Pathology involving the tongue, floor of mouth, palate, tonsils, or other oral cavity structures can lead to oral phase dysphagia. The problem in this scenario is often recognised as difficulty with initiating the swallow.
Pharyngeal disorders can cause dysphagia when dysfunction of the base of tongue, pharynx, larynx, or cricopharyngeal muscle occurs. This may be manifest by reports of food sticking in the throat, symptoms of aspiration, hoarseness, cough, pain in the throat, or even referred pain to the ear.
Oesophageal dysphagia may be as a result of oesophageal motility disorders, intrinsic or extrinsic masses, webs, rings, reflux disease, or lower oesophageal sphincter disorders. These pathologies will more likely present with sensation of food sticking in the lower aspect of the neck or chest, regurgitation of food, chest pain, or heartburn.
Dysphagia is often multifactorial in nature. For example, an elderly patient may have weak pharyngeal musculature, with cervical osteophytes and oesophageal reflux. Each issue alone may not be problematic, but combined they may cause significant dysphagia.
Oropharyngeal infection/inflammation
Infections such as pharyngitis, oesophageal candidiasis, epiglottitis, and retropharyngeal abscess can cause dysphagia, as can radiation- and/or chemotherapy-induced oral mucositis and immune-mediated oesophageal disorders.[9]Reddy CA, McGowan E, Yadlapati R, et al. AGA clinical practice update on esophageal dysfunction due to disordered immunity and infection: expert review. Clin Gastroenterol Hepatol. 2024 Dec;22(12):2378-87.
https://www.cghjournal.org/action/showPdf
http://www.ncbi.nlm.nih.gov/pubmed/39436337?tool=bestpractice.com
[10]Hutcheson KA, Lewin JS. Functional outcomes after chemoradiotherapy of laryngeal and pharyngeal cancers. Curr Oncol Rep. 2012 Apr;14(2):158-65.
http://www.ncbi.nlm.nih.gov/pubmed/22249533?tool=bestpractice.com
Oral cavity structural abnormalities
Hypertrophic tonsils
Causes dysphagia for solids by interfering with transfer of bolus from oral cavity to pharynx.
May be associated with obstructive sleep apnoea, recurrent infections, and snoring.
Lingual tonsils (at the base of the tongue) may be difficult to visualise but may also become hypertrophic and interfere with swallowing. Can be visualised with flexible nasopharyngoscopy or indirect laryngoscopy with a dental mirror.[Figure caption and citation for the preceding image starts]: Hypertrophic tonsils causing severely narrowed pharyngeal openingFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
Oral cavity tumours (especially cancers)
Can affect any of the structures in the oral cavity and become large enough to cause obstruction and prevent food passage.
Can affect function of any of the structures by invasion into surrounding tissue: for example, carcinoma of the tongue with floor of mouth invasion that leads to impaired tongue mobility, resulting in difficulty swallowing.
More common in smokers and alcohol drinkers.
Becoming more common in non-smokers because of human papillomavirus-induced squamous cell carcinomas involving the tonsils and base of the tongue.
Often associated with pain, altered speech, neck mass, or bloody sputum.
Dentition
Oropharyngeal structural abnormalities
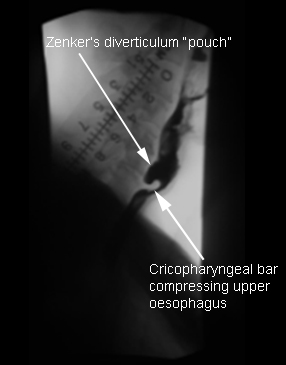
Zenker's diverticulum
Located proximal to upper oesophageal sphincter.
The incidence increases by age; more frequent in women.
Prevalence 50% in seventh and eighth decades.
Is associated with regurgitation of undigested food, intermittent solid food dysphagia, halitosis, and excessive salivation.
