Differentials
Common
Stroke
History
transient/permanent symptoms: usually abrupt onset, numbness, paraesthesia, weakness, paralysis, headache, facial drop, speech disturbance, swallowing difficulties, vision loss, memory loss, and/or loss of consciousness; mass effect/herniation: usually progressive impairment of consciousness, one-sided weakness, visual disturbance, hearing disturbance, taste disturbance, difficulty swallowing, facial paralysis, and/or difficulty in breathing
Exam
commonly: hypertension, contralateral hemiparesis, hemisensory loss, dysphasia, dysphagia, anosognosia, visuospatial deficit, contralateral vision loss, memory loss, Weber's syndrome (ipsilateral ocular nerve palsy and contralateral hemiplegia), constricted pupils, and/or ipsilateral ataxia followed by ipsilateral gaze paresis and ipsilateral facial paralysis; mass effect/herniation: usually progressive impairment of consciousness, hemiparesis, oculomotor palsy, cranial nerve palsies, respiratory arrest, hypertension, hypotension, and/or brain death
1st investigation
- CT head:
haemorrhagic: intra- or extracerebral mass effect with displacement of midline structures (septum pellucidum or pineal by >9 mm from the midline); ischaemic: hypoattenuation (darkness) of the brain parenchyma, loss of grey matter-white matter differentiation, sulcal effacement
More - ECG:
normal, myocardial infarction (MI)-related changes, or atrial fibrillation (AF)
More
Other investigations
Cardiac arrest
History
sudden collapse, may be preceded by chest pain
Exam
absent carotid pulse
1st investigation
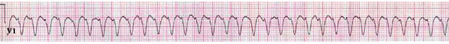
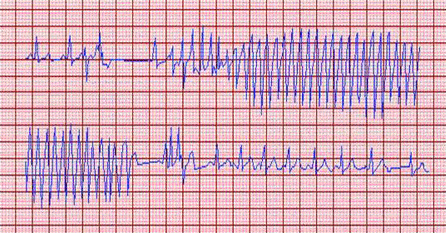
- ECG:
cardiac rhythm disturbance: for example, ventricular fibrillation or asystole
More
Other investigations
- ABG:
may show respiratory acidosis; metabolic acidosis; respiratory acidosis with renal compensation; metabolic acidosis with respiratory compensation; mixed metabolic and respiratory acidosis
- somatosensory evoked responses with median nerve stimulation at the wrist:
variable
More - neuron-specific enolase:
variable
More
Hypertensive encephalopathy
History
visual disturbance, impaired consciousness, weakness; posterior reversible encephalopathy syndrome: vision loss, convulsive seizures
Exam
hypertension, variable focal features, such as hemiplegia; posterior reversible encephalopathy syndrome: cortical blindness (pupillary light reflex is spared but patient is blind)
1st investigation
- cranial CT:
normal or vasogenic oedema, usually most marked in the white matter of the posterior parts of the cerebral hemispheres
More
Basilar artery thrombosis
History
commonly vision loss and photopsia
Exam
often quadriparesis, pseudobulbar palsy, papillary and ocular palsies
1st investigation
- cranial CT with CT angiogram:
basilar artery occlusion
More
Other investigations
- MRI brain:
basilar artery occlusion; brainstem ischaemia; thalamus ischaemia, ischaemia of peripheral posterior cerebral artery territories
More
Cerebral venous thrombosis
History
intractable worsening headache of subacute onset, often associated with nausea and vomiting, seizures common
Exam
papilloedema; venous infarction: focal neurology, such as hemiplegia
1st investigation
- MRI brain with venous phase:
occluded cortical veins or larger venous channels, often parenchymal haemorrhages
More - CT angiogram with venous follow through:
occluded cortical veins or deep or superficial venous channels
Other investigations
- thrombophilia screen:
normal, protein C deficiency, protein S deficiency, factor V Leiden, antithrombin 3 deficiency, polycythaemia, thrombocytosis, paroxysmal nocturnal haemoglobinuria
More
Alcohol-use disorder
History
history of harmful use of alcohol and alcohol dependence; tolerance; withdrawal; impaired control of drinking behaviour; continued alcohol use despite adverse consequences
Exam
odour of alcoholic beverage on breath, stigmata of liver disease in chronic alcoholics
1st investigation
- serum ethanol:
>17.4 mmol/L (>80 mg/dL)
Other investigations
Substance abuse and overdose
History
