Approach
A thorough history reveals the diagnosis in 80% to 85% of patients.[60] It is also useful in differentiating oropharyngeal dysphagia from oesophageal dysphagia.
Patients with oral dysphagia most often have problems in initiating the voluntary swallow, with difficulty chewing and controlling food or fluid in their mouth, and transferring a bolus posteriorly.
Pharyngeal dysphagia leads to a range of symptoms including nasal regurgitation, the sensation of residue in the throat after swallowing, difficulty initiating the involuntary pharyngeal stage of swallowing, coughing, choking, or wet voice quality after swallowing.
Patients with oesophageal dysphagia often report food sticking in their lower neck or mid-chest region. Patients may use different manoeuvres to help the food passing the oesophagus, or they may sip water to relieve the obstruction.
The key tests used for the evaluation of dysphagia are oesophagogastroduodenoscopy (OGD), videofluoroscopic swallow study, barium x-ray, fibre-optic nasopharyngeal laryngoscopy, or oesophageal manometry. However, the choice of specific testing depends on the clinical presentation.
History
Age: dysphagia with food impaction in a young, adult, white male should raise suspicion for eosinophilic oesophagitis.[43] In a patient >40 years of age this is commonly due to Schatzki ring.[61] Concern for oesophageal cancer must lead to investigation in patients older than 50 years of age.
Symptom onset: dysphagia primarily to solid foods is probably indicative of a structural lesion, whereas dysphagia to both solid and liquid from the onset of symptoms is most likely to be due to motility or neurological disorders of the pharynx or oesophagus.[62][63]
Duration and progression of symptoms: rapid progression of dysphagia, particularly with weight loss, is suggestive of malignancy, whereas patients with peptic strictures usually have long-standing history of dysphagia. Oesophageal rings tend to cause intermittent solid food dysphagia; however, stricture and cancer cause progressive dysphagia.
Site of dysphagia: the site where the patient localises dysphagia is of limited value; however, retrosternal or epigastric dysphagia usually corresponds with the location of the lesion, whereas suprasternal dysphagia is usually referred from the hypopharynx or lower in the oesophagus.[62][64] In one study of 139 patients 21.6% exactly localised the level of obstruction, with over half being within 2 cm. 15% of patients with a distal oesophageal aetiology for their symptoms believed the source was their throat.[64]
Associated symptoms: difficulty initiating a swallow along with coughing, choking, hoarseness, gagging, nasal regurgitation, aspiration pneumonias, and weight loss are more suggestive of oropharyngeal dysphagia. Neurological signs and symptoms may also present in patients with oropharyngeal dysphagia. Chest pain is often seen in idiopathic achalasia and diffuse oesophageal spasm.[35] Previous history of heartburn is suggestive of peptic stricture.
Medication history: radiation- and/or chemotherapy-induced oral mucositis may cause dysphagia. A thorough medication history should be elicited.
Physical examination
There are no specific examination findings for dysphagia, but there may be findings suggestive of the cause: for example, slurred speech, haemiplegia in stroke, or scleroderma manifestations.
A thorough head and neck examination should be performed in all patients, including examination of the oral cavity. The neck should be palpated to evaluate for lymphadenopathy associated with infections or metastatic tumours, thyroid masses or thyromegaly, and hyolaryngeal elevation during swallowing. Neurological examination including examination of the cranial nerves is also required. Cranial neuropathies (e.g., glossopharyngeal, vagus nerve) can cause severe dysphagia. See Assessment of cranial nerve mononeuropathy.
Fibre-optic nasopharyngoscopy/laryngoscopy should be performed as part of the initial examination. This is a routine office or bedside awake endoscopy to evaluate structure and some functional aspects of the oropharynx and larynx. Although cricopharyngeus and oesophagus are not visualised, pooling of secretions can suggest dysfunction.[Figure caption and citation for the preceding image starts]: Larynx as a result of cricopharyngeal dysfunctionFrom the collection of Dr S. Charous [Citation ends].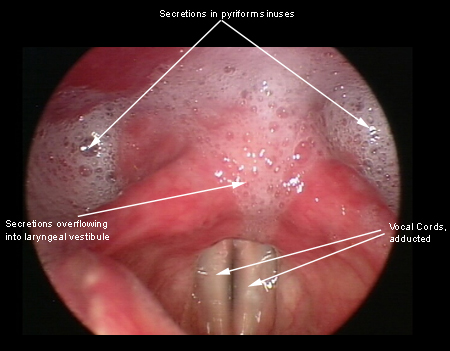
Investigations
Patients presenting with associated neurological symptoms or physical findings without other aetiologies for dysphagia may require further evaluation. For patients with dysphagia in which an obvious aetiology is not identified based on a history and physical examination (including nasopharyngoscopy/laryngoscopy), a modified barium swallow, flexible endoscopic evaluation of swallowing (FEES), oesophagram or transnasal oesophagoscopy (or a combination) will be the necessary initial tests required. Laboratory assessment is usually ordered in oropharyngeal dysphagia to assess the neuromuscular causes:[12][65]
Thyroid function test (thyromegaly)
Cerebrospinal fluid analysis (multiple sclerosis)
Botulinum toxin assay
Liver enzymes
Ceruloplasmin levels (Wilson's disease)
24-hour urinary copper (Wilson's disease)
Creatine phosphokinase (inflammatory myopathies)
Acetylcholine receptor antibodies (myasthenia gravis)
Anti-DNA and antinuclear antibodies (scleroderma).