Barium swallow is the best diagnostic test.[Figure caption and citation for the preceding image starts]: Zenker’s diverticulum: lateral view with barium oesophagramFrom the collection of Dr S. Charous, Clinical Professor of Otolaryngology - Head and Neck Surgery, Loyola University Medical Center; used with permission. [Citation ends].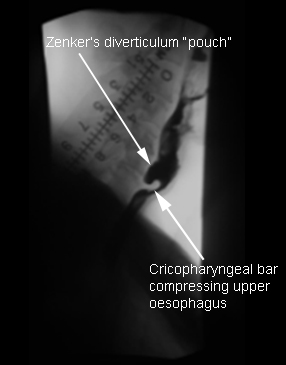
Can be missed or difficult to visualise on oesophageal endoscopy.[11]Cassivi SD, Deschamps C, Nichols FC, et al. Diverticula of the esophagus. Surg Clin North Am. 2005 Jun;85(3):495-503, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15927646?tool=bestpractice.com
Pharyngeal/laryngeal tumours
Symptoms may include progressive solid food dysphagia, weight loss, and otalgia (referred pain).
Hoarseness, symptoms of aspiration (especially of liquids), and shortness of breath are often associated with laryngeal tumours.
Vast majority of malignancies are squamous cell carcinomas, often very aggressive when this is the primary site with frequent metastases.
Endoscopy with biopsy is the best diagnostic test.[12]Cook IJ, Kahrilas PJ. AGA technical review on the management of oropharyngeal dysphagia. Gastroenterology. 1999 Feb;116(2):455-78.
http://www.ncbi.nlm.nih.gov/pubmed/9922328?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Laryngeal/pharyngeal squamous cell carcinomaFrom the collection of Dr S. Charous [Citation ends].
Stenosis
Mostly caused by prior radiation, surgery, or chemical ingestion.
May be idiopathic, but this is rare.
Presents as solid food dysphagia or symptoms of aspiration.
Flexible fibre-optic nasopharyngoscopy/laryngoscopy, oesophagogastroduodenoscopy (OGD), and barium swallow are helpful.
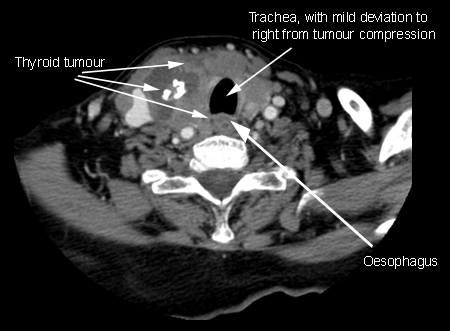
Extrinsic compression
Cervical lymphadenopathy, cricopharyngeal bar, cervical spine osteophytes, or thyromegaly.[Figure caption and citation for the preceding image starts]: Endoscopic view of pharynx showing osteophytes pressing inwards on posterior pharyngeal wall, obscuring view of larynx with epiglottis in backgroundFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].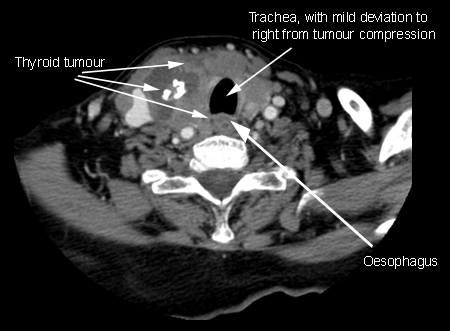
Flexible fibre-optic nasopharyngoscopy/laryngoscopy and barium swallow can usually identify the defect.
Velopharyngeal insufficiency
Usually due to tumours, surgical resection of the palate, radiation to the palate, or cleft palate. Other causes include stroke, other brain pathology, or high-level vagus nerve injuries.
