Complications
A regular pattern of bowel movement every day or every other day is expected. Constipation is a common problem starting in the second year of life (a consequence of neurogenic bowel), and is treated with a high-fibre diet and hydration. Daily dosing with polyethylene glycol is often needed as well. Timed toileting is introduced when toddlers show an interest in toileting routines (parents are counselled to place their toddler on the commode for 10-15 minutes after meals in order to take advantage of the gastrocolic reflex). Spina Bifida Association bowel management guidelines recommend bowel continence. Independence with the bowel programme is less likely if not begun by pre-teen and early teen years.
A pattern of hard stools alternating with watery diarrhoea is suggestive of impaction and should be treated with enema clean-out. If rectal prolapse occurs, reduction is performed with gloved hand and lubricant.
Daily transanal irrigation programmes are effective and time efficient and can help children attain faecal continence at an early age, ideally by pre-school entry. Surgical treatment (posterior repair and suspension of the rectum) is rarely needed. Constipation may worsen with ageing, decreased fibre intake, and reduced activity. Fluids may need increasing. Spina Bifida Association: lifespan bowel management protocol Opens in new window
Faecal soiling is common (also a consequence of neurogenic bowel) and typically seen in children who have decreased rectal tone. This can result in significant skin breakdown, which is prevented with regular use of barrier creams. Occasionally, fibre laxatives can be helpful as bulking agents. Loperamide is not recommended. Daily transanal irrigation programmes are effective and time efficient and can help children attain faecal continence by pre-school entry. Surgical treatment options such as Malone antegrade colonic enema surgery should be discussed, but are typically performed when children are of school age and able to participate in decision making. Spina Bifida Association: lifespan bowel management protocol Opens in new window
May be a problem due to reduced mobility and lack of physical activity. Some studies have also shown that people with spina bifida have less lean body mass and a lower basal metabolic rate than the general population.
Prevention is more successful than trying to reduce weight. Therefore, a healthy diet and regular exercise should be encouraged from an early age. A single study of metformin for the treatment of central adiposity and the prevention of metabolic syndrome in children with spina bifida has documented success.[189]
All patients have tethering of the spinal cord (lower end of the spinal cord has abnormal attachment to other structures), but not all are symptomatic. Tethered cord rarely presents in early childhood. However, there have been case reports of early tethering (12 months) and epidermal inclusion cysts among infants who have had fetal surgery. Classic presentation is during the pre-adolescent growth spurt.
Signs and symptoms of tethered cord include back pain; rapidly progressive scoliosis; evolving cavovarus deformity; leg spasms; change in motor or sensory level; change in bowel, bladder, or sexual functioning; or if there are progressive symptoms associated with Chiari malformation (choking, gagging, new ophthalmoplegia or dysarthria, arching of neck, occipital notch tenderness, sleep apnoea).[190]
Caution is advised with making the diagnosis by x-ray appearance alone; therefore, MRI spine is indicated only if symptoms are present.[191] Findings include tethering or scarring of the cord, syrinx, a thickened filum terminale, and a low-lying conus (below L2-L3). The normal filum is 2 mm or less in diameter at L5-S1. Sagittal T1- or T2-weighted images readily show the level of the conus. [Figure caption and citation for the preceding image starts]: Spine MRI scan showing tethered cordFrom the collection of Dr Nienke P. Dosa; used with permission [Citation ends].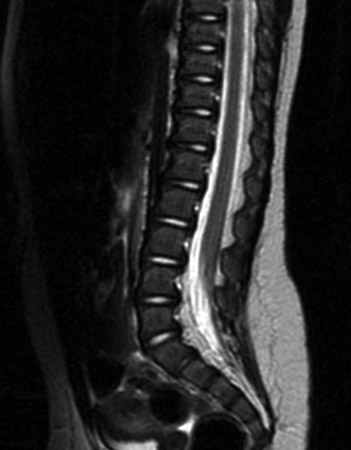
Treatment is surgical untethering of the cord, a procedure that is effective in improving back pain in 90% of patients and prevents further progression of other symptoms.[192]
In general, all women with spina bifida are fertile. However, perineal numbness and reduced lubrication can cause labial tears or friction injury. Erectile dysfunction and retrograde ejaculation are common in men with spina bifida. Treatments for erectile dysfunction include sildenafil, injectable papaverine, and others. Sympathomimetics such as pseudoephedrine can help reduce retrograde ejaculation if taken before intercourse.
Ischial ulcers suggest inadequate off-loading in a wheelchair. Sacral ulcers can occur postoperatively, and are due to inadequate off-loading on a mattress. Pressure sores in the feet are due to poorly fitted orthoses or poor ambulation technique such as single-arm crutch walking. Most often, decubitus ulcers are due to inadequate equipment.
