Approach
Sialadenitis is an umbrella term for inflammation of one of the salivary glands, most commonly the parotid or submandibular. The history, symptoms, signs, and investigations required depend on the nature of the presentation, the gland affected, and any underlying contributing conditions, such as an autoimmune disease or sialoliths. Sialadenitis may present with airway compromise due to swelling of the affected gland, particularly the submandibular. Features of airway compromise may include stridor, use of accessory muscles, nasal flaring, wheeze, and increased respiratory rate. This requires prompt recognition and intervention to protect and secure the airway.
History and examination
Patients with acute bacterial sialadenitis may relate a history of a recent surgical intervention or use of medications such as antihistamines, antidepressants, or anticholinergic agents. These medications may lead to objective hypofunction or the subjective feeling of a dry mouth (xerostomia) but without hypofunction. There may be a history of volume depletion secondary to systemic disease.
Physical examination may reveal unilateral or bilateral painful swelling of the parotid or submandibular regions. Typical external displacement of the earlobe adjacent to an inflamed parotid gland may also be observed. Pus exiting from major salivary gland ductal orifices may occur either spontaneously or after manipulation of the affected gland. There may be associated dysphagia. Mandibular trismus is a rare finding but may be present with large swellings. Fever may be noted in acute bacterial sialadenitis. Spiking temperatures raise the suspicion of abscess formation. Cranial nerves VII (facial), IX (glossopharyngeal), and XII (hypoglossal) should be examined for any deficit that may occur if the swelling is significant.
If chronic recurrent episodes occur, underlying Sjogren syndrome or ductal abnormalities may be responsible.[13][20][14] The author indicates that in practice a patient may report a prodrome of tingling in the gland preceding pain and swelling in chronic recurrent episodes.
The formation of sialoliths can result in the development of obstructive sialadenitis. Sialoliths are usually asymptomatic until they reach a critical size that interferes with salivary output. Around 80% to 90% of salivary stones occur in the submandibular gland. Most of the remaining stones occur in the parotid gland. Sublingual stones are uncommon.[2] There is usually a history of abrupt episodic painful swelling of the parotid or submandibular gland. Episodes typically occur around meal times, last for 2 to 3 hours, and gradually subside.[31] If left untreated, more frequent episodes may occur. Alternatively, the swelling may not completely subside. The association of symptoms with eating is variable; therefore, a high index of clinical suspicion is required.
Autoimmune sialadenitis is characterised by persistent, indolent, and usually asymptomatic bilateral swelling of parotid glands, and may represent the first manifestation of more widespread systemic disease. Patients may complain of dry eyes and dry mouth (typical symptoms of Sjogren syndrome) and may have a concomitant connective tissue disease (e.g., SLE, rheumatoid arthritis, or scleroderma). It may also underlie repeated episodes of acute bacterial sialadenitis.[14] Oral candidiasis may be present.
Chronic sclerosing sialadenitis typically presents in a submandibular gland as a unilateral swelling that cannot be differentiated clinically from a neoplasm. Pain is an inconsistent finding.[32][33]
Subacute necrotising sialadenitis is a rare condition that may present with a unilateral or bilateral swelling on the palate that is usually painful.[34] It is described as being of sudden onset and may be ulcerated.
Investigations
In the acute presentation, pus swabs should be taken if there is any exudate from salivary ductal orifices. Imaging of all patients is recommended to exclude an obstructing sialolith or evolving abscess. Plain dental radiographs are the investigation of choice if a sialolith is suspected. CT imaging is recommended if plain radiographic films are negative. Sialography can be used in combination with CT when sialolithiasis, ductal strictures, or loss of parenchymal integrity is suspected. If an abscess is suspected, ultrasonography is a useful initial investigation. If a sialolith is visualised, referral to a head and neck specialist (such as an oral and maxillofacial surgeon) for further management is advised.[22][20] FBC is usually measured to evaluate the WBC count, which is typically raised in the presence of infection. If fever is present, blood cultures are advised to direct antibiotic therapy. If recurrent episodes occur, investigations for ductal abnormalities and Sjogren syndrome are recommended.
