History and exam
Key diagnostic factors
common
presence of risk factors
Key factors include inflammatory diseases, human leukocyte antigen (HLA)-B27 positivity, and ocular trauma.
pain (anterior uveitis)
Sometimes described as a dull pain in the orbital region; commonly found in anterior uveitis.
Intermediate and posterior uveitis present without pain.
decreased vision
May be expressed as blurred vision, decreased acuity, or decrease in visual fields (intermediate or posterior uveitis).
synechiae
Iris adherence to either the cornea (anterior synechia) or lens (posterior synechia) typically form during acute inflammation and can also be seen on slit-lamp examination.
Both anterior synechia and posterior synechia are seen most commonly in chronic anterior uveitis.[Figure caption and citation for the preceding image starts]: Anterior uveitis with posterior synechiaeCourtesy of Mr Hugh Harris; used with permission [Citation ends].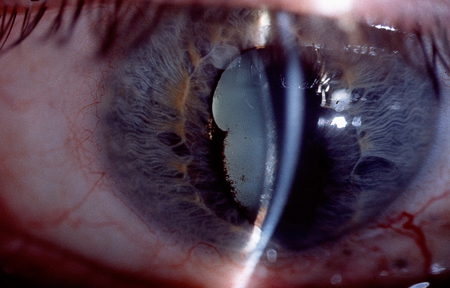 [Figure caption and citation for the preceding image starts]: Posterior synechiae (iris adhesions to anterior lens capsule) in this patient as a result of uveitisBMJ Case Reports 2012; doi:10.1136/bcr.12.2011.5418. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Posterior synechiae (iris adhesions to anterior lens capsule) in this patient as a result of uveitisBMJ Case Reports 2012; doi:10.1136/bcr.12.2011.5418. Used with permission [Citation ends].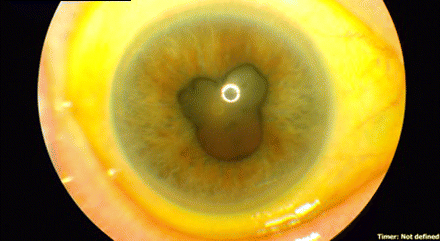
flare
Flare is the hallmark of anterior uveitis and is identified with inflammation and leukocytes floating in the aqueous humour of the anterior chamber. Sedimentation may form a hypopyon (or fluid level) of leukocytes in the anterior chamber of the eye.
The grading schema ranges from 0 to 4+.[2]
keratic precipitates
These are lymphocyte aggregates on the corneal endothelium, of a granulomatous or non-granulomatous variety, seen in anterior uveitis.[47]
Mutton-fat keratic precipitates are characteristic of granulomatous inflammatory diseases and may also be seen in the anterior chamber using a slit-lamp examination. In non-granulomatous disease, fine keratic precipitates form over the corneal endothelium. In granulomatous uveitis, Koeppe nodules (clusters of cells on the iris sphincter margin) form. Busacca nodules are clusters of cells generally seen in the anterior chamber in severe cases (rare).
Other diagnostic factors
common
tearing
Watery eyes without purulent discharge.
photophobia
Sensitivity to light is common in anterior uveitis.
floaters
Seen in posterior uveitis as a result of vitritis.
eye redness without discharge
Seen in anterior uveitis.
constricted or non-reactive pupil
Seen in anterior uveitis.
decreased intra-ocular pressure
Found in anterior uveitis. In rare cases, there may be increased pressure.
retinal exudates and oedema, optic nerve oedema
A dilated fundus examination is required to identify these signs of vitritis, found in intermediate and posterior uveitis.
retinal vascular sheathing
Retinal vascular sheathing or accumulation of inflammatory cells along vessel walls is seen in intermediate and posterior uveitis as a result of retinitis.[48] Fundoscopic examination allows visualisation. In sarcoidosis, these lesions appear as candle wax drippings. Fluorescein angiography demonstrates associated vascular leakage (perivascular staining) and capillary non-perfusion.
macular oedema
In intermediate or posterior uveitis with macular oedema, patients may present with metamorphopsia (change in object shape) or changes in colour vision.
optic disc swelling
May be seen on dilated fundoscopic examination in intermediate and posterior uveitis.
retinal haemorrhages
Damage to the retina and retinal vasculature may lead to leaky vessels, causing haemorrhage into the retina and vitreous. This is seen in intermediate and posterior uveitis.
ciliary flush
Ciliary flush is a conjunctival injection, exacerbating near the limbus. Common in anterior uveitis.
corneal oedema
May be seen in anterior uveitis.
uncommon
cataract
In cases of chronic inflammation, a posterior subcapsular cataract may be visualised.
Risk factors
strong
inflammatory diseases of the joints, bowel, or skin
human leukocyte antigen (HLA)-B27 positive
Approximately 50% of patients with anterior uveitis test positive for HLA-B27.[11]
ocular trauma
A history of ocular trauma and high-risk occupational work (e.g., metalworking) should be noted.
Use of this content is subject to our disclaimer