ingestion of lysergic acid diethylamide (LSD), cocaine, amfetamines, opioids, sedatives, organophosphates, carbamate insecticides, jimson weed, deadly nightshade, methanol, ethylene glycol (antifreeze), ephedrine, pseudoephedrine, alpha-2 agonists, sedatives, first-generation antihistamines, tricyclic antidepressants, benzatropine
Exam
variable
1st investigation
- drug screen:
positive for toxin
More
Other investigations
- ABG:
normal, respiratory alkalosis, or metabolic acidosis
More
Carbon monoxide poisoning
History
typically presents in winter months with headache, confusion, and abdominal discomfort; patients may visit emergency department repeatedly with these symptoms only to arrive later in coma; also presents as patients discovered comatose following exposure to internal combustion engine exhaust (vehicle or generator)
Exam
typically impaired consciousness with intact brainstem reflexes; cherry red discoloration of mucous membranes and lips is helpful but rarely present (should not be relied on)
1st investigation
- blood carboxyhaemoglobin concentration:
>15%
More
Other investigations
- MRI brain:
acute changes in white matter
- single-photon emission CT:
abnormally reduced metabolic activity
More
Sepsis-associated encephalopathy
History
fever may be present; may be a history of confusion, delirium, and (commonly) any of: cough, shortness of breath, chest pain, dysuria, urinary urgency, urinary frequency, reduced urine output, loin pain, joint pain; may be a history of risk factors such as recent surgery, presence of immunosuppression
Exam
elevated/depressed body temperature, increased heart rate, tachypnoea; may be signs of local infection (e.g., abnormal chest examination), impaired attention, disorientation, delusions, hallucinations (delirium or stupor with paratonic rigidity or asterixis may precede coma); neurological examination is otherwise normal, although patients treated in the intensive care unit (ICU) may develop a neuromyopathy (ICU-acquired weakness)
1st investigation
- basic test panel (FBC, serum electrolytes, blood glucose, serum liver function tests, coagulation profile):
elevated WBC count or leukopenia; elevated urea and creatinine; low platelets; blood glucose may be elevated or, more rarely, low; serum transaminases and serum bilirubin may be elevated; may be prolonged or elevated INR, PT, aPTT
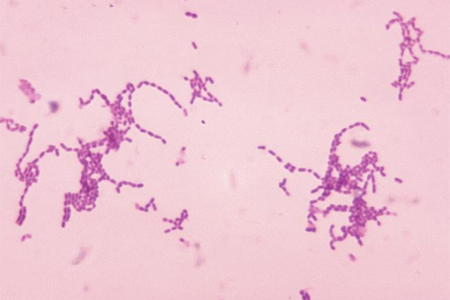
More - cultures and Gram stain of blood, urine, sputum, and body fluid:
responsible organisms may be identified and recovered
- arterial blood gas:
may be hypoxia, hypercapnia, elevated anion gap, metabolic acidosis
- serum lactate:
may be elevated >2 mmol/L (>18 mg/dL)
More - ECG:
normal; may demonstrate tachycardia
Other investigations
- EEG:
graded pattern of severity ranging from mild slowing to a burst-suppression pattern
More
Bacterial meningitis
History
presence of any 2 of: fever, headache, neck stiffness, or any alteration in mental status before coma can suggest diagnosis; children also often have vomiting, photophobia, and lethargy
Exam
fever, unwell appearance; meningococcal meningitis: petechial rash plus or minus shock, neck stiffness to forwards flexion, inability to completely extend the lower limbs (Kernig's sign), flexion at the hip and knee when the neck is flexed (Brudzinski's sign)
1st investigation
- FBC:
elevated WBC count with left shift
- blood culture:
positive for Neisseria meningitidis, Streptococcus pneumoniae, or Haemophilus influenzae in
More - CT or MRI brain:
normal or early hydrocephalus and meningeal enhancement
More - cerebrospinal fluid (CSF) analysis:
elevated CSF pressure (usually >180 mm H₂O or >20 mmHg), pleocytosis (usually >1000 WBCs), mostly polymorphonuclear leukocytes, elevated protein (>45 mg/dL, reduced glucose (usually <40 mg/L or 3 mmol/L and <40% of serum glucose); CSF Gram stain positive in most untreated cases
More
Other investigations
Syncope
History
transient coma; prodromal diaphoresis, nausea, dimming of vision, tinnitus; may be precipitated by upright posture, fainting avoided by sitting or lying down; coma may be abrupt without postural influence; convulsions/incontinence may occur; usually abruptly regain consciousness/orientation
Exam
