Investigations
1st investigations to order
flexible laryngoscopy
Test
Should be performed in all patients to assess laryngeal anatomy and related comorbidity (e.g., mucosal inflammation as evidence of GORD).
Topical anaesthesia is applied to the nasal mucosa so the upper airway and larynx may be examined while the child is fully awake. This allows assessment of vocal cord movement. However, flexible laryngoscopy does not provide for a reliable assessment of the subglottis or more distal airway.
Laryngeal features may include an elongated or tubular epiglottis with collapse into the glottic airway on inspiration (12%).[22] The aryepiglottic folds may be short (15% of cases), with posterior angling of the epiglottis.[22][11] The arytenoids may also seem tall due to redundant mucosa with anterior and medial collapse of the arytenoids, cuneiforms, corniculate cartilage, or aryepiglottic folds into the airway (57%).[22]
These features may occur separately or in combination (15%).[22]
Result
dynamic collapse of the supraglottic tissues on inspiration; visible narrowing and obstruction of the supraglottic airway; anatomical anomalies; evidence of GORD
Investigations to consider
rigid laryngobronchoscopy
Test
With flexible laryngoscopy, subglottic views cannot be reliably obtained to exclude synchronous airway pathology. Furthermore, LM can only be confirmed with dynamic views obtained during spontaneous respiration, under a general anaesthetic, usually as the general anaesthesia lightens.
Rigid laryngobronchoscopy can both confirm the findings of flexible laryngoscopy and reliably exclude co-existing airway lesions (e.g., tracheomalacia, subglottic stenosis, or vocal cord palsy). The incidence of second lesions has been reported to be between 12% and 64%.[22][8][23][24][25]
Some authors advise a full airway assessment in all patients with LM to ensure potentially life-threatening pathology is not overlooked, whereas others proceed with rigid endoscopy only if there is apnoea, failure to thrive, or clinical suspicion of a second lesion.[22][24][26] The procedure is performed in all cases requiring endoscopic surgery for treatment of LM.[Figure caption and citation for the preceding image starts]: Typical example of laryngomalaciaFrom the personal teaching collection of Simone J. Boardman, MBBS, FRACS (OHNS) and C. Martin Bailey, BSc, FRCS, FRCSEd [Citation ends].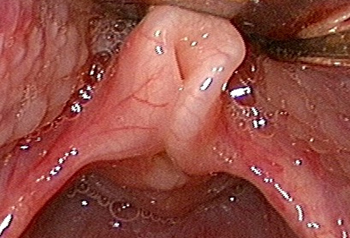
Result
collapse of the supralaryngeal tissues during inspiration is evident when the patient is breathing spontaneously; may show additional pathology
FEES testing
Test
Videofluoroscopic swallowing studies or functional endoscopic evaluation of swallowing (FEES) testing is used in assessing feeding problems to detect episodes of laryngeal penetration or aspiration.
Result
may reveal swallowing abnormalities
polysomnography
Test
May be considered to determine associated obstructive sleep apnoea (OSA). Sleep studies assist in the ongoing management of patients with LM and OSA, particularly in following the progress and making management decisions for complex patients with multiple medical problems.
Result
variable; may show increased respiratory disturbance index (RDI)
chest x-ray
Test
May provide evidence of synchronous airway pathology or aspiration.
Result
variable; may show cavities or new infiltrate in dependent lung fields
lateral neck radiograph
ECG
Test
Order in patients with clinical findings suggestive of an underlying genetic syndrome (e.g., Down's syndrome) associated with congenital heart disease.
Result
variable; may show evidence of congenital heart disease
echocardiogram
Test
Order in patients with clinical findings suggestive of an underlying genetic syndrome (e.g., Down's syndrome) associated with congenital heart disease.
Result
variable; may show evidence of congenital heart disease
Use of this content is subject to our disclaimer