node involvement is a poor prognostic factor; these patients are not ideal candidates for aggressive multimodality therapy.[58]
Result
spread to mediastinal lymph nodes
pulmonary function tests
Test
FEV1 and diffusion capacity of lung for carbon monoxide (DLCO) should be performed on all patients with mesothelioma who are being evaluated for surgery. Patients with marginal function can be further assessed with radionuclide studies as needed.
In general, postoperative FEV1 and DLCO should be >40% of predicted values.
Spirometry is a sensitive predictor of postoperative complications after thoracotomy.
Result
spirometry and lung volumes
FBC
Test
Baseline blood counts are necessary before treatment is initiated or invasive procedures are performed.
Chemotherapy, and to a lesser degree radiotherapy, can decrease haematopoiesis, necessitating baseline and periodic analysis of blood counts.
Result
usually normal; low haemoglobin, high platelet count, high white blood cell count are usually found in advanced disease and are poor prognostic factors
basic metabolic panel
Test
Recommended as baseline before treatment is initiated.
Some chemotherapy agents, cisplatin in particular, can affect electrolytes and kidney function.
Result
usually normal
Emerging tests
diagnostic biomarkers
Test
Soluble mesothelin-related peptide (SMRP) levels may correlate with disease status and survival.[2][59]
However, potential diagnostic biomarkers, including SMRP, cannot be used alone to confirm pleural mesothelioma.[44][45][55][56]
Research into potential diagnostic and prognostic biomarkers is ongoing.
Result
positive for marker
Use of this content is subject to our disclaimer