postural hypotension: drop in blood pressure from supine to standing; arrhythmia/pulmonary embolism/cardiac cause: abnormal pulse rate/rhythm, murmurs; neurological cause: sensory, motor, speech, vision deficits; carotid hypersensitivity: carotid sinus massage may reproduce symptoms
1st investigation
- FBC:
anaemic cause: reduced Hb; infective cause: elevated WBC count
- serum glucose:
metabolic cause: elevated or reduced
- ECG:
abnormal results may demonstrate cardiac cause
More
Other investigations
- exercise stress test:
abnormal results may demonstrate cardiac cause
- tilt table test:
abnormal results may demonstrate cardiac cause or reflex fainting (vasomotor or vasodepressor syncope)
More - EEG:
abnormal results may demonstrate neurological cause
- CT head:
abnormal results may demonstrate neurological cause
- MRI brain:
abnormal results may demonstrate neurological cause
Seizure disorder
History
transient coma; prodromal symptoms including diaphoresis, nausea, dimming of vision, and tinnitus; convulsive movements and incontinence can occur; usually followed by confusion and drowsiness that often lasts ≥10 minutes
Exam
convulsive: bilateral synchronous convulsions, open eyes; non-convulsive: no convulsions, infrequently nystagmoid eye movements, or bilateral facial twitching
1st investigation
- EEG:
generalised seizure activity
More - serum glucose:
normal, extreme hypoglycaemia, or extreme hyperglycaemia
More - electrolyte panel:
normal, hyponatraemia, hypernatraemia, magnesium abnormality, calcium abnormality, or phosphate abnormality
- urea:
normal or uraemia
More - serum creatine kinase:
normal or markedly elevated
More - serum antiepileptic drug levels:
normal or low
More - drug screen:
normal, or positive for amfetamines/cocaine
Other investigations
- MRI brain:
neoplastic, traumatic, vascular, inflammatory, or degenerative lesions may be present
Traumatic brain injury
History
concussion: transient coma following blow to head, retrograde amnesia; ‘talk and die’ syndrome: concussion followed by lucid interval then coma; diffuse axonal injury (DAI): instant coma, eye opening usually after 2 to 3 weeks, awareness recovery variable; mass effect/herniation: usually progressive impairment of consciousness, one-sided weakness, visual disturbance, hearing disturbance, taste disturbance, difficulty in swallowing, facial paralysis, and/or difficulty in breathing
Exam
concussion: transient apnoea, loss of pupillary reflexes, loss of corneal reflexes; mass effect/herniation from epidural/subdural haematoma: usually progressive impairment of consciousness, hemiparesis, oculomotor palsy, cranial nerve palsies, respiratory arrest, hypertension, hypotension, and/or brain death
1st investigation
- CT head:
mass lesion: intra- or extracerebral mass effect with displacement of midline structures (septum pellucidum or pineal by >9 mm from the midline), petechial haemorrhages in cerebral white matter; DAI: petechial haemorrhages in corpus callosum and dorsolateral brainstem
More
Other investigations
- skull x-ray:
may show linear or depressed skull fracture
More - MRI brain:
DAI: petechial haemorrhages; severe DAI: corpus callosum haemorrhage, dorsolateral rostral brainstem haemorrhage; mass lesion: extra-axial epidural or subdural haematomas, or intra-axial contusion with variable confluence (typically on orbital surfaces of frontal lobes, and in temporal lobe)
More - tensor tract imaging:
DAI: tract damage
More - somatosensory evoked response testing:
DAI: bilateral absence or delay of the N20 response from median nerve stimulation
More
Hypoglycaemia
History
cold perspiration, confusion, multi-focal or generalised seizures, light-headedness, or agitation preceding loss of consciousness
Exam
increased heart rate, elevated blood pressure, diaphoresis
1st investigation
- serum glucose:
reduced <2.8 mmol/L (<50 mg/dL)
Other investigations
- CT head:
normal
- MRI brain:
severe cases: increased diffusion weighted signal of cerebral cortex with thalamus and cerebellum sparing
More
Hyperglycaemia
History
increased diuresis, progressive confusion, history of diabetes mellitus, sub-optimal insulin therapy, seizures
Exam
clinical dehydration, tachycardia, hypotension; diabetic ketoacidosis (DKA): Kussmaul's breathing, acetone breath
1st investigation