Associated with hypernasal speech. Nasal regurgitation (of liquids more than solids) can occur.[13]Lynch CA, Rule DW, Klaben B, et al. Surgical treatment of acquired velopharyngeal insufficiency in adults with dysphagia and dysphonia. J Voice. 2024 Jul;38(4):911-7.
http://www.ncbi.nlm.nih.gov/pubmed/35027239?tool=bestpractice.com
[14]Shprintzen RJ, Marrinan E. Velopharyngeal insufficiency: diagnosis and management. Curr Opin Otolaryngol Head Neck Surg. 2009 Aug;17(4):302-7.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2810137
http://www.ncbi.nlm.nih.gov/pubmed/19448542?tool=bestpractice.com
[15]Rudnick EF, Sie KC. Velopharyngeal insufficiency: current concepts in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg. 2008 Dec;16(6):530-5.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2810137
http://www.ncbi.nlm.nih.gov/pubmed/19005324?tool=bestpractice.com
Oropharyngeal neuromuscular abnormalities
Neuromuscular discoordination, involving the central nervous system and or the peripheral nervous system, can result in oral or pharyngeal dysphagia.[16]Rothstein RD. A systematic approach to a patient with dysphagia. Hosp Pract (Minneap). 1997 Mar 15;32(3):169-75.
http://www.ncbi.nlm.nih.gov/pubmed/9078978?tool=bestpractice.com
Neurological examination and evaluation of neurological symptoms are helpful in directing the physician to the underlying aetiology of the dysfunction. The following are common neuromuscular causes of oral or pharyngeal dysphagia; stroke in this group is the most common cause:
Stroke: approximately 40% to 70% of people with stroke experience dysphagia[2]World Gastroenterology Organisation. WGO practice guideline - dysphagia. Sep 2014 [internet publication].
http://www.worldgastroenterology.org/guidelines/global-guidelines/dysphagia
Parkinson's disease[17]Sapir S, Ramig L, Fox C. Speech and swallowing disorders in Parkinson disease. Curr Opin Otolaryngol Head Neck Surg. 2008 Jun;16(3):205-10.
http://www.ncbi.nlm.nih.gov/pubmed/18475072?tool=bestpractice.com
[18]Potulska A, Friedman A, Królicki L, et al. Swallowing disorders in Parkinson's disease. Parkinsonism Relat Disord. 2003 Aug;9(6):349-53.
http://www.ncbi.nlm.nih.gov/pubmed/12853234?tool=bestpractice.com
Vocal cord paralysis
Amyotrophic lateral sclerosis
Multiple sclerosis
Brain and skull base tumours
Post-operative resections of skull base or brain tumours (especially and often involving cranial nerves IX, X, and XII)
Sjogren’s syndrome[19]Mandl T, Ekberg O, Wollmer P, et al. Dysphagia and dysmotility of the pharynx and oesophagus in patients with primary Sjögren’s syndrome. Scand J Rheumatol. 2007 Sep-Oct;36(5):394-401.
http://www.ncbi.nlm.nih.gov/pubmed/17963171?tool=bestpractice.com
Myasthenia gravis
Inflammatory myopathies
Wilson's disease
Progressive supranuclear palsy
Oculopharyngeal muscular dystrophy
Muscle tension dysphagia, which describes excessive laryngeal and pharyngeal tension that disrupts swallowing; it is a diagnosis of exclusion made with speech therapists and cannot yet be diagnosed with conventional testing.[20]Kang CH, Hentz JG, Lott DG. Muscle tension dysphagia: symptomology and theoretical framework. Otolaryngol Head Neck Surg. 2016 Nov;155(5):837-42.
http://www.ncbi.nlm.nih.gov/pubmed/27352887?tool=bestpractice.com
The minimum assessment should include a comprehensive clinical swallow evaluation (with thorough history and head and neck examination), laryngoscopic evaluation of the larynx and pharynx, videofluoroscopic swallow study (also known as modified barium swallow study), and oesophageal evaluation.[21]Lott DG, Rosow CHK, Curtis JA, et al. The diagnosis of muscle tension dysphagia. Bulletin. 2023 Aug 17; 44(4).
https://bulletin.entnet.org/clinical-patient-care/article/22870225/the-diagnosis-of-muscle-tension-dysphagia
Oesophageal structural abnormalities
Stricture
The main symptom is solid food dysphagia.
