Although the causes are numerous, a thorough history and physical examination helps elucidate the diagnosis in most patients.
History
The primary purpose of the initial encounter is to evaluate whether the symptoms suggest a more serious underlying condition.[5]Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018 Nov;27(11):2791-2803.
https://www.doi.org/10.1007/s00586-018-5673-2
http://www.ncbi.nlm.nih.gov/pubmed/29971708?tool=bestpractice.com
Musculoskeletal lower back pain can be diagnosed clinically from the history and physical examination. It is an exclusion diagnosis, therefore the clinician must eliminate specific lower back pain causes of neurological compromise, neoplasia, inflammatory arthritis, fracture, or referred pain from other locations or organ systems.
Red flags
Red flag signs and symptoms warranting additional diagnostic imaging and emergency referral to a spine specialist for ongoing management may include:[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
[30]Ramírez N, Olivella G, Valentín P, et al. Are constant pain, night pain, or abnormal neurological examination adequate predictors of the presence of a significant pathology associated with pediatric back pain? J Pediatr Orthop. 2019 Jul;39(6):e478-e481.
https://www.doi.org/10.1097/BPO.0000000000001353
http://www.ncbi.nlm.nih.gov/pubmed/30817418?tool=bestpractice.com
[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
[32]American College of Radiology. ACR appropriateness criteria: suspected retroperitoneal bleed. 2021 [internet publication].
https://acsearch.acr.org/docs/3158181/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794602?tool=bestpractice.com
[33]Henschke N, Maher CG, Refshauge KM. A systematic review identifies five "red flags" to screen for vertebral fracture in patients with low back pain. J Clin Epidemiol. 2008 Feb;61(2):110-18.
http://www.ncbi.nlm.nih.gov/pubmed/18177783?tool=bestpractice.com
[34]Han CS, Hancock MJ, Downie A, et al. Red flags to screen for vertebral fracture in people presenting with low back pain. Cochrane Database Syst Rev. 2023 Aug 24;8(8):CD014461.
http://www.ncbi.nlm.nih.gov/pubmed/37615643?tool=bestpractice.com
[35]Rossiter DJ, Haider Z, David B, et al. How not to miss major spinal pathology in patients with back pain. Br J Hosp Med (Lond). 2017 May 2;78(5):C66-9.
http://www.ncbi.nlm.nih.gov/pubmed/28489442?tool=bestpractice.com
Saddle anaesthesia
Sphincter disturbance (bladder or bowel dysfunction e.g. acute urinary retention, new onset urinary or faecal incontinence, loss of anal sphincter tone)
Profound or progressive neurological deficit
History of malignancy with new onset back pain
Systemic ailments, including fever, chills, night sweats, and/or unexplained weight loss
Intravenous drug use
Urinary tract infection
Immunosuppression, including prolonged corticosteroid use or other immunosuppressive therapies
Trauma (including minor trauma in older adults)
Presence of contusion or abrasions over the spine
History of osteoporosis
Pain that is refractory to conservative management
Thoracic pain
Non-mechanical pain (i.e., systemic or referred causes of pain). Pain at rest and at night suggests a non-mechanical cause
Age >50 years
Red flag signs and symptoms vary between guidelines.[37]Parreira PCS, Maher CG, Traeger AC, et al. Evaluation of guideline-endorsed red flags to screen for fracture in patients presenting with low back pain. Br J Sports Med. 2019 May;53(10):648-654.
https://www.doi.org/10.1136/bjsports-2018-099525
http://www.ncbi.nlm.nih.gov/pubmed/30337350?tool=bestpractice.com
Most guidelines endorse the red flags of history of malignancy, unexpected weight loss, significant trauma, prolonged corticosteroid use, fever and HIV.[5]Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018 Nov;27(11):2791-2803.
https://www.doi.org/10.1007/s00586-018-5673-2
http://www.ncbi.nlm.nih.gov/pubmed/29971708?tool=bestpractice.com
Patients should be questioned regarding prior back pain episodes and treatments, onset, duration, location, radiation, character, aggravating and relieving factors, and severity. Musculoskeletal lower back pain may be dull, gnawing, tearing, burning, electric and/or associated with muscle spasms. Associated sciatica (radicular pain in the distribution of the sciatic nerve) usually presents as unilateral pain radiating from the buttock to below the knee.[53]Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015 Mar 26;372(13):1240-8.
https://www.doi.org/10.1056/NEJMra1410151
http://www.ncbi.nlm.nih.gov/pubmed/25806916?tool=bestpractice.com
Sciatic pain often has aching and sharp qualities and the patient may report associated weakness, numbness or paresthesia.[54]Jensen RK, Kongsted A, Kjaer P, et al. Diagnosis and treatment of sciatica. BMJ. 2019 Nov 19;367:l6273.
https://www.doi.org/10.1136/bmj.l6273
http://www.ncbi.nlm.nih.gov/pubmed/31744805?tool=bestpractice.com
Pain from spinal stenosis is typically worse with standing and lumbar extension and is relieved by sitting or forward flexion. Postural changes trigger neurogenic claudication, with symptoms of pain, weakness, numbness or tingling in the lower back, legs and buttocks.[19]Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234.