Skin examination should be performed by both patient and physician, particularly at the cele repair site, coccygeal area, ischial tuberosities, feet, and ankles, and in between toes. Prompt identification of the underlying cause is essential.
Decubitus ulcers are quite common in young adults and should be treated aggressively.
Pressure sores are rare in infants, but friction or burn injuries can be a concern.
Poor nutrition and faecal and urinary incontinence can also contribute to wounds.
Pressure mapping of the seating device may help determine areas of pressure and facilitate correction for recurrent ischial pressure sores.
In addition to treating the underlying cause, the physician should carefully document the extent of the wound, and evaluate and treat signs and symptoms of infection with oral antibiotics if minor, and intravenous antibiotics if more severe. Chronic wounds should be evaluated with plain films and bone scan to rule out an underlying osteomyelitis. Negative pressure wound therapy is effective for stage 3 and stage 4 decubitus ulcers. Referral to a wound care centre for comprehensive follow-up and nutritional and psychological support is recommended if available.
Many adolescents and young adults become socially isolated. Participation in peer activities is less than in the general population due to a complex interplay of physical disability, incontinence, executive dysfunction, and non-verbal learning disability. Depression may be related to poor social integration and achievement.
Anxiety and depression are common, affecting 30% of adults (both young and old).[158]
Cardiovascular disease (CVD) risk may be increased due to higher incidence of metabolic syndrome and obesity. As the population ages, this may become a major concern. In one study, CVD was the second most frequent cause of death in adults with spina bifida.[193]
Regular preventative care, including healthy diet and activity level, with weight control should be encouraged. Smoking cessation therapy for those who smoke is needed.
May occur in adult patients. The cause is poorly understood, and few data exist on lymphoedema and spina bifida.[165] Treatment involves compressive stockings and manual or mechanical pump therapy. Prolonged lymphoedema left untreated can lead to cellulitis and increased risk of pressure sores, as well as osteomyelitis in the feet and legs.
Shunt obstruction is a relatively common complication, affecting 40% of paediatric patients. The risk of shunt obstruction or infection is greatest during the first 6-12 months after shunt placement.
Signs and symptoms include headache, vomiting, somnolence, personality change, rapid head growth, and seizures. Headaches related to shunt malfunction may be intermittent, as in the case of proximal valve obstruction, or worse, when the patient is supine, due to diminished gravity flow, or when proceeding from a supine to upright position due to over-drainage related to slit ventricle syndrome (when the ventricles are over-drained, and appear as slits on the scans).
It is essential to document a patient's baseline neurological examination with every clinical encounter. Any deterioration, such as new numbness, spasticity or weakness, academic difficulties, headache, or features of Chiari malformation such as ophthalmoplegia, sleep apnoea, arching of the neck, or dysphagia, should be evaluated promptly with a high index of suspicion for shunt malfunction.
A shunt series (plain x-rays that trace the shunt tubing from head to abdomen) is used to document broken or fractured tubing. Magnetic resonance imaging (MRI) or computed tomography (CT) head is indicated if there are signs or symptoms of shunt malfunction. However, up to 15% to 20% of patients with shunt malfunction have no change in ventricle size on MRI or CT scan.[86]
Shunt revision is the mainstay of treatment.
Patients with shunted hydrocephalus are more likely to have learning disabilities.
Non-verbal learning disability is often diagnosed at school when mathematics and abstract reasoning are introduced. It is also characterised by difficulties in visual spatial tasks (e.g., understanding directions). Reading comprehension, which is increasingly important to academic performance in other subjects, can also be a challenge as children transition from learning to read to reading to learn. Families and school personnel should be made aware of teaching strategies and adaptations for non-verbal learning disability. Individualised education plans should focus on the learning disability rather than the motor impairment so that appropriate educational supports are put into place.
Executive dysfunction is very common and classically presents with 'cocktail party' speech and disinhibition. Children and adults with executive dysfunction may also have difficulties with novel situations, setting priorities, and taking initiative. The key to fostering independence is repetition of essential tasks and self-care skills so that these become rote activities.
Many young adults with spina bifida leave school with educational qualifications. Yet employment rates and other social outcomes in young adulthood are sub-optimal. This is in part due to unmasking of non-verbal learning disability and executive dysfunction when the structure of school routines is no longer available. Studies have also shown that teenagers with spina bifida do not engage in the same activities as non-disabled peers during the high school years. It is therefore essential to promote participation from an early age, and also to discuss from an early age the impact that executive dysfunction can have on independent living and employment, unless adaptations are made proactively and appropriate support systems such as vocational training are utilised before high school graduation.