OGD or barium oesophagrams are the best diagnostic test.
Dysphagia is most prevalent when the luminal diameter is <15 mm (normal is 20 mm).[22]Schatzki R. The lower esophageal ring: long term follow-up of symptomatic and asymptomatic rings. Am J Roentegenol Radiat Ther Nucl Med. 1963 Oct;90:805-10.
http://www.ncbi.nlm.nih.gov/pubmed/14068418?tool=bestpractice.com
Acid reflux accounts for 60% to 70% of cases of strictures and mainly occurs in the region of the lower oesophageal sphincter.[23]Palmer ED. The hiatus hernia-esophagitis-esophageal stricture complex: twenty year prospective study. Am J Med. 1968 Apr;44(4):566-79.
http://www.ncbi.nlm.nih.gov/pubmed/4868278?tool=bestpractice.com
Caustic agents and radiotherapy may lead to strictures.
Pills such as potassium chloride, doxycycline, quinidine, non-steroidal anti-inflammatory drugs, iron, and alendronic acid may cause strictures.[24]Kikendall JW. Pill-induced esophageal injury. Gastroenterol Clin North Am. 1991 Dec;20(4):835-46.
http://www.ncbi.nlm.nih.gov/pubmed/1787016?tool=bestpractice.com
Intramural lesions
Foreign body: acute dysphagia could occur as a result of foreign bodies and food impaction in the oesophagus. These most often will obstruct at the level of the upper or lower oesophageal sphincters.
Oesophageal/cardia carcinomas: patients typically present with reflux in early disease, and dysphagia and odynophagia in locally advanced or late disease.[25]Thrumurthy SG, Chaudry MA, Thrumurthy SSD, et al. Oesophageal cancer: risks, prevention, and diagnosis. BMJ. 2019 Jul 9;366:l4373.
https://www.bmj.com/content/366/bmj.l4373.full
http://www.ncbi.nlm.nih.gov/pubmed/31289038?tool=bestpractice.com
Dysphagia alone or with unintentional weight loss is the most common presenting symptom.[26]Astin MP, Martins T, Welton N, et al. Diagnostic value of symptoms of oesophagogastric cancers in primary care: a systematic review and meta-analysis. Br J Gen Pract. 2015 Oct;65(639):e677-91.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4582881
http://www.ncbi.nlm.nih.gov/pubmed/26412845?tool=bestpractice.com
Adenocarcinoma and squamous cell carcinoma account for the vast majority of all cases of oesophageal cancer.[27]Then EO, Lopez M, Saleem S, et al. Esophageal cancer: an updated surveillance epidemiology and end results database analysis. World J Oncol. 2020 Apr;11(2):55-64.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7141161
http://www.ncbi.nlm.nih.gov/pubmed/32284773?tool=bestpractice.com
[28]GBD 2017 Oesophageal Cancer Collaborators. The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020 Jun;5(6):582-97.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7232026
http://www.ncbi.nlm.nih.gov/pubmed/32246941?tool=bestpractice.com
Squamous cell carcinoma is often associated with alcohol and tobacco consumption, and with human papillomavirus infection; adenocarcinoma with gastro-oesophageal reflux disease (GORD), Barrett’s oesophagus, high body mass index, and male sex.[25]Thrumurthy SG, Chaudry MA, Thrumurthy SSD, et al. Oesophageal cancer: risks, prevention, and diagnosis. BMJ. 2019 Jul 9;366:l4373.
https://www.bmj.com/content/366/bmj.l4373.full
http://www.ncbi.nlm.nih.gov/pubmed/31289038?tool=bestpractice.com
Approximately 75% of all oesophageal adenocarcinomas are located in the distal oesophagus, whereas squamous cell carcinomas occur more frequently in the proximal-to-middle oesophagus.[29]Obermannová R, Alsina M, Cervantes A, et al. Oesophageal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Oct;33(10):992-1004.