https://www.doi.org/10.1136/bmj.h6234
http://www.ncbi.nlm.nih.gov/pubmed/26727925?tool=bestpractice.com
Further inquiry into functional, occupational, social, and psychiatric history should be sought to address risk factors, including obesity, occupational risks, smoking, and psychosocial stressors.[55]Parreira P, Maher CG, Steffens D, et al. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018 Sep;18(9):1715-21.
http://www.ncbi.nlm.nih.gov/pubmed/29792997?tool=bestpractice.com
Maladaptive pain coping behaviours, nonorganic signs, functional impairment, poor general health status, and psychiatric comorbidities are risk factors for developing chronic disabling low back pain.[9]Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010 Apr 7;303(13):1295-302.
http://www.ncbi.nlm.nih.gov/pubmed/20371789?tool=bestpractice.com
Symptoms of severe compression of the cauda equina or spinal cord
Bowel or bladder dysfunction, bilateral sciatica, and saddle anaesthesia may be symptoms of severe compression of the cauda equina. The aetiology is usually a large central herniated disc or a pathologic or traumatic fracture. Acute spinal cord compression may present with sensory symptoms of altered sensation below a certain level or hemisensory loss; motor symptoms of hemiplegia/hemiparesis, paraplegia/paraparesis or tetraplegia/tetraparesis; and/or autonomic symptoms including constipation and urinary retention. The etiology may be spine trauma, vertebral compression fracture, intervertebral disc herniation, primary or metastatic spinal tumour, or infection.
A complete history and physical examination should identify impending neurological compromise and the need for emergency referral to a spinal surgeon.
Infections
Important infections to consider are spinal epidural abscess, osteomyelitis of the spine and discitis. Spinal epidural abscess can present with fever, back or neck pain, and neurological deficits. However, this triad of symptoms is only present in 10% to 15% of cases and therefore having a low threshold for considering this diagnosis in patients at risk is crucial.[27]Alerhand S, Wood S, Long B, et al. The time-sensitive challenge of diagnosing spinal epidural abscess in the emergency department. Intern Emerg Med. 2017 Dec;12(8):1179-83.
http://www.ncbi.nlm.nih.gov/pubmed/28779448?tool=bestpractice.com
Risk factors for epidural abscess include diabetes mellitus, intravenous drug use, an immunocompromised state, recent spinal surgery or trauma, presence of indwelling spinal catheter, pre-existing infection (in contiguous tissue or distant infection causing bacteremia), dialysis and alcohol misuse.[27]Alerhand S, Wood S, Long B, et al. The time-sensitive challenge of diagnosing spinal epidural abscess in the emergency department. Intern Emerg Med. 2017 Dec;12(8):1179-83.
http://www.ncbi.nlm.nih.gov/pubmed/28779448?tool=bestpractice.com
Osteomyelitis and discitis of the lumbar vertebrae can present with low back pain and a low grade fever.[56]Mylona E, Samarkos M, Kakalou E, et al. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009 Aug;39(1):10-7.
https://www.doi.org/10.1016/j.semarthrit.2008.03.002
http://www.ncbi.nlm.nih.gov/pubmed/18550153?tool=bestpractice.com
It may be associated with intravenous drug use, lower extremity and hip infections, and tuberculosis, due to the anatomy of the Batson venous plexus.[57]Ursprung WM, Kettner NW, Boesch R. Vertebral osteomyelitis: a case report of a patient presenting with acute low back pain. J Manipulative Physiol Ther. 2005 Nov-Dec;28(9):713-8.
http://www.ncbi.nlm.nih.gov/pubmed/16326242?tool=bestpractice.com
[58]Eren Gök S, Kaptanoğlu E, Celikbaş A, et al. Vertebral osteomyelitis: clinical features and diagnosis. Clin Microbiol Infect. 2014 Oct;20(10):1055-60.
https://www.doi.org/10.1111/1469-0691.12653
http://www.ncbi.nlm.nih.gov/pubmed/24766063?tool=bestpractice.com
It is important to consider vertebral osteomyelitis and discitis in older adults with back pain and urinary tract symptoms as the urinary tract may be a source of infection from gram-negative organisms.[56]Mylona E, Samarkos M, Kakalou E, et al. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009 Aug;39(1):10-7.
https://www.doi.org/10.1016/j.semarthrit.2008.03.002
http://www.ncbi.nlm.nih.gov/pubmed/18550153?tool=bestpractice.com
Herpes zoster (shingles) affecting a truncal dermatome may present with back pain. There is typically a prodrome of burning, stinging or stabbing pain, followed by a vesicular rash which does not cross the midline.
