History and exam
Key diagnostic factors
common
postural instability with unexplained (often backwards) falls
Postural instability, resulting in progressive falls, is a cardinal feature that presents within the first 1-3 years of onset of the classic and most common subtype of PSP, PSP-Richardson’s syndrome (PSP-RS).[3][28]
Patients often report a sense of imbalance and repeated falls.[3][28] Patients with PSP-RS usually have an erect posture and tend to fall backwards.[55] Imbalanced, slow, lurching walking on a wide base is reminiscent of a 'drunken sailor'.[10] In contrast to the en bloc turning typical of Parkinson’s disease, patients with PSP may pivot carelessly and retropulse, with a risk of falling backwards.[10]
Evaluate postural instability with the pull test.[3][10] This involves the examiner standing behind the patient and first gently pulling both shoulders, then doing so more vigorously a second time to disturb the patient’s balance.[55] An abnormal pull test is confirmed if the patient needs to take more than two steps backwards to regain balance or if they need to be caught.[3]
A sit-to-stand test may reveal altered sequencing due to lack of trunk flexion and anterior weight shift.[10]
Although patients with other less common PSP subtypes may not present with postural instability/falls, all patients will develop this feature as the condition progresses.
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
abnormal vertical eye movements
Vertical oculomotor dysfunction is a cardinal feature of PSP-RS, the most common subtype of PSP.[3] It typically causes the patient difficulty with tasks that require looking downwards (e.g., reading, eating, and walking downstairs).
It usually presents within 2-3 years of symptom onset, usually beginning with slowing of vertical saccades (eye movements) and progressing to vertical supranuclear gaze palsy.[28]
Slow vertical saccades are defined by a slow enough speed of vertical eye movements for the examiner to see the movements in a bedside test. Vertical supranuclear gaze palsy presents as a clear limitation of the range of voluntary gaze in the vertical more than the horizontal plane, affecting both upwards and downwards gaze. Some patients may complain of diplopia or blurred vision due to difficulty with convergence.
To assess the saccades, instruct the patient to shift their gaze between two fixed visual points (such as the index finger and thumb) positioned on the right/left or top/bottom sides of their visual field. First evaluate the horizontal saccades and then proceed to examine the vertical saccades. Normally, the trajectory of the eyeball is so fast that it can hardly be seen to be moving, whereas in PSP the speed of the eyeball movement is so slow that the trajectory can be easily seen.[28] This slowing is seen to affect vertical eyeball movements both earlier than, and to a greater degree than, horizontal eyeball movements.[3][28]
Reduction or loss of the optokinetic nystagmus (OKN), typically tested with OKN strips, confirms the loss of saccades.[10]
Restriction of the vertical range (as opposed to speed) of voluntary eye movements occurs later, with low amplitude of the voluntary vertical gaze.
Use the doll’s head manoeuvre to activate the vertibulo-ocular reflex, thereby confirming the supranuclear nature of gaze palsy (i.e., involuntary vertical eye movements are preserved whereas voluntary eye movements are impaired).[3] This involves asking the patient to fix the eyes on a target while the head is passively moved up and down.
A valuable sign that is not part of the formal PSP diagnostic criteria but can be seen before restriction and slowing of saccades is a curvilinear path on downwards saccades (the 'round-the-houses' sign).[42]
Macro square wave jerks can frequently be seen in patients with PSP and are often an early sign of oculomotor dysfunction.[3] These can be provoked by asking the patient to fixate on a near target with eyes in the primary position. Jerky involuntary movements of small amplitude will be seen that momentarily move the eyes horizontally away from the target followed by returning to the target after an interval of less than a second. These are not specific to PSP but tend to be more frequent, larger movements in PSP than in other conditions in which square wave jerks can occur (e.g., other parkinsonian conditions, Friedreich's ataxia, Huntington's chorea, and multiple sclerosis).[10][56][57]
Although patients with other less common PSP subtypes may not present with vertical oculomotor dysfunction, all patients will develop this feature as the condition progresses.