- serum glucose:
elevated
More - urinary ketones:
normal or elevated if DKA
- serum ketones:
normal or elevated if DKA
Other investigations
- ABG:
normal or metabolic acidosis if DKA
- CT head:
normal
- MRI brain:
normal
Hepatic encephalopathy
History
underlying hepatic failure, alcoholism, intravenous drug abuse, paracetamol overdose; malaise, confusion/delirium, agitation, progressive impairment of consciousness from stupor to coma; chronic liver disease: decompensation often due to intercurrent infection, sedative drugs, excessive diuresis or constipation
Exam
ascites, spider nevi, dilated peri-umbilical veins, ± jaundice, tremor, increased tone, asterixis, Kayser-Fleischer rings (crescentic, rusty-brown discoloration in the limbus of the corneae, especially in young patients)
1st investigation
- liver function tests (LFTs):
abnormal
More - INR:
normal or elevated
More - serum glucose:
normal or reduced
More - serum lactate:
normal or elevated
More - FBC:
elevated WBC count if intercurrent infection
- serum electrolyte panel:
hyponatraemia
- urea:
elevated in cases with hepatorenal syndrome
- serum creatinine:
elevated in cases with hepatorenal syndrome
- ABG:
respiratory alkalosis
Other investigations
Hyponatraemia
History
headache, behavioural changes, nausea, vomiting, impaired consciousness
Exam
generalised or focal neurological impairment; occasionally mono- or hemiparesis, ataxia
1st investigation
- serum electrolyte panel:
sodium reduced <145 mmol (145 mEq/L)
More
Other investigations
- CT head:
normal or slight reduction in brain volume
- MRI brain:
normal
Hypothyroidism
History
gradual slowing down to impairment of consciousness; weight gain, constipation, lethargy; precipitation by intercurrent infection, cold exposure, stress, phenytoin, amiodarone, lithium, or withdrawal of thyroid replacement therapy; myxoedema coma: puffy eyes, previous thyroid disorder, head injury, or pituitary injury
Exam
myxoedema coma: pale doughy skin, periorbital swelling, swollen tongue, hypothermia, bradycardia, slow relaxation phase of deep tendon reflexes, hypoventilation
1st investigation
- thyroid function test (TFT):
reduced thyroxine, elevated or reduced thyroid-stimulating hormone (TSH)
More
Wernicke's encephalopathy
History
coma, hypothermia; history of alcohol misuse, malnutrition, gastric stapling, or patients requiring haemodialysis (not taking supplemental B vitamins)
Exam
absent vestibulo-ocular reflexes in hypothermic patient with preserved pupillary reflexes is a major clue; triad of ataxia, ophthalmoplegia, and encephalopathy is not always present
1st investigation
- plasma pyruvate:
elevated
More
Hypophosphataemia
History
previous malnutrition with recent in-hospital feeding; deterioration with stupor, coma, myoclonus, seizures, or profound weakness after being given nutritional supplementation or glucose solutions in hospital
Exam
severe muscle weakness, features of metabolic encephalopathy, including multi-focal myoclonus or seizures
1st investigation
- serum phosphate:
reduced <0.5 mmol/L (1.5 mg/dL)
More - serum electrolyte panel:
normal or reduced magnesium, normal or reduced potassium
Other investigations
- CT head:
normal
Uncommon
Subarachnoid haemorrhage
History
initial severe headache, described as 'worst ever'; photophobia, neck stiffness, abrupt loss of consciousness in 30%; mass effect/herniation: usually progressive impairment of consciousness, one-sided weakness, visual disturbance, hearing disturbance, taste disturbance, difficulty in swallowing, facial paralysis, and/or difficulty in breathing
Exam
neck stiffness to forward flexion (if not comatose); retinal or pre-retinal (subhyaloid) haemorrhage on funduscopy; early third nerve palsy may be present; mass effect/herniation: usually progressive impairment of consciousness, hemiparesis, oculomotor palsy, cranial nerve palsies, respiratory arrest, hypertension, hypotension, and/or brain death
1st investigation
- CT head:
blood in basal cisterns and subarachnoid space over the hemispheres (95% cases); intra-ventricular blood and early hydrocephalus (some cases)
More
Encephalitis
History