https://www.annalsofoncology.org/article/S0923-7534(22)01850-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35914638?tool=bestpractice.com
[30]Rustgi AK, El-Serag HB. Esophageal carcinoma. N Engl J Med. 2014 Dec 25;371(26):2499-509.
http://www.ncbi.nlm.nih.gov/pubmed/25539106?tool=bestpractice.com
OGD with biopsy is usually diagnostic.[31]Pasha SF, Acosta RD, Chandrasekhara V, et al; ASGE Standards of Practice Committee. The role of endoscopy in the evaluation and management of dysphagia. Gastrointest Endosc. 2014 Feb;79(2):191-201.
http://www.giejournal.org/article/S0016-5107%2813%2902209-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24332405?tool=bestpractice.com
Benign tumours: rare; include leiomyoma, granular cell tumours, and papillomas.
Oesophageal metastases: metastasis to the oesophagus is rare, but most frequently occurs in the context of advanced lung or breast cancer. Other possible primary carcinomas include ovarian and colonic cancer.[32]Thomasset SC, Garcea G, Berry DP. Oesophageal metastasis from colorectal cancer. Case Rep Gastroenterol. 2008 Feb 19;2(1):40-4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3075164
http://www.ncbi.nlm.nih.gov/pubmed/21490836?tool=bestpractice.com
Extramural lesions compressing the oesophagus
Mediastinal masses
Bronchial carcinoma
Cervical osteoarthritis/cervical osteophytes[33]Carlson ML, Archibald DJ, Graner DE, et al. Surgical management of dysphagia and airway obstruction in patients with prominent ventral cervical osteophytes. Dysphagia. 2011 Mar;26(1):34-40.
http://www.ncbi.nlm.nih.gov/pubmed/20099000?tool=bestpractice.com
Patients usually have symptoms of underlying disease with recently added solid food dysphagia
Best diagnosed with barium study.[12]Cook IJ, Kahrilas PJ. AGA technical review on the management of oropharyngeal dysphagia. Gastroenterology. 1999 Feb;116(2):455-78.
http://www.ncbi.nlm.nih.gov/pubmed/9922328?tool=bestpractice.com
Oesophageal ring
Manifest by intermittent solid food dysphagia; if found presumed to be the cause of symptoms.
Mucosal ring (Schatzki ring): prevalence of 0.2% to 1.4%. Located at gastro-oesophageal junction.
Muscular rings: located 1.5 cm proximal to the gastro-oesophageal junction. Typically asymptomatic.[34]Tobin RW. Esophageal rings, webs, and diverticula. J Clin Gastroenterol. 1998 Dec;27(4):285-95.
http://www.ncbi.nlm.nih.gov/pubmed/9855256?tool=bestpractice.com
Anatomical abnormalities
Oesophageal diverticulum: known as traction diverticulum secondary to pulling of the oesophageal wall. Located in the middle third of the oesophagus. Barium study is the most useful test to identify them.
Hiatus hernia: is typically asymptomatic, associated with GORD, and can cause bleeding and incarceration.
Webs: found in 5% to 15% of patients with benign causes of dysphagia who undergo OGD.[34]Tobin RW. Esophageal rings, webs, and diverticula. J Clin Gastroenterol. 1998 Dec;27(4):285-95.
http://www.ncbi.nlm.nih.gov/pubmed/9855256?tool=bestpractice.com
Oesophageal motor abnormalities
Idiopathic achalasia
Oesophageal motility disease with insufficient lower oesophageal sphincter relaxation and loss of oesophageal peristalsis.
Progressive dysphagia to solids followed by liquids is seen in 82% to 100% of patients.