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
[Figure caption and citation for the preceding image starts]: The “round-the-houses” sign, which can often be seen before restriction and slowing of saccades. Note the lateral curvature of downward path of eye movement (yellow arrows)Rowe JB, et al. Practical Neurology 2021; 21: 376-83; used with permission [Citation ends].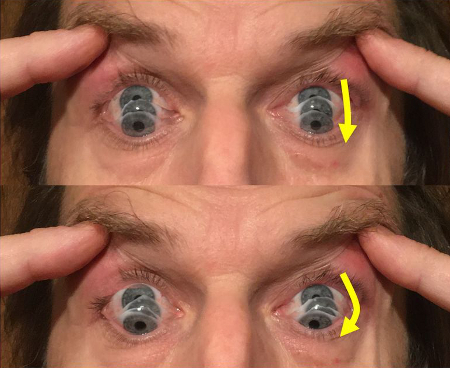
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
parkinsonism
Parkinsonism (bradykinesia, rigidity, and tremor) is a common feature of PSP-RS and is particularly predominant as an early feature of the parkinsonism subtype of PSP (PSP-P).[3][10] Bradykinesia is examined by gait assessment and finger or toe tapping tests, which show significant slowing, and/or dampening of amplitude, compared with healthy individuals. In PSP, bradykinesia and rigidity are typically asymmetric and predominantly axial, affecting the trunk and neck (whereas in Parkinson’s disease the limbs are usually most affected).[3][10] The patient might report neck and back stiffness. Tremor is less frequent in PSP than in Parkinson’s disease and, when present, is usually milder and bilateral.[44]
Freezing of gait can be provoked by asking the patient to pass through a narrow space or to turn around while walking. In the very rare subtype PSP-progressive gait freezing (PSP-PGF), freezing of gait is the predominant symptom in the first year of disease onset, accompanied by bradykinesia and/or rigidity.[51][52][53][54]
If the patient has been previously misdiagnosed with Parkinson’s disease, they might report a poor response of parkinsonism and freezing of gait to levodopa.[3][10]
cognitive dysfunction
Mild cognitive impairment involving mainly the executive domain is frequent early in the disease course, leading to dementia in at least half of patients in more advanced stages.[37][38]Patients usually complain of difficulties planning and multitasking. Memory disturbance is usually characterised by deficits in retrieval, with relatively preserved encoding (learning of new information).[10]
Use a screening scale to evaluate cognition. The Montreal Cognitive Assessment (MoCA) scale is preferred over the Mini Mental State Examination (MMSE) because it is more sensitive in detecting executive dysfunction.[59]
Behavioural and cognitive symptoms are the presenting feature in around 20% of patients with PSP.[10] In the rare subtype PSP with frontal presentation (PSP-F), cognitive dysfunction and behaviour change are the predominant initial symptoms early in the disease course.[10][45][46]
rapidly progressive symptoms
The rapid progression of symptoms can help to distinguish PSP from other parkinsonian disorders. Frequent falls typically occur within the first 1-3 years after symptom onset. Slowing of vertical saccades usually occurs 2-3 years after symptom onset and within 3-4 years the cardinal feature of supranuclear gaze palsy will become unequivocally apparent. Significant early cognitive impairment is also common.[3][28]
Other diagnostic factors
common
speech problems
Speech impairment is an early symptom in half of patients with PSP-RS.[36] Dysarthria eventually affects almost all patients with PSP and has a hypokinetic and/or spastic feature, often accompanied by a strained-strangled or breathy voice quality.[61][62] At advanced stages, the patient may lose the ability to speak (anarthria).
Free speech will reveal most speech and/or language deficits. Language disturbances in PSP are characterised by apraxia of speech and non-fluent aphasia.[3] Apraxia of speech involves difficulty planning and coordinating the movements necessary for speech production, resulting in effortful, halting speech with inconsistent sound errors and distortions, or slow speech with segmented syllables.[3][60] Patients with nonfluent aphasia have reduced fluency and difficulty in generating speech and forming coherent sentences.[3][60]
Progressive apraxia and non-fluent aphasia are the predominant presenting symptom in the rare subtype PSP-speech/language disorder (PSP-SL).[47]
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
dysphagia
Impaired swallowing presents with frequent coughing on swallowing liquids and drooling (sialorrhoea), and usually occurs within 1-2 years after speech disturbances in patients with PSP-RS.[36] At later stages, this can lead to weight loss and aspiration pneumonia.