Spinal metastasis
Metastasis to the spine needs to be excluded, especially in patients with a current diagnosis of cancer, a history of cancer, or suspected cancer.[39]National Institute for Health and Care Excellence. Spinal metastases and metastatic spinal cord compression. Sep 2023 [internet publication].
https://www.nice.org.uk/guidance/ng234
Breast, prostate, and lung cancer are responsible for more than 80% of cases of metastatic bone disease and the spine is the most common site of bone metastasis.[59]Maccauro G, Spinelli MS, Mauro S, et al. Physiopathology of spine metastasis. Int J Surg Oncol. 2011 Aug 10 [Epub ahead of print].
https://www.doi.org/10.1155/2011/107969
http://www.ncbi.nlm.nih.gov/pubmed/22312491?tool=bestpractice.com
Spinal compression fractures
Should be considered in patients who are at risk of osteoporotic disease. Older people and those on long-term corticosteroid therapy are particularly at risk.
Many osteoporotic spinal compression fractures are asymptomatic with no recognised trauma and are identified incidentally on x-ray while investigating other pathologies. However, some patients can present with acute onset back pain from minor trauma such as coughing or sneezing. The pain often disturbs sleep, is aggravated by movement and can radiate bilaterally to the abdomen.
Inflammatory spondyloarthropathy
Back pain due to inflammatory spondyloarthropathy more commonly starts before the age of 35 years. There may be a family history of psoriasis or spondyloarthritis, or a history of recent genitourinary infection. Other features suggesting spondyloarthritis include waking due to pain in the second half of the night, buttock pain, improvement with movement and improvement within 48 hours of taking nonsteroidal anti-inflammatory drugs.[28]National Institute for Health and Care Excellence. Spondyloarthritis in over 16s: diagnosis and management. Jun 2017 [internet publication].
https://www.nice.org.uk/guidance/NG65
Musculoskeletal symptoms apart from chronic back pain include dactylitis and enthesitis. Extra-articular symptoms include uveitis and psoriasis (including psoriatic nail symptoms).
It is important to be aware that the diagnosis of spondyloarthritis is sometimes missed or delayed.[28]National Institute for Health and Care Excellence. Spondyloarthritis in over 16s: diagnosis and management. Jun 2017 [internet publication].
https://www.nice.org.uk/guidance/NG65
Prompt referral to a rheumatologist is therefore essential for further diagnostic tests and appropriate management.
Non-specific causes of back pain
It is important to identify any less serious or non-specific causes of back pain to ensure appropriate management and maximum quality of life for these patients. While a specific cause of low back pain can rarely be identified, the most prevalent type is mechanical non-specific low back pain (exacerbated by movement and relieved by rest).[6]Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb 1;344(5):363-70.
http://www.ncbi.nlm.nih.gov/pubmed/11172169?tool=bestpractice.com
[60]Gianola S, Bargeri S, Del Castillo G, et al. Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Br J Sports Med. 2022 Jan;56(1):41-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8685632
http://www.ncbi.nlm.nih.gov/pubmed/33849907?tool=bestpractice.com
Risk stratification tools can be used (e.g., the STarT Back risk assessment tool) at first point of contact for each new episode of low back pain, with or without sciatica, to inform shared decision-making about stratified management.[7]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].
https://www.nice.org.uk/guidance/ng59
Physical examination
Perform a focused musculoskeletal and neurological examination.
Inspection
Looking for obvious deformity (e.g., in fractures) and abnormal curvature (scoliosis, kyphosis, lordosis), which can create pain in a minority of cases. This should prompt the clinician to order x-rays to document baseline curvature and orthopaedic referral for moderate to severe cases. Patients with spondylolisthesis may have an exaggerated lordosis and heart-shaped buttock.
Palpation
Palpation of the spinous processes and musculature: to localise any tenderness and to detect the presence of a midline 'step-off' of the spinous processes that may indicate spondylolisthesis.[61]Grødahl LH, Fawcett L, Nazareth M, et al. Diagnostic utility of patient history and physical examination data to detect spondylolysis and spondylolisthesis in athletes with low back pain: a systematic review. Man Ther. 2016 Aug;24:7-17.
http://www.ncbi.nlm.nih.gov/pubmed/27317501?tool=bestpractice.com
Tenderness on palpation over the sacroiliac joint may indicate sacroiliitis. Localised tenderness, present particularly with percussion, can indicate vertebral discitis or osteomyelitis.
Movement
Active and passive range of motion (ROM) assessment:[62]Alqarni AM, Schneiders AG, Hendrick PA. Clinical tests to diagnose lumbar segmental instability: a systematic review. J Orthop Sports Phys Ther. 2011 Mar;41(3):130-40.
http://www.jospt.org/doi/full/10.2519/jospt.2011.3457#.VAB3QfldXY8
http://www.ncbi.nlm.nih.gov/pubmed/21289452?tool=bestpractice.com
patients are asked in standing position to actively flex, extend, and laterally bend as far as they can. Pain on flexion that radiates to the leg suggests disc herniation with impingement on a nerve root; pain on extension can suggest either facet arthropathy or spinal stenosis. Greatly restricted ROM in a younger patient may suggest ankylosing spondylitis. Normal values for ROM vary between studies and decline in older age.[63]Troke M, Moore AP, Maillardet FJ, et al. A new, comprehensive normative database of lumbar spine ranges of motion. Clin Rehabil. 2001 Aug;15(4):371-9.