Oesophageal manometry is useful in detecting motility abnormalities of achalasia.[35]Farrokhi F, Vaezi MF. Idiopathic (primary) achalasia. Orphanet J Rare Dis. 2007 Sep 26;2:38.
http://www.ojrd.com/content/2/1/38
http://www.ncbi.nlm.nih.gov/pubmed/17894899?tool=bestpractice.com
[36]Patti MG, Gorodner MV, Gulvani C, et al. Spectrum of esophageal motility disorders: implications for diagnosis and treatment. Arch Surg. 2005 May;140(5):442-8; discussion 448-9.
http://www.ncbi.nlm.nih.gov/pubmed/15897439?tool=bestpractice.com
[37]Lacy BE, Weiser K. Esophageal motility disorders: medical therapy. J Clin Gastroenterol. 2008 May-Jun;42(5):652-8.
http://www.ncbi.nlm.nih.gov/pubmed/18364589?tool=bestpractice.com
[38]Smout AJ. Advances in esophageal motor disorders. Curr Opin Gastroenterol. 2008 Jul;24(4):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/18622164?tool=bestpractice.com
Scleroderma
Causes oesophageal hypomotility and incompetence of lower oesophageal sphincter.
Can lead to chronic gastro-oesophageal reflux with subsequent stricture formation.
Oesophageal manometry along with clinical correlation is helpful in diagnosis.[39]Richter JE. Oesophageal motility disorders. Lancet. 2001 Sep 8;358(9284):823-8.
http://www.ncbi.nlm.nih.gov/pubmed/11564508?tool=bestpractice.com
Diffuse oesophageal spasm
Mostly manifest by recurrent chest pains associated with meals.
More common with ingestion of very hot or very cold foods.
Is diagnosed by manometry, which reveals simultaneous contractions.[36]Patti MG, Gorodner MV, Gulvani C, et al. Spectrum of esophageal motility disorders: implications for diagnosis and treatment. Arch Surg. 2005 May;140(5):442-8; discussion 448-9.
http://www.ncbi.nlm.nih.gov/pubmed/15897439?tool=bestpractice.com
[37]Lacy BE, Weiser K. Esophageal motility disorders: medical therapy. J Clin Gastroenterol. 2008 May-Jun;42(5):652-8.
http://www.ncbi.nlm.nih.gov/pubmed/18364589?tool=bestpractice.com
[38]Smout AJ. Advances in esophageal motor disorders. Curr Opin Gastroenterol. 2008 Jul;24(4):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/18622164?tool=bestpractice.com
[40]Richter JE, Castell DO. Diffuse esophageal spasm: reappraisal. Ann Intern Med. 1984 Feb;100(2):242-5.
http://www.ncbi.nlm.nih.gov/pubmed/6691670?tool=bestpractice.com
Finding on barium swallow study is 'corkscrew' oesophageal body from a simultaneous contraction.[36]Patti MG, Gorodner MV, Gulvani C, et al. Spectrum of esophageal motility disorders: implications for diagnosis and treatment. Arch Surg. 2005 May;140(5):442-8; discussion 448-9.
http://www.ncbi.nlm.nih.gov/pubmed/15897439?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Corkscrew oesophagus from diffuse oesophageal spasm seen on a barium swallow studyFrom the collection of Dr S. Charous [Citation ends].
Hypocontracting oesophagus
Can be diagnosed with oesophagram or manometry.[37]Lacy BE, Weiser K. Esophageal motility disorders: medical therapy. J Clin Gastroenterol. 2008 May-Jun;42(5):652-8.
http://www.ncbi.nlm.nih.gov/pubmed/18364589?tool=bestpractice.com
[38]Smout AJ. Advances in esophageal motor disorders. Curr Opin Gastroenterol. 2008 Jul;24(4):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/18622164?tool=bestpractice.com
Nutcracker oesophagus
Is associated with chest pain.
Normal peristalsis with increased distal oesophageal mean amplitudes and hypertensive lower oesophageal sphincter.