If not apparent from the history, swallowing function can be evaluated by a water swallow test.
behaviour problems
Apathy and, less frequently, depression are the most common behavioural symptoms in PSP, presenting in about 60% of patients.[39]
Impulsiveness and disinhibition are seen in one third of patients and can lead to behaviours that increase the risk of falls.[33][39] These features usually present as motor recklessness: for example, carelessness when standing and walking to pick up something off the floor despite severe balance/gait problems, or overstuffing the mouth despite impaired swallowing.[3]
Pseudobulbar affect (PBA) may present in some patients and is characterised by labile emotions (e.g., inappropriate episodes of weeping or, less frequently, laughter). Anxiety is less frequent.[39][40]
Behavioural and cognitive symptoms are the presenting feature in around 20% of patients with PSP.[10] In the rare subtype PSP with frontal presentation (PSP-F), cognitive dysfunction and behaviour change are the predominant initial symptoms early in the disease course.[10][45][46]
facial and/or limb dystonia
Facial dystonia can result in deep nasolabial folds and a furrowed brow, giving the appearance of surprise or concern (referred to as the Procerus sign).[3][65]
Disturbances in eyelid motion are frequent, including severely decreased blinking, lid retraction (resulting in a staring appearance), blepharospasm, and eyelid-opening apraxia (see video below). Blepharospasm and eyelid-opening apraxia both result in involuntary eyelid closure. Blepharospasm is caused by active contraction in the orbicularis oculi muscles, which may be amenable to treatment with botulinum toxin, whereas apraxia of eyelid opening is caused by an inability to open the eye due to central mechanisms and is far more difficult to treat.[3][65]
Limb dystonia is usually unilateral, involving an upper limb or one side of the body. It occurs most frequently in the corticobasal syndrome variant of PSP (PSP-CBS) but is also seen in up to one third of patients with PSP-RS.[64]
Neck dystonia, although less frequent, is more specific to PSP (mainly PSP-RS).[3] It may present with retrocollis (with the neck extended and the head pulled back) and can significantly accentuate imbalance and increase risk of falls.
Iankova V, et al; Movement Disorder Society-endorsed PSP Study Group. Parkinsonism Relat Disord 2020 Sep;78:200-3; used with permission
apraxia
Neurological examination will reveal apraxia in many patients with PSP.[66] Apraxia is defined as a disorder of skilled action and tool use despite adequate sensorimotor and cognitive function. It is one of the defining features in the PSP-CBS phenotype, but is also frequently seen in PSP-RS (if the degree of motor impairment allows for appropriate testing).[67]
Bedside tests include asking the patient to copy gestures (e.g., a peace sign or OK sign) or asking the patient to mime how they would use a tool to perform a task (e.g., brushing teeth or stirring coffee).
sleep disturbance
Disordered sleep is an under-recognised feature of PSP and is often progressive, leading to impaired daytime functioning. Patients (or carers) might report insomnia, excessive daytime sleepiness, and sleep fragmentation (e.g., obstructive sleep apnoea, periodic limb movement disorder, and restless leg syndrome), although all of these are also common in other neurodegenerative disorders.[10]
constipation
Constipation affects 71% to 80% of patients with PSP.[10] Putative causes include a sedentary lifestyle, hypodipsia, central dysautonomia, and drug adverse effects.
uncommon
myoclonus
Myoclonus is an important feature of the PSP-CBS phenotype that rarely occurs in PSP-RS.[3] Because the myoclonus in these patients is usually action-induced, it might not be apparent on observation but can be provoked by slightly tapping on outstretched fingers.
pyramidal signs
Pyramidal signs such as brisk muscle stretch reflexes, Babinski sign, Hoffmann sign, or exaggerated jaw jerk are occasionally present in patients with PSP of various phenotypes.[68]
Risk factors
strong
increasing age (>40 years)
exposure to chromate and phosphate
A cluster of PSP-Richardson's syndrome (PSP-RS) and PSP-parkinsonism (PSP-P) with an incidence 12.3 times higher than in the general population was identified in northern France in a small area with severe environmental contamination from historic chromate and phosphate ore processing, linked to textile dyeing and tanning industries.[20]
Use of this content is subject to our disclaimer