initial fever and malaise followed by speech difficulty, seizures, behavioural changes, impaired alertness; history of overseas travel; history of recent infection with infectious mononucleosis, measles or rubella; may also experience convulsions
Exam
cognitive testing demonstrates language disturbance (aphasia, paraphasic errors in speech, anomia, apraxia) and evidence of temporal lobe seizures (staring, unresponsiveness, automatisms); West Nile encephalitis: may have bulbar paralysis and quadriplegia
1st investigation
- MRI brain:
hyperintensities in the medial temporal lobe and insular cortex on 1 or both sides
More
Other investigations
Brain abscess
History
progressively worsening headache, seizures; mass effect/herniation: usually progressive impairment of consciousness, one-sided weakness, visual disturbance, hearing disturbance, taste disturbance, difficulty in swallowing, facial paralysis, and/or difficulty in breathing
Exam
body temperature may not be elevated; progression of focal signs; mass effect/herniation: usually progressive impairment of consciousness, hemiparesis, oculomotor palsy, cranial nerve palsies, respiratory arrest, hypertension, hypotension, and/or brain death
1st investigation
- CT head:
intra- or extracerebral mass effect with displacement of midline structures (septum pellucidum or pineal by >9 mm from the midline); rim of enhancement around the abscess is typically thin and uniform, as opposed to malignant glial tumours, which typically have walls of variable thickness
More - blood culture:
normal or positive with bacterial or fungal sepsis
More
Brain tumour
History
often progressive headache; eloquent area tumour: weakness, reduced sensation, speech problems; frontal lobe tumour: seizures; mass effect/herniation: usually progressive impairment of consciousness, one-sided weakness, visual disturbance, hearing disturbance, taste disturbance, difficulty in swallowing, facial paralysis, and/or difficulty in breathing
Exam
eloquent area tumour: lateralised weakness, sensory changes, dysphasia; mass effect/herniation: usually progressive impairment of consciousness, hemiparesis, oculomotor palsy, cranial nerve palsies, respiratory arrest, hypertension, hypotension, and/or brain death
1st investigation
- CT head:
intra- or extracerebral mass effect with displacement of midline structures (septum pellucidum or pineal by >9 mm from the midline)
More
Other investigations
- MRI brain:
intra- or extracerebral mass effect with displacement of midline structures (septum pellucidum or pineal by >9 mm from the midline)
More
Hypernatraemia
History
thirst, confusion, fever, convulsions, diarrhoea, vomiting, burns
Exam
clinical dehydration, oliguria
1st investigation
Other investigations
- CT head:
normal
- MRI brain:
normal
Hypercalcaemia
History
mental slowing and impairment, personality changes, confusion; history of abdominal pain, or kidney stones
Exam
encephalopathic features with intact brainstem functioning
1st investigation
- serum electrolyte panel:
calcium elevated, usually >3 mmol/L (12 mg/dL)
More
Hypocalcaemia
History
behavioural changes, abdominal pain, fatigue, muscle weakness, cramps, fractures, seizures
Exam
papilloedema, raised intracranial pressure; occasionally, hyperreflexia, positive Chvostek's and Trousseau's signs, tetany, laryngeal stridor
1st investigation
- serum electrolyte panel:
reduced calcium
More
Other investigations
- CT head:
normal
Hypermagnesaemia
Hypomagnesaemia
History
seizures
Exam
dysphagia, athetosis, papilloedema, raised intracranial pressure; occasionally hemiplegia
1st investigation
- serum electrolyte panel:
reduced Mg <1.0 mmol/L (<2.0 mEq/L)
Other investigations
- CT head:
normal
Porphyria
History
acute confusion, hallucinations, psychotic behaviour, anxiety, depression; abdominal, limb, chest, back pain; weakness; stupor, coma; seizures
Exam
peripheral neuropathy; sweating, tachycardia, hypertension, evidence of impairment
1st investigation
- urinary porphobilinogen (PBG):
elevated, reddish colour
More - urinary delta-aminolevulinic acid:
elevated
Other investigations
Mitochondrial disorder
History
intermittent stroke-like events, seizures, visual disturbances
Exam
short stature, hearing impairment, visual field defects or cortical blindness, ophthalmoplegia, ataxia, cardiomyopathy, polyneuropathy in varied combinations