https://www.doi.org/10.1191/026921501678310171
http://www.ncbi.nlm.nih.gov/pubmed/11518438?tool=bestpractice.com
One study of asymptomatic subjects investigated the ROM of the lumbar spine during 15 activities of daily living. The median ROM used was 9 degrees for flexion/extension, 6 degrees for lateral bending and 5 degrees for rotation.[64]Bible JE, Biswas D, Miller CP, et al. Normal functional range of motion of the lumbar spine during 15 activities of daily living. J Spinal Disord Tech. 2010 Apr;23(2):106-12.
https://www.doi.org/10.1097/BSD.0b013e3181981823
http://www.ncbi.nlm.nih.gov/pubmed/20065869?tool=bestpractice.com
Every patient with lower back pain should have a hip examination. The distribution of pain from hip disorders is similar to the distribution of pain from lumbar spine disorders.[65]Prather H, Cheng A, Steger-May K, et al. Hip and lumbar spine physical examination findings in people presenting with low back pain, with or without lower extremity pain. J Orthop Sports Phys Ther. 2017 Mar;47(3):163-172.
https://www.doi.org/10.2519/jospt.2017.6567
http://www.ncbi.nlm.nih.gov/pubmed/28158964?tool=bestpractice.com
Hip and spine disorders may also coexist. Passive ROM of each hip should be assessed with the patient lying supine. There should be normally 130° of flexion, extension to 15° beyond neutral, and approximately 45° of internal and external rotation.[66]Soucie JM, Wang C, Forsyth A, et al. Range of motion measurements: reference values and a database for comparison studies. Haemophilia. 2011 May;17(3):500-7.
https://www.doi.org/10.1111/j.1365-2516.2010.02399.x
http://www.ncbi.nlm.nih.gov/pubmed/21070485?tool=bestpractice.com
Pain in any of these motions suggests hip pathology and hip x-rays should be obtained.
Patient gait and ability to walk should also be observed.
Provocative tests
May be performed for lumbar disk herniation, sacroiliac joint pain, and spondylosis.
Provocative testing for for lumbar disk herniation
Straight-leg raise or contralateral straight-leg raise test: when positive, indicates a possible herniated nucleus pulposus (HNP). A straight-leg raise is performed with the patient supine and the hip flexed gradually with the knee extended. Pain that is reproduced below 60° of hip flexion on the ipsilateral side is considered a positive straight-leg raise and is more sensitive. Reproduced pain on the contralateral side indicates a positive contralateral straight-leg raise and is more specific. Pain that occurs above 60° is usually secondary to hamstring tightness.[67]Deville WL, van der Windt DA, Dzaferagic A, et al. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine. 2000 May 1;25(9):1140-7.
http://www.ncbi.nlm.nih.gov/pubmed/10788860?tool=bestpractice.com
[68]Rubinstein SM, van Tulder M. A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract Res Clin Rheumatol. 2008 Jun;22(3):471-82.
http://www.ncbi.nlm.nih.gov/pubmed/18519100?tool=bestpractice.com
[69]van der Windt DA, Simons E, Riphagen II, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010 Feb 17;(2):CD007431.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007431.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/20166095?tool=bestpractice.com
The pain associated with HNP is usually worse in the leg than in the back, with pain radiating to the lower extremity in a dermatomal distribution. However, the absence of a positive straight-leg raise test and dermatomal pain does not exclude disk herniation.[70]Al Nezari NH, Schneiders AG, Hendrick PA. Neurological examination of the peripheral nervous system to diagnose lumbar spinal disc herniation with suspected radiculopathy: a systematic review and meta-analysis. Spine J. 2013 Jun;13(6):657-74.
http://www.ncbi.nlm.nih.gov/pubmed/23499340?tool=bestpractice.com
Femoral stretch or contralateral femoral stretch tests: can be used to assess for upper lumbar disk herniation. The test is typically performed with the patient prone. The knee is flexed, and then the leg is extended. If it reproduces the leg pain, it is considered positive.[71]Estridge MN, Rouhe SA, Johnson NG. The femoral stretching test. A valuable sign in diagnosing upper lumbar disc herniations. J Neurosurg. 1982 Dec;57(6):813-7.
http://www.ncbi.nlm.nih.gov/pubmed/7143064?tool=bestpractice.com
Provocative tests for sacroiliac joint (SIJ) pain
Several tests exist to evaluate the SIJ. Three or more positive tests indicate that the SIJ is likely to be the pain generator.[72]van der Wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006 Jan;87(1):10-4.
https://www.doi.org/10.1016/j.apmr.2005.09.023
http://www.ncbi.nlm.nih.gov/pubmed/16401431?tool=bestpractice.com
[73]Laslett M, Aprill CN, McDonald B, et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005 Aug;10(3):207-18.
