Summary
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Multidisciplinaire richtlijn Postpartumzorg in de eerste lijn (deel 1)Published by: Werkgroep Ontwikkeling Richtlijnen Eerste Lijn (Worel)Last published: 2022Guideline multidisciplinaire des soins postnatals dans la première ligne de soins (partie 1)Published by: Groupe de Travail Développement de recommmandations de première ligneLast published: 2022Multidisciplinaire richtlijn Postpartumzorg in de eerste lijn (deel 2)Published by: Werkgroep Ontwikkeling Richtlijnen Eerste Lijn (Worel)Last published: 2024Guideline multidisciplinaire des soins postnatals dans la première ligne de soins (partie 2)Published by: Groupe de Travail Développement de recommmandations de première ligneLast published: 2024Definition
History and exam
Key diagnostic factors
- estimated blood loss (EBL) ≥500 mL within 24 hours of birth
- uterine atony
- obstetric lacerations and/or expanding haematomas
- signs of hypovolaemia
- retained tissue (placenta, membranes, or placenta accreta spectrum)
- uterine defect on bimanual examination
Other diagnostic factors
- symptoms of hypovolaemia
- uterine tenderness (secondary postpartum haemorrhage [PPH])
- signs of infection (secondary postpartum haemorrhage [PPH])
Risk factors
- placenta previa/low lying placenta
- placenta accreta spectrum
- platelet count <50 × 10⁹/L (<50,000 per microlitre)
- active antepartum bleeding
- inherited coagulopathy
- acquired coagulopathy
- history of PPH in prior delivery
- operative (assisted) vaginal delivery
- current use of therapeutic anticoagulation
- prior caesarean delivery, uterine surgery, or multiple laparotomies
- uterine overdistension (multiple gestation, polyhydramnios, fetal macrosomia with estimated fetal weight >4000 g)
- grand multiparity (>4 prior births)
- large uterine myomas
- class III obesity (BMI >40)
- pre-existing maternal anaemia
- prolonged labour or precipitous delivery
- labour induction or augmentation with prolonged use of oxytocin
- magnesium sulfate use
- caesarean delivery
- placental abruption
- severe pre-eclampsia or HELLP syndrome
- intrauterine fetal demise (IUFD)
- intrapartum infection
- selective serotonin-reuptake inhibitor (SSRI) or serotonin-noradrenaline reuptake inhibitor (SNRI) use in the month before delivery
Diagnostic investigations
1st investigations to order
- quantification of blood loss
- blood type and cross-match
- FBC
- coagulation profile (PT, PTT, INR, fibrinogen)
Investigations to consider
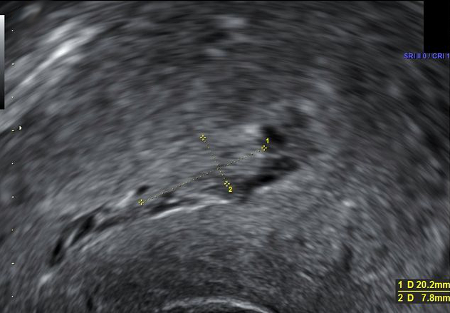
- uterine ultrasound
- inherited coagulation assays
- diagnostic laparotomy
- CT abdomen/pelvis
- vaginal microbiology (secondary PPH)
Emerging tests
- thromboelastography (TEG) or rotational thromboelastometry (ROTEM®)
- app-based blood loss quantification technology
Treatment algorithm
Contributors
Authors
Dena Goffman, MD
Vice Chair for Quality and Patient Safety
Department of Obstetrics and Gynecology
Columbia University Irving Medical Center
New York
NY
Disclosures
DG declares ongoing advisory board roles for Cooper Surgical Obstetrical Safety Council and Organon Jada Scientific Advisory Board; prior PPH educational speaker roles for PRIME, Haymarket, and Laborie; principal investigator for Treating Abnormal Postpartum Uterine Bleeding or Postpartum Hemorrhage with the Jada System-A Postmarket Registry 6/2021 (grant money paid to institution); NIH grant money paid to institution for Effectiveness of Pictographs to Prevent Wrong-Patient Errors in the NICU, and MPI Simulation for Attending Obstetricians to Improve Technical Skills for Managing Postpartum Hemorrhage; none of the above included an obligation to speak on or disseminate product information.