1st investigation
- serum lactic acid:
elevated during attacks
- muscle biopsy:
ragged red fibres, stains of succinate dehydrogenase show prominent staining of endothelium
Thyroid storm
History
history of hyperthyroidism, fever, profuse sweating, weight loss, fatigue, nausea and vomiting, diarrhoea, abdominal pain, anxiety, altered behaviour, seizures; history of triggering factors, including sepsis, surgery, anaesthesia induction, radioactive iodine therapy, use of known causative medications (anticholinergics, adrenergics, non-steroidal anti-inflammatory drugs [NSAIDs], chemotherapy, excessive thyroxine), withdrawal of or non-compliance with antithyroid medication, trauma to or vigorous palpation of the thyroid, pregnancy, labour, diabetic ketoacidosis
Exam
fever >38.5°C initially followed by hyperpyrexia, tachycardia disproportionate to fever, goitre, Graves' ophthalmopathy, hyperreflexia with transient pyramidal signs, signs of high-output heart failure
1st investigation
- diagnostic criteria score:
≥45: highly suggestive; 25-44: likely; <25: unlikely
More - ECG:
may show supraventricular or ventricular tachycardia
Burns
History
pain; may be evidence of abuse or neglect in children
Exam
airway oedema; clouded cornea; erythema, cellulitis
1st investigation
- none:
diagnosis is usually apparent on clinical evaluation
Other investigations
- EEG:
mild: slowing pattern; severe: burst-suppression pattern
More
Hyperthermia
History
history of heat stroke, hot environment, stroke, trauma, encephalitis, sepsis, cocaine or amfetamine abuse; seizures
Exam
core body temperature >38.5°C; >42°C causes coma
1st investigation
- FBC:
elevated WBC count if sepsis
- blood culture:
normal or positive
Other investigations
- EEG:
slowing pattern
More
Hypothermia
History
coma preceded by delirium and then stupor as temperature drops; may be accidental; may be a history of hypothalamic disorder, spinal cord injury, hypothyroidism, adrenal failure, Wernicke's encephalopathy, advanced sepsis, sedative drug intoxication
Exam
core body temperature <35°C; <28°C usually causes coma; pupillary light reflex absent, resembling brain death
1st investigation
Other investigations
- EEG:
wave patterns vary with core temperature: <30°C: evolutionary changes with slowing pattern; 20°C to 22°C: changes to burst-suppression pattern; <20°C: isoelectric pattern
More
Psychogenic unresponsiveness
History
usually female, odd behaviour, weeping, verbalising, psychosocial problems, abuse, non-epileptic pseudoseizures, psychogenic seizures; uncommon in childhood or age >60 years
Exam
nystagmus with caloric testing implies patient conscious; variety of behaviour (e.g., eyes facing floor, rolling over to avoid being tickled, eyes closed during seizure, holding/shaking bed sides, asynchronous movements during seizure), or motionless
1st investigation
- EEG:
normal awake pattern with alpha rhythm blocking and passive eye opening
More
Other investigations
- ABG:
pseudoseizures: normal or respiratory alkalosis from hyperventilation
More
Locked-in state
History
basis pontis lesions: sudden/stuttering onset, communication with eye movement; central pontine myelinolysis: systemically unwell inpatients, history of sudden sodium/osmolality elevation; polyneuropathy: gradual onset, cranial nerve palsy; pharmacological paralysis: ICU/post-surgical recovery room onset
Exam
consciousness preserved but impaired motor output; basis pontis lesions: upper motor neuron palsy of lower cranial nerves and 4 limbs, vertical eye movement, eyes open and close voluntarily; polyneuropathy: no vertical eye movement, may lose pupillary reflexes, absent deep tendon reflexes; pharmacological paralysis: intact pupillary reflexes
1st investigation
- MRI brain:
basis pontis lesion: infarct, haemorrhage, or demyelinative lesion in basis pontis
- EMG:
acute inflammatory demyelinative polyneuropathy (AIDP) or Guillain-Barre syndrome: prolonged 'f waves'/conduction block
More
Other investigations
- CSF exam:
elevated protein with no or few white blood cells; AIDP: classic albumino-cytological dissociation
Use of this content is subject to our disclaimer