Investigations
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Behandeling acuut cardiogeen longoedeem in een urgente situatie (in afwachting van hospitalisatie)Published by: Werkgroep Ontwikkeling Richtlijnen Eerste Lijn (Worel)Last published: 2022La prise en charge de l’oedème pulmonaire aigu cardiogénique en situation d'urgence (en attente d'une hospitalisation)Published by: Groupe de Travail Développement de recommmandations de première ligneLast published: 20221st investigations to order
ECG
Test
Record and interpret a 12-lead ECG for any patient with suspected heart failure; monitor this continuously.[1]
Arrange this immediately if the patient is haemodynamically unstable or in respiratory failure to look for any life-threatening cause of acute heart failure such as acute coronary syndrome. See Non-ST-elevation myocardial infarction.[1]
Check heart rhythm, heart rate, QRS morphology, and QRS duration, as well as looking for specific abnormalities such as arrhythmias, atrioventricular block (both left bundle branch block and right bundle branch block), evidence of a previous myocardial infarction (e.g., Q waves) and evidence of left ventricular hypertrophy.[1]
Practical tip
Presence of wide QRS or bundle branch block (BBB) is associated with a worse prognosis. Evidence from one meta-analysis showed that BBB of any type (right or left) was associated with a modest increase in the risk of all cause mortality in patients with acute heart failure.[33]
The ECG is usually abnormal in acute heart failure.[1]
[Figure caption and citation for the preceding image starts]: ECG showing left ventricular hypertrophy with sinus tachycardiaFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].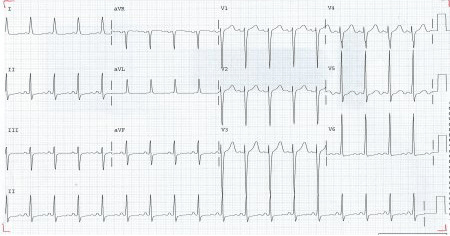
Result
arrhythmias, ischaemic ST- and T-wave changes
chest x-ray
Test
Pulmonary congestion
Pleural effusion
Interstitial or alveolar oedema
Cardiomegaly.
Practical tip
Be aware that significant left ventricular dysfunction may be present without cardiomegaly on chest x-ray.[34]
[Figure caption and citation for the preceding image starts]: Chest x-ray showing acute pulmonary oedema with increased alveolar markings, fluid in the horizontal fissure, and blunting of the costophrenic anglesFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Chest x-ray showing acute pulmonary oedema with increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray showing acute pulmonary oedema with increased alveolar markings and bilateral pleural effusionsFrom the private collections of Syed W. Yusuf, MBBS, MRCPI, and Daniel Lenihan, MD; used with permission [Citation ends].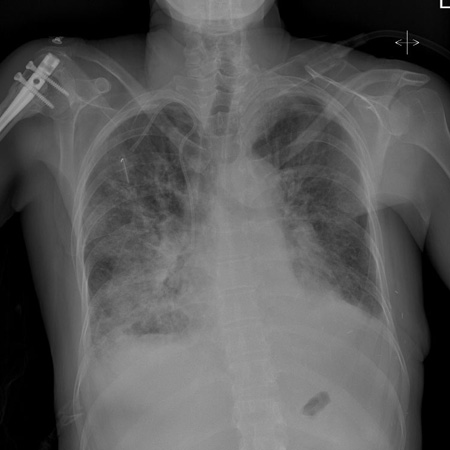
Result
pulmonary congestion, pleural effusion, pulmonary oedema, cardiomegaly
natriuretic peptides
Test
Order N-terminal pro-B-type natriuretic peptide (NT-proBNP) if available. Brain natriuretic peptide (BNP) or mid-regional pro-atrial natriuretic peptide (MR-proANP) (in some countries) are alternatives.[1][27][29]
Normal levels make the diagnosis of acute heart failure unlikely.[1][29] However, elevated levels of natriuretic peptides do not automatically confirm the diagnosis of acute heart failure as they may be associated with a wide variety of cardiac and non-cardiac causes. Low levels of natriuretic peptides can occur in end-stage heart failure, flash pulmonary oedema, or right-sided acute heart failure.[1]
Most older patients presenting to hospital with acute breathlessness have an elevated NT-proBNP so separate ‘rule in’ diagnostic cut-offs are useful in this setting.
If NT-proBNP is significantly elevated (>1800 ng/L [>1800 pg/mL] in patients >75 years; see table below) acute heart failure is likely and should be confirmed by inpatient echocardiography. If the NT-proBNP is intermediate (>300 ng/L [>300 pg/mL] but <1800 ng/L [<1800 pg/mL]), consider other possible causes of breathlessness, but if these are excluded and diagnostic suspicion of heart failure remains, request an echocardiogram.[29]
Age (years) | <50 | 50-75 | >75 |
NT-proBNP level (ng/L or pg/mL) above which acute heart failure is likely[27] | >450 | >900 | >1800 |
Female sex is also associated with modest elevation in NT-proBNP.[35]
Practical tip
Be aware that natriuretic peptides may be raised due to other causes (e.g., acute coronary syndrome, myocarditis, pulmonary embolism, older age, and renal or liver impairment), hence the need for practical ‘rule in’ cut-offs.[1]
Result
NT-proBNP >300 ng/L (>300 picograms [pg]/mL), BNP >100 ng/L (>100 pg/mL), MR-proANP >120 ng/L (>120 pg/mL)
troponin
Test
Measure troponin in all patients with suspected acute heart failure.[28]
Troponin may be useful for prognosis; elevated levels are associated with poorer outcomes.[28]
Be aware that interpretation is not straightforward; type 2 myocardial infarction and myocardial injury are common.
