Investigations
1st investigations to order
FBC
renal function
liver function tests
Test
May identify cholestasis secondary to hepatic metastasis or regional hepatic inflammation.[64]
Baseline values prior to start of potentially hepatotoxic chemotherapy are useful.
Result
normal or elevated aspartate aminotransferase, alanine aminotransferase, and serum bilirubin
urinalysis
Test
Visible or non-visible haematuria may be a presenting sign.[4]
Proteinuria may be found in children with Denys-Drash syndrome or with associated nephrosis.
Result
clear/red colour; red blood cell >3/high power field; protein >30 mg/dL or normal
serum total protein/albumin
Test
Cachexia and poor oral intake may lead to lower serum albumin/total protein.
Rarely, proteinuria may result in hypoalbuminaemia in patients with bilateral Wilms' tumour, Denys-Drash syndrome, or other condition associated with nephrosis.[65]
Result
normal or low
coagulation studies
serum calcium level
Test
May be elevated due to bone metastasis and elevated PTH from a more aggressive renal tumour.[67]
Result
normal or elevated
abdominal ultrasound
Test
First-line test for establishing presumptive diagnosis of a renal tumour.[4][49]
Relatively easy to perform without sedation in young children, abdominal ultrasound establishes the renal origin, and the number and location of renal masses.[49]
Duplex ultrasound can be used to determine the presence of a tumour thrombus in the renal vein and inferior vena cava.[49]
Ultrasound to assess venous involvement and additional urogenital tract imaging to assess for ureteric involvement is controversial and not routinely needed.
Result
evenly echogenic, heterogenous, mainly solid mass arising from kidney(s) with or without cystic areas
CT or MRI abdomen and pelvis
Test
Either CT or MRI of the abdomen and pelvis should be obtained for locoregional staging by evaluating the contralateral kidney for synchronous disease and determining the size and number of ipsilateral masses, presence of lymphadenopathy, presence and extent of tumour thrombus, and presence of metastatic disease to organs such as the liver.[49][Figure caption and citation for the preceding image starts]: Wilms' tumour: MRI findingsUHRAD.com; used with permission [Citation ends].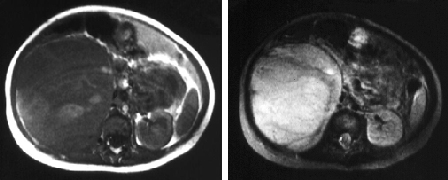
Signs of possible rupture and infiltration into adjacent organs may be observed; however, imaging has a poor predictive value for preoperative rupture.[50]
Children's Oncology Group (COG) protocols support the use of CT or MRI for locoregional staging; the International Society of Paediatric Oncology - Renal Tumour Study Group (SIOP-RTSG) prefers MRI over CT for abdominopelvic evaluation.[49]
MRI is strongly recommended over CT in case of bilateral or genetically predisposed Wilms' tumours, as it may help identify multifocal tumours and nephrogenic rests.[49][68][69][50]
Review of histology is required for a definitive diagnosis.
Result
renal mass with heterogeneous enhancement; extrarenal lesions associated with metastatic disease
CT chest (with or without contrast)
Test
Lungs are the most frequently occurring site of metastases for Wilms' tumour; however, differentiation of malignant and benign pulmonary nodules remains challenging.[49]
The International Society of Paediatric Oncology (SIOP) protocol, and the Children's Oncology Group (COG) protocol, advocate chest CT for detection of lung lesions at diagnosis.[49]
The SIOP protocol classifies pulmonary nodules ≥3 mm as lung metastases, but there is significant observer variability such that use of this threshold is questioned.[70][71]
Result
pulmonary lesions associated with metastatic disease; intracardiac extension; thoracic lymphadenopathy; pulmonary embolism
chest x-ray
Test
In resource-limited regions, chest x-ray can be used to identify lung metastasis; however, plain radiography may miss smaller pulmonary lesions (typically <1 cm).[4]
Chest x-ray may be used for disease surveillance at follow-up.[49][72]
Result
pulmonary lesions; hilar and/or mediastinal widening due to lymphadenopathy may be identified
Investigations to consider
tumour histology
Test
Definitive diagnosis is based on histology of tumour following surgical resection (nephrectomy).[4][48]
If the tumour is unresectable, the Children's Oncology Group (COG) protocol recommends an open biopsy or core needle biopsy with a minimum of 10-12 non-necrotic cores to ensure sufficient tissue for molecular testing.[4][52]
The International Society of Paediatric Oncology (SIOP) protocol does not routinely recommend pretreatment biopsy.[53]
Percutaneous cutting needle biopsy (tru-cut biopsy) can potentially be considered in patients whose tumours are suspected not to be Wilms' tumour, such as young children with stage IV disease and in children >10 years of age (as the frequency of non-Wilms renal tumours is increased in these patient populations).[53][54]
All three lineages of the developing kidney (blastema, epithelia, and stroma) can be identified in classic triphasic Wilms' tumour histology.[18]
Two classification systems used, based on histology:[73]
COG: presence or absence of anaplasia.
SIOP: low-risk (completely necrotic, cystic, partially differentiated), intermediate-risk (histology that is not low-risk or high-risk), high-risk (blastemal, diffuse anaplastic).
Result
confirms the diagnosis with characteristic pathological appearances
genetic testing
Test
Genetic testing for changes in WT1 and other genes associated with Wilms' tumour may be considered for all patients with Wilms' tumour. In particular, genetic testing is recommended for patients at high risk for an underlying predisposition syndrome. Features suggestive of a predisposition syndrome include bilateral or multifocal disease, early onset (age <2 years), family history of Wilms' tumour, multiple nephrogenic rests, unexplained proteinuria or renal failure, or urogenital or other phenotypic anomalies associated with predisposing syndromes.[48][55]
Gene panels are available for Wilms' tumour predisposition that include WT1 and other relevant genes such as TRIM28 and REST.[38][48][56][57]
Patients with clinical features suggestive of Beckwith-Wiedemann syndrome may be tested for genetic and/or epigenetic changes at the 11p15.5 imprinted region, which may also be mosaic.[37][38][57]
Testing strategies may combine a Wilms' tumour gene panel with testing for Beckwith-Wiedemann syndrome, or may be targeted for patients with clinical features suggestive of a specific syndrome.[57]
Result
deletions of WT1 and other contiguous genes; confirms genetic predisposition (e.g., Beckwith-Wiedemann syndrome, familial Wilms' tumour)
tumour molecular biomarker testing
Test
Evaluated to help guide risk assessment and treatment in patients with favorable histology Wilms' tumours.[48]
Assays for biomarkers associated with unfavourable outcomes, such as loss of heterozygosity (LOH) in 16q, 11p, and 1p, and gain of chromosome 1q, are performed on tumour tissue.[33][48][58][59]
Result
LOH at 16q, 11p, and 1p; 1q gain
Use of this content is subject to our disclaimer