https://www.doi.org/10.1016/j.math.2005.01.003
http://www.ncbi.nlm.nih.gov/pubmed/16038856?tool=bestpractice.com
[74]Kokmeyer DJ, Van der Wurff P, Aufdemkampe G, et al. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther. 2002 Jan;25(1):42-8.
https://www.doi.org/10.1067/mmt.2002.120418
http://www.ncbi.nlm.nih.gov/pubmed/11898017?tool=bestpractice.com
Thigh thrust test: the most sensitive test (sensitivity 88%).[73]Laslett M, Aprill CN, McDonald B, et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005 Aug;10(3):207-18.
https://www.doi.org/10.1016/j.math.2005.01.003
http://www.ncbi.nlm.nih.gov/pubmed/16038856?tool=bestpractice.com
The patient lies supine with the contralateral leg extended. The examiner flexes the ipsilateral hip to 50 degrees and the knee remains relaxed. The examiner encloses the knee and slightly adducts the femur, then applies a graded force through the long axis of the femur.[74]Kokmeyer DJ, Van der Wurff P, Aufdemkampe G, et al. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther. 2002 Jan;25(1):42-8.
https://www.doi.org/10.1067/mmt.2002.120418
http://www.ncbi.nlm.nih.gov/pubmed/11898017?tool=bestpractice.com
Distraction test: the most specific (specificity 81%).[73]Laslett M, Aprill CN, McDonald B, et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005 Aug;10(3):207-18.
https://www.doi.org/10.1016/j.math.2005.01.003
http://www.ncbi.nlm.nih.gov/pubmed/16038856?tool=bestpractice.com
With the patient lying supine, the examiner applies dorsal and lateral pressure to the anterior superior iliac spines.[74]Kokmeyer DJ, Van der Wurff P, Aufdemkampe G, et al. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther. 2002 Jan;25(1):42-8.
https://www.doi.org/10.1067/mmt.2002.120418
http://www.ncbi.nlm.nih.gov/pubmed/11898017?tool=bestpractice.com
Gaenslen’s test: performed by asking the patient to lie supine with the symptomatic leg hanging over the edge of the examination table. The nonsymptomatic leg is flexed at the hip and knee. A rotational force is then applied across the sacroiliac joint by applying pressure to the flexed knee outwards, while simultaneously applying pressure downwards on the affected sacroiliac joint with the other hand.
Pelvic compression test: performed by applying compression across the sacroiliac joints while the patient lies on their side.
FABER test: performed by asking the patient to bend their knee on the affected side and externally rotate at the hip, resting the foot across the opposite knee, so creating the shape of the number 4 with the legs. Pressure is then applied downwards on the knee on the affected side, while simultaneously using the other hand to apply pressure downwards on the opposite iliac crest.
Provocative test for spondylosis
The one-legged hyperextension test can be performed if the diagnosis of active spondylosis is suspected, but is not sufficiently sensitive to exclude the diagnosis.[75]Masci L, Pike J, Malara F, et al. Use of the one‐legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006 Nov;40(11):940-6.
http://www.ncbi.nlm.nih.gov/pubmed/16980534?tool=bestpractice.com
The patient stands on the affected leg and lifts the unaffected leg, slightly flexing the hip and flexing the knee to 80 degrees. The patient then actively extends their lumbar spine. The test is positive if this action reproduces their pain.[75]Masci L, Pike J, Malara F, et al. Use of the one‐legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006 Nov;40(11):940-6.
http://www.ncbi.nlm.nih.gov/pubmed/16980534?tool=bestpractice.com
Neurological examination
Specific neurological deficits, such as weakness, spasticity, or hyper/hyporeflexia, should be noted. These suggest more profound neurological compression; prompt referral to a spinal surgeon is indicated for further evaluation and management.[33]Henschke N, Maher CG, Refshauge KM. A systematic review identifies five "red flags" to screen for vertebral fracture in patients with low back pain. J Clin Epidemiol. 2008 Feb;61(2):110-18.
http://www.ncbi.nlm.nih.gov/pubmed/18177783?tool=bestpractice.com
Decreased rectal tone is an important examination finding, as it suggests sacral root encroachment from significant intraspinal compression.[33]Henschke N, Maher CG, Refshauge KM. A systematic review identifies five "red flags" to screen for vertebral fracture in patients with low back pain. J Clin Epidemiol. 2008 Feb;61(2):110-18.