Sjogren syndrome can be confirmed by serum studies to look for the presence of circulating antinuclear antibodies (SSA/anti-Ro and SSB/anti-La), which are pathognomonic for Sjogren syndrome. Elevated titres of antinuclear antibodies and rheumatoid factor may also be present. Salivary gland biopsy will reveal the histopathological findings associated with autoimmune sialadenitis (chronic inflammatory infiltrates replacing salivary gland parenchyma). Between 5 and 8 samples from the minor salivary glands, taken as a transmucosal procedure via the labial mucosa, are required for diagnosis.[19][14] Parotid gland biopsy is a rarelt used alternative.[35][36]
Diagnosis of IgG4-related sialadenitis involves combining the clinical features with elevated absolute serum IgG4 levels and an increased ratio of IgG4 to IgG plasma cells. Definitive diagnosis rests on the histopathological features of a lymphoplasmocytic infiltrate and fibrosis.[37] Ultrasound characteristics may have advantages over MRI or CT imaging.[6]
In the presence of a submandibular swelling suspicious of a neoplasm, ultrasound or CT scan and fine needle aspiration cytology are recommended. This may be sufficient to diagnose chronic sclerosing sialadenitis and thus reserve surgical removal of the gland for symptomatic cases. Scintigraphy with radiolabelled Tc-99 may be helpful in diagnosing a hypofunctional salivary gland accompanying chronic sclerosing sialadenitis, prior to consideration of surgery.[26] If subacute necrotising sialadenitis is suspected, a biopsy can confirm the diagnosis and differentiate it from necrotising sialometaplasia.[Figure caption and citation for the preceding image starts]: Occlusal radiographic film showing presence of multiple sialoliths in the left Wharton's ductFrom the personal collection of Dr A. Aguirre; used with permission [Citation ends].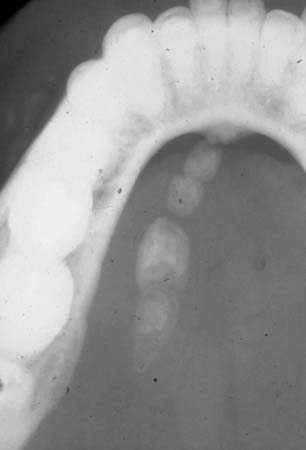
Imaging
A variety of imaging modalities are available. These include plain radiographs, ultrasound sonography, conventional X-ray sialography, digital subtraction sialography (DSA), MRI and MR sialography, sialendoscopy, and salivary gland scintigraphy.
Consensus guidelines for the investigation and management of obstructive sialadenitis recommend sonography as the method of choice.[38] However, while sonography is often readily available, most clinicians will request a plain radiograph first. Alternative or additional imaging studies may be selected based upon clinician preference, patient specific issues, or local service factors and expertise.
Conventional radiography
Although sonography is often readily available, most clinicians will request plain radiographs, such as panoramic and occlusal views, as initial screening investigations.
Smaller and non-radio-opaque stones may not be visualised.
Sonography
Gland architecture and duct systems can be evaluated, and stones with a diameter greater than 1 mm detected, using a 7.5-13 MHz linear probe in B-mode.[38]
Contrast agent enhancement or tomographic imaging improve resolution of infiltrative or malignant processes, and the deep portion of the parotid gland cannot be fully evaluated without these techniques.
A negative ultrasound cannot conclusively exclude a small stone, and MRI or CT may be required.
DSA sialography
DSA sialography has a high sensitivity for detecting obstruction and may also allow estimation of the probability of success of endoscopic stone retrieval. Salivary stones and some obstructions may resolve with the investigation, but inflammation of the duct system cannot be detected.
Acute inflammation is a relative contraindication.
Radiation-free and less invasive methods, such as MR sialography or sialendoscopy performed with interventional intent, are now preferred where available.
MR sialography
Highly T2-weighted sequences are used for MR sialography.[38] Three dimensional methods are preferred for detecting ductal stenoses and strictures. Intravenous or intraductal contrast agent may not be necessary if the pre-stenotic duct is dilated with saliva.
MR sialography may be inferior to conventional X-ray sialography for the visualisation of the smallest branches of the duct system, but provides superior visualisation of the periductal soft tissue structures and is less invasive.
The spatial resolution of MR sialography is inferior to sialendoscopy for differentiation between stones, mucus plugs, and intraductal lesions, but again is less invasive.
Sialendoscopy
A minimally invasive technique to aid visualisation and treatment of sialoliths, anatomical malformations, polyps, foreign bodies, and ductal strictures. Sialendoscopy is an established technique though tends to be available in tertiary centres
It is avoided in acute inflammation because of an increased risk of infection and duct perforation.
Scintigraphy
Scintigraphy with Tc-99m pertechnetate may be indicated when removal of a dysfunctional gland is being considered. It can be used to assess function after the treatment of obstructive sialadenitis or following radiotherapy.[38]
Scintigraphy is of value in determining the degree of salivary gland hypofunction in Sjogren syndrome.
MRI
MRI, and sometimes CT imaging, is required if neoplasia is suspected.[38]
MRI is the most reliable method for delineating soft tissue changes.
Use of this content is subject to our disclaimer