Frequent urinary tract infections (UTIs) warrant a detailed review of the symptoms that prompted the diagnosis. Cloudy urine or a routine urine culture that was obtained when a patient is otherwise asymptomatic may not represent true infection. It is important to gather information about culture results and antibiotics used for treatment. Recurrent febrile UTIs with the same organism may indicate that a bladder stone is the nidus and warrant evaluation with renal/bladder ultrasound. Video-urodynamics is performed to determine whether alterations in bladder function (possibly related to tethered cord syndrome) is contributing to recurrent infection.
It is important to review whether the patient is observant of clean technique with intermittent catheterisation. Most children who perform intermittent catheterisation become colonised with bacteria. Asymptomatic bacteriuria is not treated (except in children in the first 2 months of life). Children with frequent symptomatic infections are placed on antibiotic prophylaxis. Symptomatic infections are treated with cephalexin, nitrofurantoin, or ciprofloxacin, based on culture results.
Back pain associated with fever, costovertebral angle tenderness, and general malaise is suggestive of pyelonephritis. Treatment involves oral or intravenous antibiotics, determined by severity of the clinical picture.
In a newborn or infant, video-urodynamics or a voiding cystourethrogram is obtained if hydronephrosis is noted on the renal ultrasound. These diagnostic studies determine whether there is vesicoureteral reflux and/or incomplete emptying. If reflux is documented, clean intermittent catheterisation and antibiotic prophylaxis is instituted to prevent kidney damage. However, if low voiding pressures are noted on urodynamic study, infants with vesicoureteral reflux can be managed with antibiotic prophylaxis only, and intermittent catheterisation is discontinued.
Hydronephrosis and vesicoureteral reflux are closely correlated with a high-risk bladder. Therefore, infants with findings on ultrasound suggestive of hydronephrosis are started on clean intermittent catheterisation every 4-6 hours using 5 French or 8 French latex-free catheters. Prophylactic antibiotics are added if there is reflux. Some centres place all newborns on intermittent catheterisation, oxybutynin, and antibiotic prophylaxis at birth.
Involves extension of the central canal with obstruction and cyst (cerebrospinal fluid collection) formation in the spinal cord, known as a syrinx.
Features of syringomyelia should be assessed at every visit. Signs of cervical level syrinx include shoulder numbness (cape distribution), hyperreflexia or asymmetry of the upper extremities, and progressive scoliosis. Hand weakness, ulnar nerve entrapment, or carpal tunnel syndrome may also be a sign of a cervical level syrinx.
Magnetic resonance imaging (MRI) of the cervicothoracic junction and of the entire spine is recommended to rule out syringomyelia.
Treatment is based on clinical symptoms rather than MRI findings, because syringomyelia is visible on MRI in 80% of children with myelomeningocele, but a clinical concern in only 2% to 5% of patients.[86]
The initial treatment approach is shunt revision, followed by decompression of the posterior fossa. There is controversy about syringopleural or syringoperitoneal shunting as a primary treatment. Most centres monitor the syrinx after decompression surgery, with an MRI study 3-6 months later. A syrinx shunt is placed only if the syrinx progresses during that time interval.
Rates of latex sensitisation among individuals with spina bifida have been ascertained by a variety of immunological testing strategies and range from 23% to 73%.[185] Latex allergy (symptoms include urticaria, conjunctivitis, angio-oedema, rhinitis, bronchial asthma, and anaphylaxis) develops in 8% to 72% of latex-sensitive individuals.[186][187] Multiple surgeries and a history of atopy are the most commonly identified risk factors. The risk of latex reaction also increases with age.[188]
All individuals with spina bifida should be considered at high risk for having an allergic reaction and should practise latex avoidance in healthcare settings, as well as at home and in the community.[163] Individuals who have had an allergic reaction to latex should be advised to wear a medical alert bracelet and be prescribed an auto-injectable adrenaline.
Spina Bifida Association: latex and latex allergy guideline Opens in new window
Approximately 30% of children with shunted hydrocephalus have attention deficits, which are marked by impairment in the ability to shift focus, rather than inattentiveness due to impulsivity or hyperactivity. Low-dose stimulants may have a modest benefit for some of these children.
With changes to the spinal curvature and loosening of ligaments, back pain, sciatica, and possibly tethered cord can occur.
Walking endurance may be affected due to weight gain in pregnancy.
As a result of increased intra-abdominal pressure from the growing uterus, there is a greater risk of ventriculoperitoneal shunt malfunction.
Intermittent catheterisation may need to be increased to accommodate for the pressure on the bladder as pregnancy progresses.
Worsening constipation may require a more aggressive bowel regimen, including enemas.
Weight gain and circulation changes may increase the risk of pressure sores; therefore, frequent pressure relief movement (re-adjust position) and close skin monitoring is required.
Use of this content is subject to our disclaimer