Approach
Most systemic disorders can be diagnosed with laboratory tests that assess neuroendocrine and ovarian function.[12]
The majority of structural abnormalities are identified through pelvic examination and imaging studies.[12]
History
Last spontaneous menstrual period, contraception used, and current pregnancy status should be determined for all patients.
The following features should be explored as part of the history:[9][17][19][22][23][24][25]
Hypoestrogenism: symptoms include hot flushes, sleep disturbance, irritability, reduced libido, and vaginal dryness
Cycle irregularity: may be associated with conditions resulting in amenorrhoea (e.g., polycystic ovary syndrome)
Dysmenorrhoea or painful cramps: may be due to endometriosis, or to an obstructed outflow tract resulting in hematocolpos
Traumatic head injury: can result in hypogonadism
Central nervous system infection: (e.g., encephalitis)
Headache or visual field changes: suggestive of a central nervous system tumour
Galactorrhea: suggests hyperprolactinaemia, which is commonly associated with secondary amenorrhoea
Poor nutritional status due to systemic illness, an eating disorder: may result in functional hypothalamic amenorrhoea. An inquiry into a patient's health status, eating habits, and body image is necessary
Emotional stress: can impair hypothalamic function, resulting in functional hypothalamic amenorrhoea
Extreme athleticism: may result in functional hypothalamic amenorrhoea, especially in patients with low BMI (10% less than ideal body weight)
Chronic systemic illness: may present with fatigue, malaise, or extreme weight loss, depending on the cause.
History of obstetric or surgical procedures should prompt consideration of intrauterine adhesions. Postpartum endometritis, dilation and curettage, or other intrauterine infection can result in Asherman's syndrome, the most severe form of intrauterine adhesions (obliterative endometrial process resulting in amenorrhoea).
Chemotherapy or pelvic radiotherapy may suggest premature ovarian insufficiency (POI).
A complete medication history is important. Oral contraceptives, long-acting progestogens, androgens, antipsychotic medications, and chronic opioid use can induce amenorrhoea.[20] The type of medication may help to identify a treated disorder that could be causing amenorrhoea.
A family history of cessation of menses before age 40 years may indicate POI.
Physical examination
The patient's weight and height should be measured. Low BMI (10% less than ideal body weight) may suggest an eating disorder or the athletic triad (amenorrhoea, osteoporosis, and disordered eating).[26]
Polycystic ovary syndrome (PCOS) is associated with obesity, although estimates of the prevalence of obesity in people with PCOS vary widely depending on factors such as geography, ethnicity, and culture.[27]
External and internal genitalia are usually normal.[1] Clitoromegaly suggests hyperandrogenaemia or adrenal insufficiency. A pelvic examination may show vaginal atrophy, which is common with long-standing oestrogen deficiency. The ovaries are usually non-palpable, however, they may be palpable in some patients with polycystic ovary syndrome or autoimmune oophoritis. The uterine cervix should be noted on examination. Internal examinations are not always possible, and the clinician may need to proceed with imaging options or an examination under anesthesia.
Assess visual fields if a pituitary tumour is suspected.
Generalised Tanner staging exam is required to evaluate for oestrogen effect. Even though this is most likely to be an issue for primary amenorrhoea, patients with gonadal dysgenesis may have findings that suggest a hypo-oestrogenic state.[Figure caption and citation for the preceding image starts]: Androgen-secreting tumour in cut section of right ovaryBMJ Case Reports 2009; doi:10.1136/bcr.11.2008.1286 [Citation ends].
Other findings suggestive of an underlying pathology
Hyperandrogenaemia: careful attention should be given to signs on initial examination, including male-pattern baldness, deepening of the voice, wide distribution of terminal hair (male pattern), increase in muscle bulk, breast atrophy, and clitoromegaly.[1] These patterns may vary based on ancestry. If symptoms are slowly progressive, polycystic ovary syndrome or non-classic congenital adrenal hyperplasia is possible. Acute and progressive symptoms may indicate that the patient has an androgen-producing tumour (ovarian or adrenal).
PCOS: skin examination may show acanthosis nigricans, acne, and hirsutism.[28]
Cushing syndrome: skin examination may show purple striae.[1] Other signs include central obesity, buffalo hump, easy bruising, proximal muscle weakness, and hypertension.[29]
Thyroid dysfunction: signs include goitre, exophthalmos, lid lag, abnormal heart rate, or skin changes.