Manometry is required for diagnosis.[36]Patti MG, Gorodner MV, Gulvani C, et al. Spectrum of esophageal motility disorders: implications for diagnosis and treatment. Arch Surg. 2005 May;140(5):442-8; discussion 448-9.
http://www.ncbi.nlm.nih.gov/pubmed/15897439?tool=bestpractice.com
[37]Lacy BE, Weiser K. Esophageal motility disorders: medical therapy. J Clin Gastroenterol. 2008 May-Jun;42(5):652-8.
http://www.ncbi.nlm.nih.gov/pubmed/18364589?tool=bestpractice.com
[38]Smout AJ. Advances in esophageal motor disorders. Curr Opin Gastroenterol. 2008 Jul;24(4):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/18622164?tool=bestpractice.com
[41]Katz PO, Dalton CB, Richter JE, et al. Esophageal testing of patients with noncardiac chest pain and/or dysphagia: result of a three year experience with 1161 patients. Ann Intern Med. 1987 Apr;106(4):593-7.
http://www.ncbi.nlm.nih.gov/pubmed/3826958?tool=bestpractice.com
Eosinophilic oesophagitis
Chronic immune-mediated condition often associated with concurrent allergic diseases including food allergies, allergic rhinitis, atopic dermatitis, or asthma.[42]Chen JW, Kao JY. Eosinophilic esophagitis: update on management and controversies. BMJ. 2017 Nov 13;359:j4482.
http://www.ncbi.nlm.nih.gov/pubmed/29133286?tool=bestpractice.com
[43]Dhar A, Haboubi HN, Attwood SE, et al. British Society of Gastroenterology (BSG) and British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN) joint consensus guidelines on the diagnosis and management of eosinophilic oesophagitis in children and adults. Gut. 2022 Aug;71(8):1459-87.
https://gut.bmj.com/content/71/8/1459
http://www.ncbi.nlm.nih.gov/pubmed/35606089?tool=bestpractice.com
Three times more common in men than in women.[43]Dhar A, Haboubi HN, Attwood SE, et al. British Society of Gastroenterology (BSG) and British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN) joint consensus guidelines on the diagnosis and management of eosinophilic oesophagitis in children and adults. Gut. 2022 Aug;71(8):1459-87.
https://gut.bmj.com/content/71/8/1459
http://www.ncbi.nlm.nih.gov/pubmed/35606089?tool=bestpractice.com
[44]Garber JJ, Lochhead PJ, Uchida AM, et al. Increasing incidence of eosinophilic esophagitis in Sweden: a nationwide population study. Esophagus. 2022 Oct;19(4):535-41.
https://www.doi.org/10.1007/s10388-022-00926-5
http://www.ncbi.nlm.nih.gov/pubmed/35654916?tool=bestpractice.com
[45]Kapel RC, Miller JK, Torres C, et al. Eosinophilic esophagitis: a prevalent disease in the United States that affects all age groups. Gastroenterology. 2008 May;134(5):1316-21.
https://www.gastrojournal.org/article/S0016-5085(08)00248-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/18471509?tool=bestpractice.com
Eosinophilic oesophagitis appears to be more common in white people than in African-Americans or Asian people.[46]Mansoor E, Cooper GS. The 2010-2015 prevalence of eosinophilic esophagitis in the USA: a population-based study. Dig Dis Sci. 2016 Oct;61(10):2928-34.
https://www.doi.org/10.1007/s10620-016-4204-4
http://www.ncbi.nlm.nih.gov/pubmed/27250980?tool=bestpractice.com
[47]Moawad FJ, Dellon ES, Achem SR, et al. Effects of race and sex on features of eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2016 Jan;14(1):23-30.
https://www.cghjournal.org/article/S1542-3565(15)01193-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/26343181?tool=bestpractice.com
The peak incidence is seen in young adults and in the third and fourth decades of life.[43]Dhar A, Haboubi HN, Attwood SE, et al. British Society of Gastroenterology (BSG) and British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN) joint consensus guidelines on the diagnosis and management of eosinophilic oesophagitis in children and adults. Gut. 2022 Aug;71(8):1459-87.
https://gut.bmj.com/content/71/8/1459
http://www.ncbi.nlm.nih.gov/pubmed/35606089?tool=bestpractice.com
[44]Garber JJ, Lochhead PJ, Uchida AM, et al. Increasing incidence of eosinophilic esophagitis in Sweden: a nationwide population study. Esophagus. 2022 Oct;19(4):535-41.