Result
most patients with acute heart failure have an elevated troponin level
full blood count
Test
Order a full blood count to identify anaemia, which can worsen heart failure and also suggest an alternative cause of symptoms.[1]
Result
may show anaemia
urea, electrolytes, and creatinine
Test
Order as a baseline test to inform decisions on drug treatment that may affect renal function (e.g., diuretics, ACE inhibitors), and to exclude concurrent or causative renal failure.
Result
baseline levels
glucose and HbA1c
Test
Measure blood glucose in all patients with suspected acute heart failure to screen for diabetes.[28] In practice, also request HbA1c (based on the opinion of our expert).
Result
may be elevated
liver function tests
thyroid function tests
Test
Order thyroid-stimulating hormone in any patient with newly diagnosed acute heart failure. Both hypothyroidism and hyperthyroidism can cause acute heart failure.[1] See Overview of thyroid dysfunction.
Result
may show hypothyroidism or hyperthyroidism
C-reactive protein
Test
Consider ordering C-reactive protein (based on the opinion of our expert).
Inflammation is associated with progression of chronic heart failure.
Levels of high-sensitivity C-reactive protein are raised in patients with acute heart failure.[37]
Result
raised in acute heart failure
D-dimer
Test
Indicated in patients with suspicion of acute pulmonary embolism.[28]
Result
raised in acute pulmonary embolism; see Pulmonary embolism
echocardiography
Test
Arrange immediate bedside echocardiography for any patient with suspected heart failure who is haemodynamically unstable or in respiratory failure.[27] Specialist expertise is required.
If a patient is haemodynamically stable, arrange echocardiography within 48 hours.[29][38]
Echocardiography is used to assess myocardial systolic and diastolic function of both left and right ventricles, assess valvular function, detect intracardiac shunts, and measure left ventricular ejection fraction (LVEF).[29]
Evaluating the patient’s LVEF has a key role in assessing the severity of any decrease in systolic function and is essential in determining your patient’s long-term management.[1]
Practical tip
The diagnosis of heart failure with reduced ejection fraction (HFrEF) requires an LVEF ≤40%. Patients with heart failure with preserved ejection fraction (HFpEF) have clinical signs of heart failure with normal or near-normal LVEF, and evidence of structural and/or functional cardiac abnormalities (including raised natriuretic peptides) in the absence of significant valvular disease. There is an emerging group of patients with heart failure with mildly reduced ejection fraction (41% to 49%) (HFmrEF). The benefits of standard HFrEF therapies are less certain for this population; SGLT2 inhibitors are recommended alongside diuretics for fluid retention, but guidelines do not offer strong recommendations on other HFrEF therapies).[1]
Result
left ventricular systolic dysfunction, left ventricular diastolic dysfunction, constriction, left ventricular hypertrophy, valve disease, restrictive heart disease, right ventricular dysfunction, pulmonary hypertension, may detect the underlying cause
Investigations to consider
venous or arterial blood gas
Test
Perform an arterial blood gas (ABG) if an accurate measurement of arterial partial pressure of oxygen (PaO2) and arterial partial pressure of carbon dioxide (PaCO2) is needed.[1]
Consider measurement of blood pH and PaCO2 even if the patient does not have cardiogenic shock, especially if respiratory failure is suspected.[1]
Do not routinely perform an ABG. Venous blood gas may acceptably indicate pH and PaCO2. [1]
A blood gas may show:
Hypoxaemia
Metabolic acidosis with raised lactate in a patient with hypoperfusion
Type I or type II respiratory failure.
Result
hypoxaemia: PaO2 <10.67 kPa (<80 mmHg) on arterial blood gas; metabolic acidosis with raised lactate: pH <7.35, lactate >2 mmol/L (>18 mg/dL); type I respiratory failure: PaO2 <8 kPa (<60 mmHg); type II respiratory failure: PaCO2 >6.65 kPa (>50 mmHg)
blood tests screening for myocarditis
Test
Consider blood tests screening for acute myocarditis if you suspect myocarditis as a cause of acute heart failure. These include screening for viruses that cause acute myocarditis, including coxsackievirus group B, HIV, cytomegalovirus, Ebstein-Barr virus, hepatitis, echovirus, adenovirus, enterovirus, human herpes virus 6, parvovirus B19, and influenza viruses. See Myocarditis.
Result
may show presence of virus
bedside thoracic ultrasound
Test
Bedside thoracic ultrasound is useful in countries with no access to BNP/NT-proBNP testing for detecting signs of interstitial oedema and pleural effusion in heart failure if specialist expertise is available.[1][27] It may be used as an alternative to chest x-ray in the emergency setting in conjunction with medical history and physical examination.[39][40]
Result
interstitial oedema, pleural effusion
Cardiac magnetic resonance (CMR)
Test
Consider cardiac magnetic resonance (CMR) imaging when non-invasive tests and echocardiographic images are suboptimal or when an unusual cause of heart failure is suspected, and for diagnosis of specific cardiomyopathies.[1][2]
Result
late gadolinium enhancement in affected myocardium (cardiomyopathy)
Nuclear medicine imaging
Test
Single-photon emission CT (SPECT) or positron emission tomography (PET) may be useful in assessing ischaemia and myocardial viability. 3,3-diphosphono-1,2-propanodicarboxylic acid (DPD) scintigraphy may be useful for the detection of transthyretin cardiac amyloidosis.[1][2]
Result
ischaemia, mixed ischaemia/scar or scar tissue; in patients with transthyretin cardiac amyloidosis, a DPD scintigraphy may show myocardial tracer uptake
Use of this content is subject to our disclaimer