http://www.ncbi.nlm.nih.gov/pubmed/18177783?tool=bestpractice.com
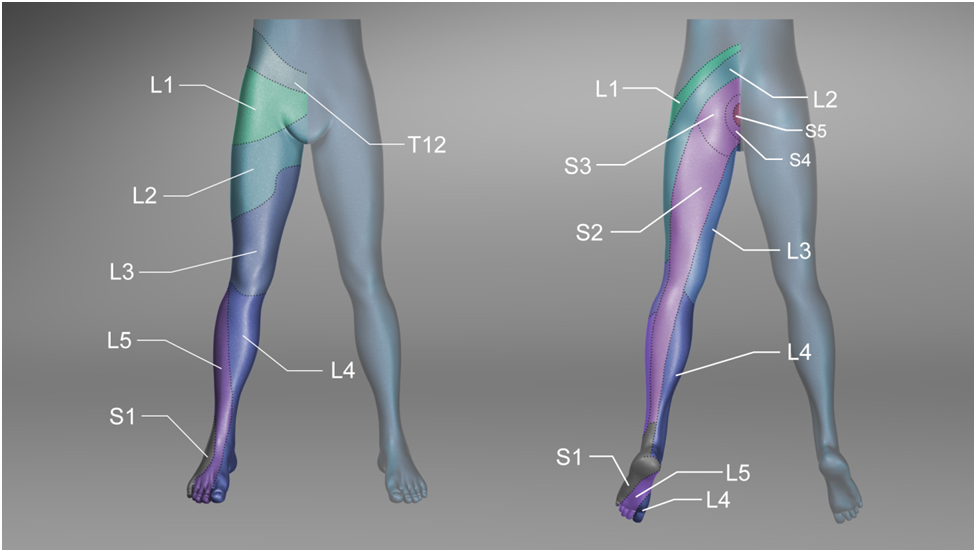
[Figure caption and citation for the preceding image starts]: Sensory dermatomes of the lower back and legCreated by BMJ Knowledge Centre [Citation ends].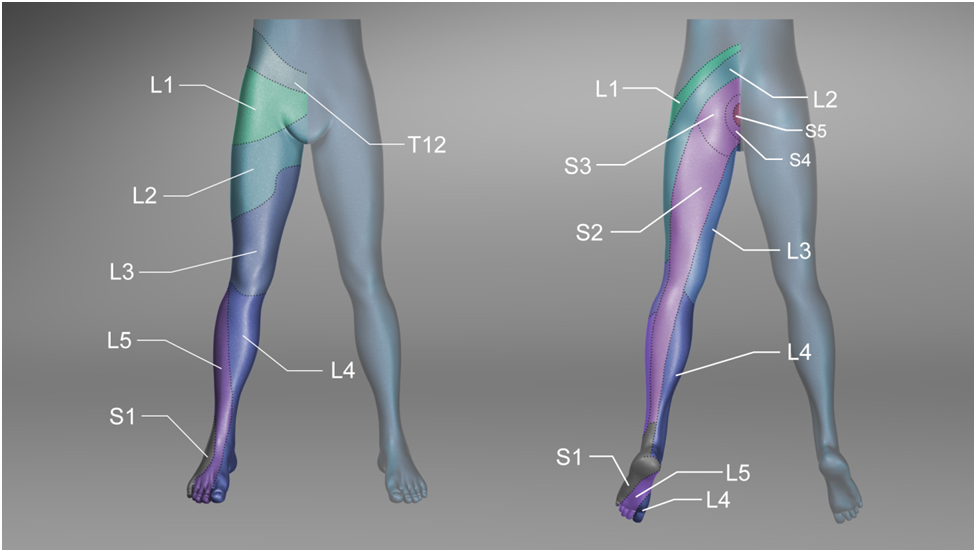
Vascular examination
Important in differentiating vascular versus neurogenic claudication. Vascular claudication typically worsens with ambulation in any position and is relieved immediately by rest. Neurogenic claudication worsens with ambulation in an extended posture and improves with forward flexion of the lumbar spine.[19]Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234.
https://www.doi.org/10.1136/bmj.h6234
http://www.ncbi.nlm.nih.gov/pubmed/26727925?tool=bestpractice.com
Patients with claudication may have concomitant vascular and spinal pathologies. Diminished pulses and mottled, thin, shiny skin are signs of peripheral arterial disease.
Other features that may aid diagnosis
A general physical examination may detect additional features that inform the diagnosis. For instance, presentations that may be associated with referred pain:
Aortic aneurysm (a detectable pulsatile abdominal mass)
Peptic ulcer (epigastric tenderness and melaena on rectal examination)
Renal colic or pyelonephritis (flank or costovertebral tenderness)
Pancreatitis (fever and tenderness/guarding of abdomen)
Herpes zoster (characteristic vesicular rash [shingles] in the affected dermatome).
Inspection of the backHow to perform an inspection examination of the back, including inspection of gait and posture
Laboratory tests
Routine laboratory studies are not necessary in the evaluation of back pain unless the physician is concerned about the possibility of malignancy, infection or inflammatory arthritis. In these cases full blood count (FBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are typically obtained. Blood cultures should be taken if infection is suspected.
FBC, ESR and CRP are normal in cases of mechanical back pain. Though non-specific, abnormal values may indicate malignancy, infection or inflammatory arthritis and should prompt further investigation of the cause of back pain.
A urinalysis and urine culture should be ordered when considering the possibility of pyelonephritis or renal colic.