https://www.doi.org/10.1007/s10388-022-00926-5
http://www.ncbi.nlm.nih.gov/pubmed/35654916?tool=bestpractice.com
Patients may present with dysphagia, heartburn, chest pain, acute food impaction, and/or associated other symptoms consistent with gastro-oesophageal reflux.[42]Chen JW, Kao JY. Eosinophilic esophagitis: update on management and controversies. BMJ. 2017 Nov 13;359:j4482.
http://www.ncbi.nlm.nih.gov/pubmed/29133286?tool=bestpractice.com
OGD can show multiple oesophageal rings with narrowing and decreased distensibility of oesophageal lumen from submucosal fibrosis and remodelling, oedema, exudates, linear furrows, and strictures, or the oesophagus may appear normal.[9]Reddy CA, McGowan E, Yadlapati R, et al. AGA clinical practice update on esophageal dysfunction due to disordered immunity and infection: expert review. Clin Gastroenterol Hepatol. 2024 Dec;22(12):2378-87.
https://www.cghjournal.org/action/showPdf
http://www.ncbi.nlm.nih.gov/pubmed/39436337?tool=bestpractice.com
[42]Chen JW, Kao JY. Eosinophilic esophagitis: update on management and controversies. BMJ. 2017 Nov 13;359:j4482.
http://www.ncbi.nlm.nih.gov/pubmed/29133286?tool=bestpractice.com
Diagnosis is confirmed with biopsy of the oesophageal mucosa during endoscopy.[43]Dhar A, Haboubi HN, Attwood SE, et al. British Society of Gastroenterology (BSG) and British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN) joint consensus guidelines on the diagnosis and management of eosinophilic oesophagitis in children and adults. Gut. 2022 Aug;71(8):1459-87.
https://gut.bmj.com/content/71/8/1459
http://www.ncbi.nlm.nih.gov/pubmed/35606089?tool=bestpractice.com
[48]Roman S, Savarino E, Savarino V, et al. Eosinophilic oesophagitis: from physiopathology to treatment. Dig Liver Dis. 2013 Nov;45(11):871-8.
http://www.sciencedirect.com/science/article/pii/S159086581300090X
http://www.ncbi.nlm.nih.gov/pubmed/23545170?tool=bestpractice.com
[49]Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. 2013 May;108(5):679-92.
http://www.ncbi.nlm.nih.gov/pubmed/23567357?tool=bestpractice.com
[50]Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011 Jul;128(1):3-20.e6; quiz 21-2.
https://www.jacionline.org/article/S0091-6749(11)00373-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/21477849?tool=bestpractice.com
[51]Lucendo AJ, Molina-Infante J, Arias Á, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J. 2017 Apr;5(3):335-58.
https://onlinelibrary.wiley.com/doi/10.1177/2050640616689525
http://www.ncbi.nlm.nih.gov/pubmed/28507746?tool=bestpractice.com
In the US, at least 2-4 biopsies are taken; at least 6 biopsies are recommended in Europe.[43]Dhar A, Haboubi HN, Attwood SE, et al. British Society of Gastroenterology (BSG) and British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN) joint consensus guidelines on the diagnosis and management of eosinophilic oesophagitis in children and adults. Gut. 2022 Aug;71(8):1459-87.
https://gut.bmj.com/content/71/8/1459
http://www.ncbi.nlm.nih.gov/pubmed/35606089?tool=bestpractice.com
[50]Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011 Jul;128(1):3-20.e6; quiz 21-2.
https://www.jacionline.org/article/S0091-6749(11)00373-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/21477849?tool=bestpractice.com
[51]Lucendo AJ, Molina-Infante J, Arias Á, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J. 2017 Apr;5(3):335-58.
https://onlinelibrary.wiley.com/doi/10.1177/2050640616689525
http://www.ncbi.nlm.nih.gov/pubmed/28507746?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].

 [Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].