Lilly Liu, MD, MPH
Department of Obstetrics and Gynecology
Columbia University Irving Medical Center
New York
NY
Disclosures
LL declares that she has no competing interests.
Lisa Nathan, MD
Chief of Obstetrics
Department of Obstetrics and Gynecology
Columbia University Irving Medical Center
New York
NY
Disclosures
LN has been paid to speak at an Organon symposium on the Jada System for obstetric hemorrhage management.
Peer reviewers
John C. Smulian, MD, MPH
Chair
Department of Obstetrics and Gynecology
University of Florida College of Medicine
Gainesville
FL
Disclosures
JCS declares that he has no competing interests.
Dilly O. C. Anumba, MBBS, MD, FRCOG, FWACS, LLM
Professor of Obstetrics and Gynaecology
University of Sheffield
Consultant in Obstetrics and Fetomaternal Medicine
Sheffield Teaching Hospitals NHS Foundation Trust
Sheffield
UK
Disclosures
DOCA declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Escobar MF, Nassar AH, Theron G, et al. FIGO recommendations on the management of postpartum hemorrhage 2022. Int J Gynaecol Obstet. 2022 Mar;157 Suppl 1(suppl 1):3-50.Full text Abstract
Hunt BJ, Allard S, Keeling D, et al. A practical guideline for the haematological management of major haemorrhage. Br J Haematol. 2015 Sep;170(6):788-803.Full text Abstract
Committee on Practice Bulletins-Obstetrics. Practice bulletin no. 183: postpartum hemorrhage. Obstet Gynecol. 2017 Oct;130(4):e168-86. Abstract
Royal College of Obstetricians and Gynaecologists. Prevention and management of postpartum haemorrhage: green-top guideline no. 52. BJOG. 2017 Apr;124(5):e106-49.Full text Abstract
World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. 2012 [internet publication].Full text Abstract
American College of Obstetricians and Gynecologists. Safe Motherhood Initiative: obstetric hemorrhage bundle [internet publication].Full text
Goffman D, Ananth CV, Fleischer A, et al. The New York State Safe Motherhood Initiative: early impact of obstetric hemorrhage bundle implementation. Am J Perinatol. 2019 Nov;36(13):1344-50. Abstract
Bienstock JL, Eke AC, Hueppchen NA. Postpartum hemorrhage. N Engl J Med. 2021 Apr 29;384(17):1635-45.Full text Abstract
Main EK, Goffman D, Scavone BM, et al. National partnership for maternal safety: consensus bundle on obstetric hemorrhage. Obstet Gynecol. 2015 Jul;126(1):155-62.Full text Abstract
National Institute for Health and Care Excellence. Intrapartum care. Nov 2025 [internet publication].Full text
World Health Organization. WHO recommendations: uterotonics for the prevention of postpartum haemorrhage. 2018 [internet publication].Full text Abstract
World Health Organization. WHO recommendation on routes of oxytocin administration for the prevention of postpartum haemorrhage after vaginal birth. 2020 [internet publication].Full text Abstract
World Health Organization. WHO recommendations on the assessment of postpartum blood loss and use of a treatment bundle for postpartum haemorrhage. 2023 [internet publication].Full text Abstract
Althabe F, Therrien MNS, Pingray V, et al. Postpartum hemorrhage care bundles to improve adherence to guidelines: a WHO technical consultation. Int J Gynaecol Obstet. 2020 Mar;148(3):290-9.Full text Abstract
World Health Organization. WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. 2017 [internet publication]Full text Abstract
Reference articles
A full list of sources referenced in this topic is available here.
Use of this content is subject to our disclaimer