Standardised bedside swallowing assessment
Remains an important early screening tool for dysphagia and aspiration risk, however, it is not reliable for detection of silent aspiration.
Variable sensitivity and specificity depending on the method used.
Trial swallow tests using different viscosities are more sensitive than using water. However, combining swallow tests with pulse oximetry (oxygen desaturation ≥2%) using subjective aspiration assessments has the highest sensitivity (63% to 98%).[66]
Usually nurse-led and can help identify which patients need referral for swallow assessment by a speech and swallowing therapist.
Specific investigational studies:
Transnasal oesophagoscopy
Barium swallow (or oesophagram)
Radiographic examination of the oesophagus is indicated for the detection of structural abnormalities that OGD fails to identify; also useful in detecting pharyngeal motility disorders.
Double-contrast views are best for detecting mucosal lesions (e.g., tumours, oesophagitis). Prone single-contrast views are best for detecting lower oesophageal rings or strictures, as the distal oesophagus is inadequately distended when the patient is upright.[1][69][70]
Videofluoroscopic swallow study (also known as modified barium swallow study)
A videofluoroscopic swallow study is performed by a radiologist and speech therapist on patients with oropharyngeal dysphagia.
It focuses on the oral cavity, pharynx, and cervical oesophagus, recording to assess abnormalities of both the oral and pharyngeal phases of swallowing.
Reveals oropharyngeal dysfunction as well as the risk of aspiration during swallowing in such groups of patients.
Patients are given various consistencies of radio-opaque fluids to swallow; hence, the study is helpful in finding the optimal diet, by which the risk of aspiration is minimised.[1][71]
The assessment is also used to trial compensatory or rehabilitative maneuvers and strategies which may have therapeutic benefit for the patient or improve their swallowing safety and efficiency.
A standardised oesophageal screening protocol can be performed by a speech therapist in addition to the standard videofluoroscopic swallow study.[72]
Flexible Endoscopic Evaluation of Swallowing (FEES)
Complementary to the videofluoroscopic swallow study in evaluating oropharyngeal swallowing and laryngeal pathology, including laryngeal penetration and aspiration.
An excellent addition to the bedside swallow in determining risk of aspiration, especially in the bedridden patient.
The sensory testing aspect of FEES with sensory testing utilises an air pulse stimulus of mechanoreceptors within the larynx.[73]
Biphasic oesophagram
Permits detection of both structural and functional abnormalities of the oesophagus.
Double-contrast views are best for detecting mucosal lesions (e.g., tumours, oesophagitis).
Prone single-contrast views with continuous drinking of low-density barium are best for detecting lower oesophageal rings or strictures.[1]
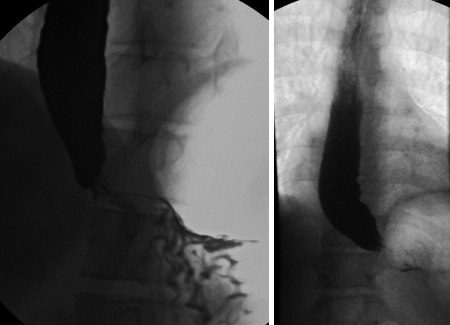
Timed barium oesophagogram
Simple, non-invasive, widely available barium technique for evaluating oesophageal emptying in patients with achalasia.
The films are taken at 1, 2, and 5 minutes after the last swallow of barium; the purpose of 2-minute film is to assess interim emptying.[35][Figure caption and citation for the preceding image starts]: Idiopathic achalasia: barium oesophagograms showing a dilated oesophageal body and a tapering stricture in the distal oesophagus ('bird's beak')From the collection of Dr S. Charous [Citation ends].
May be required following initial studies, as described above.
It reveals structural abnormalities as well as providing the opportunity to perform therapeutic intervention such as balloon dilatation in idiopathic achalasia and resection of webs.
Oesophageal biopsies taken during endoscopy, if positive, may confirm conditions such as eosinophilic oesophagitis, carcinoma, or gastro-oesophageal reflux disease as the cause of oesophageal dysphagia.
Oesophageal dilation at the time of endoscopy can be therapeutic for multiple disorders such as Schatzki rings, stricture, or stenoses.
Oesophageal manometry
A diagnostic study that measures intraluminal pressure as well as co-ordination activity of the upper and lower oesophagus sphincter and the oesophageal body.
Solid-state, multi-channel catheters allow increased accuracy in evaluating oesophageal motility.
The diagnostic study of choice in patients with suspected motility abnormalities without evidence of mechanical obstruction.[74]
Also used for evaluation of dysphagia in patients treated for achalasia or who have undergone antireflux surgery.
Surface electromyography
This is a simple, radiation-free method for screening and preliminary differentiation between oral and pharyngeal dysphagia.
The needle electrodes are used within swallowing muscles in the neck to record the timing of muscle contraction patterns and amplitude of electronic activity of the muscles during swallowing.
Dysphagia following oral cavity conditions prolongs drinking time and decreases the activity of the masseter, but it does not affect pharynx and submental muscles.
Not appropriate for the diagnosis of suspected neurogenic dysphagia.
Muscle tension dysphagia is a diagnosis of exclusion made with speech therapists. It cannot be diagnosed thus far with conventional testing.[20] The minimum assessment should include a comprehensive clinical swallow evaluation (with thorough history and head and neck examination), laryngoscopic evaluation of the larynx and pharynx, instrumental evaluation of oropharyngeal swallowing, and oesophageal evaluation.[21]
Use of this content is subject to our disclaimer