Imaging
Most patients with low back pain, with or without sciatica, do not routinely require imaging when presenting in a non-specialist setting.[7]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].
https://www.nice.org.uk/guidance/ng59
[Evidence C]76fcb122-2d95-45cf-a51c-016101b66763guidelineCWhat are the effects of X-ray imaging or magnetic resonance imaging (MRI) compared with no investigation in people with low back and/or sciatica?[7]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].
https://www.nice.org.uk/guidance/ng59
If there are no red flags or high-risk features, they can be reassured that their symptoms will respond to conservative treatment.
If symptoms are progressive or persist longer than 6 weeks, imaging should be obtained if the result will change clinical management, for example if the patient is a candidate for surgery or intervention or if there is diagnostic uncertainty.[7]National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].
https://www.nice.org.uk/guidance/ng59
[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
Degenerative and disc abnormalities are found in many asymptomatic patients, causing over-diagnosis and unwarranted patient anxiety.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
[76]Rubinstein SM, van Tulder M. A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract Res Clin Rheumatol. 2008 Jun;22(3):471-82.
http://www.ncbi.nlm.nih.gov/pubmed/18519100?tool=bestpractice.com
[77]Chou R, Fu R, Carrino JA, et al. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009 Feb 7;373(9662):463-72.
http://www.ncbi.nlm.nih.gov/pubmed/19200918?tool=bestpractice.com
[78]Chou R, Qaseem A, Owens DK, et al. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011 Feb 1;154(3):181-9.
http://www.ncbi.nlm.nih.gov/pubmed/21282698?tool=bestpractice.com
[79]Weishaupt D, Zanetti M, Hodler J, et al. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998 Dec;209(3):661-6.
http://www.ncbi.nlm.nih.gov/pubmed/9844656?tool=bestpractice.com
[80]Stadnik TW, Lee RR, Coen HL, et al. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology. 1998 Jan;206(1):49-55.
http://www.ncbi.nlm.nih.gov/pubmed/9423651?tool=bestpractice.com
Degenerative findings do not necessarily equate to symptomatic lesions.[81]Tonosu J, Oka H, Higashikawa A, et al. The associations between magnetic resonance imaging findings and low back pain: a 10-year longitudinal analysis. PLoS One. 2017 Nov 15;12(11):e0188057.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5687715
http://www.ncbi.nlm.nih.gov/pubmed/29141001?tool=bestpractice.com
[82]Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Mar;72(3):403-8.
http://www.ncbi.nlm.nih.gov/pubmed/2312537?tool=bestpractice.com
Furthermore, there is no correlation between severity of symptoms and findings on MRI.[83]Burgstaller JM, Schüffler PJ, Buhmann JM, et al. Is there an association between pain and magnetic resonance imaging parameters in patients with lumbar spinal stenosis? Spine (Phila Pa 1976). 2016 Sep;41(17):E1053-62.
http://www.ncbi.nlm.nih.gov/pubmed/26953669?tool=bestpractice.com
Therefore, imaging studies should be ordered after discussion with a spinal surgeon or by the spinal surgeon in most cases to prevent ordering of unnecessary tests.
When imaging is indicated, magnetic resonance imaging (MRI) is usually the diagnostic modality of choice.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
Plain x-rays
May be indicated when there is a suspicion of a vertebral fracture: for example, in patients with low velocity trauma, especially minor trauma in older adults, and those with osteoporosis or chronic corticosteroid use.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
[84]Clark EM, Cummings SR, Schousboe JT. Spinal radiographs in those with back pain-when are they appropriate to diagnose vertebral fractures? Osteoporos Int. 2017 Aug;28(8):2293-7.
http://www.ncbi.nlm.nih.gov/pubmed/28444431?tool=bestpractice.com
Plain x-rays are performed in people with suspected sacroiliitis to rule out other causes of pain, but there are no pathognomonic findings specific to sacroiliac joint pain.[85]American College of Radiology. ACR appropriateness criteria: inflammatory back pain: known or suspected axial spondyloarthritis. 2021 [internet publication].
https://acsearch.acr.org/docs/3094107/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794593?tool=bestpractice.com
If plain x-rays are obtained following thoracolumbar spinal trauma, anteroposterior and lateral views are required. A 'swimmer’s lateral' view should be obtained if the shoulders obscure the upper thoracic spine.[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
However, computed tomography (CT) is the diagnostic modality of choice in these patients.[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
Magnetic resonance imaging (MRI)
Urgent MRI is indicated if neurological compromise is present, or if infection or tumour is suspected.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
[38]American College of Radiology. ACR appropriateness criteria: suspected spine infection. 2021 [internet publication].
https://acsearch.acr.org/docs/3148734/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794603?tool=bestpractice.com
[39]National Institute for Health and Care Excellence. Spinal metastases and metastatic spinal cord compression. Sep 2023 [internet publication].
https://www.nice.org.uk/guidance/ng234
If a patient has metal in their body or is unable to undergo an MRI, a CT myelogram is usually warranted.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
MRI scan of the sacroiliac joints is not generally required but is recommended when inflammatory spondylitis is suspected as the cause of back pain but the clinical examination and plain x-ray has not established the diagnosis.[85]American College of Radiology. ACR appropriateness criteria: inflammatory back pain: known or suspected axial spondyloarthritis. 2021 [internet publication].
https://acsearch.acr.org/docs/3094107/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794593?tool=bestpractice.com
MRI is sometimes used to diagnose spondylosis or spondylolisthesis.[86]Hansen BB, Nordberg CL, Hansen P, et al. Weight-bearing MRI of the lumbar spine: spinal stenosis and spondylolisthesis. Semin Musculoskelet Radiol. 2019 Dec;23(6):621-33.
https://www.doi.org/10.1055/s-0039-1697937
http://www.ncbi.nlm.nih.gov/pubmed/31745952?tool=bestpractice.com
Lumbar disc high intensity zones on MRI may be seen in patients with discogenic low back pain.[87]Yang L, Li W, Yang Y, et al. The correlation between the lumbar disc MRI high-intensity zone and discogenic low back pain: a systematic review and meta-analysis. J Orthop Surg Res. 2023 Oct 7;18(1):758.
https://josr-online.biomedcentral.com/articles/10.1186/s13018-023-04187-5
http://www.ncbi.nlm.nih.gov/pubmed/37805519?tool=bestpractice.com
However, the clinical significance of these findings is debated because high intensity zones in the lumbar spine have been reported in asymptomatic individuals.[88]Teraguchi M, Yim R, Cheung JP, et al. The association of high-intensity zones on MRI and low back pain: a systematic review. Scoliosis Spinal Disord. 2018;13:22.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6195950
http://www.ncbi.nlm.nih.gov/pubmed/30377668?tool=bestpractice.com
[89]Sima S, Chen X, Sheldrick K, et al. Reconsidering high intensity zones: its role in intervertebral disk degeneration and low back pain. Eur Spine J. 2024 Apr;33(4):1474-83.
https://link.springer.com/article/10.1007/s00586-024-08185-x
http://www.ncbi.nlm.nih.gov/pubmed/38381388?tool=bestpractice.com
Computed tomography (CT)
CT imaging of the thoracolumbar spine is the preferred test following spinal trauma for patients with midline tenderness, a high energy mechanism of injury, or those who are >60 years with a mechanism of injury consistent with thoracolumbar spine injury. CT may also be required in patients who cannot be examined due to intoxication, Glasgow Coma Score <15‚ or a distracting injury.[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
CT may also be indicated if spinal metastases or metastatic spinal cord compression is suspected, and MRI is contraindicated.[39]National Institute for Health and Care Excellence. Spinal metastases and metastatic spinal cord compression. Sep 2023 [internet publication].
https://www.nice.org.uk/guidance/ng234
Neurological compromise, gross spinal deformities or manual step off on spinal palpation also warrant CT. CT has a higher sensitivity for detecting fractures of the thoracolumbar spine than plain radiographs and also identifies soft tissue injuries that often accompany spinal fractures.[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
[40]Bailitz J, Starr F, Beecroft M, et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: a prospective comparison. J Trauma. 2009 Jun;66(6):1605-9.
https://www.doi.org/10.1097/TA.0b013e3181a5b0cc
http://www.ncbi.nlm.nih.gov/pubmed/19509621?tool=bestpractice.com
Up to 20% of patients with spinal injuries have a second, noncontiguous injury, therefore imaging of the entire spine is recommended.[31]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
Bone scintigraphy
Bone scintigraphy may be performed to detect vertebral compression fractures in patients with contraindications to magnetic resonance imaging.
Bone scintigraphy with single-photon emission CT (SPECT) or SPECT/CT is usually not used for initial imaging but can be useful for radiographically occult fractures and to evaluate acuity of vertebral fracture.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
It is also used to detect bone metastases.[29]American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].
https://acsearch.acr.org/docs/69483/Narrative
http://www.ncbi.nlm.nih.gov/pubmed/34794594?tool=bestpractice.com
Bone scintigraphy with single photon emission computed tomography is the gold standard for diagnosis of spondylolisthesis.[75]Masci L, Pike J, Malara F, et al. Use of the one‐legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006 Nov;40(11):940-6.
http://www.ncbi.nlm.nih.gov/pubmed/16980534?tool=bestpractice.com
Further investigations
Diagnosis of sacroiliitis as the cause of back pain is usually made by physical examination. However, further investigations include diagnostic local anaesthetic block injection of the sacroiliac joint under C-arm fluoroscopic guidance that, when positive, provides corresponding pain relief.[74]Kokmeyer DJ, Van der Wurff P, Aufdemkampe G, et al. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther. 2002 Jan;25(1):42-8.
https://www.doi.org/10.1067/mmt.2002.120418
http://www.ncbi.nlm.nih.gov/pubmed/11898017?tool=bestpractice.com
Other investigations, including laboratory, imaging, and endoscopic tests, are used when pain is suspected to be non-spine related (e.g., referred from intra/retroperitoneal pathologies). See Differential diagnosis.