Adrenal insufficiency (Addison's disease): signs include orthostatic hypotension, pigment changes, and decreased axillary or pubic hair.[30]
Laboratory tests
Urine or serum pregnancy: the first test performed in anyone of reproductive age presenting with secondary amenorrhoea.[1]
Follicle-stimulating hormone (FSH): after ruling out pregnancy, this is the next test ordered.[1] In combination with oestradiol levels, gonadotrophins help to determine if amenorrhoea is due to gonadal failure, hypothalamic dysfunction, or systemic or functional causes. FSH is more useful as a single test than luteinising hormone (LH). LH is not usually included in the initial investigations ordered.
Serum oestradiol: low levels are suggestive of either primary ovarian insufficiency (along with elevated FSH) or suppressed hypothalamic function (low FSH).
Serum prolactin: elevated levels of circulating prolactin (hyperprolactinaemia), whether idiopathic or due to a pituitary adenoma, result in hypogonadotrophic hypogonadism. For persistently elevated levels, neuroimaging is indicated to rule out intracranial neoplasm.[31]
Thyroid-stimulating hormone (TSH): indicated to rule out (primary) hypothyroidism. Mild or sub-clinical hypothyroidism probably will not result in menstrual irregularities.[12] It is proposed that elevated thyrotrophin-releasing hormone stimulates prolactin secretion from the pituitary, suppressing FSH production.[32] Suppressed TSH suggests hyperthyroidism, which may cause oligomenorrhoea.
Serum androgens: measured for signs of hyperandrogenism. Levels of androgens such as dehydroepiandrosterone sulphate and free testosterone are elevated in patients with polycystic ovary syndrome, but may be significantly higher in patients with androgen-producing tumours.[23]
A karyotype helps to confirm the aetiology of premature ovarian insufficiency in patients <30 years.[33]
Physiological tests and imaging
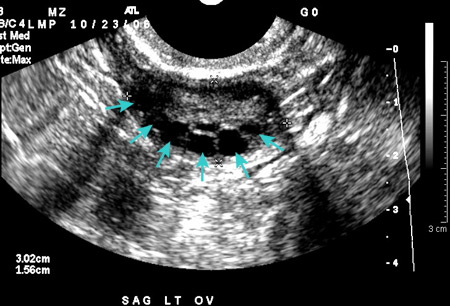
Transabdominal or transvaginal ultrasound: performed if a pelvic examination is not possible. Ultrasound confirms normal anatomy, aids in the diagnosis of most structural abnormalities, and may obviate the need for progestogen challenge. Transvaginal is the preferred modality, if possible, to evaluate endometrial thickness. In patients with low levels of estradiol, a thin endometrial echo (atrophy) would be characteristic on transvaginal ultrasound.[Figure caption and citation for the preceding image starts]: Polycystic ovarian ultrasoundFrom the collection of Dr M.O. Goodarzi; used with permission [Citation ends].
Progestogen challenge: can be used to evaluate the competence of a functional outflow tract exposed to normal levels of circulating oestrogen. Lack of a withdrawal bleed may occur in patients with premature ovarian insufficiency, hypothalamic dysfunction, Asherman's syndrome, or polycystic ovary syndrome (e.g., elevated androgen levels may induce endometrial atrophy), all of which require substantially different evaluations. If no withdrawal bleed is observed, administering oestrogen for 4 to 8 weeks, followed by a second progestin withdrawal challenge, can help to differentiate between structural and endocrinological causes. (Note that there are no clear recommendations as to length of exposure to low circulating levels of oestradiol; the length of time given here is a suggestion). Hormonal assays and ultrasound findings largely obviate the need for progestin challenge.[1]
Additional imaging studies
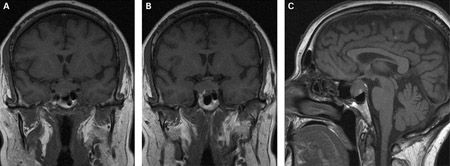
Magnetic resonance imaging (MRI) is the most effective tool for characterising specific structural abnormalities and may prevent the need for surgical diagnosis.
If prolactin levels are significantly elevated, cranial MRI is indicated to rule out pituitary adenoma.[1][31][Figure caption and citation for the preceding image starts]: (A) Coronal T1-weighted MRI scan showing a pituitary mass with expansion of the pituitary fossa (B) Coronal T1-weighted MRI scan showing a pituitary mass extending into the cavernous sinus, particularly on the right (C) Sagittal T1-weighted MRI scan of the pituitary tumourBMJ Case Reports 2009; doi:10.1136/bcr.08.2009.2193 [Citation ends].
 [Figure caption and citation for the preceding image starts]: T2-weighted axial MRI scan showing a lesion in the pituitary fossa (arrow), displaying heterogeneous signal intensity suggesting recent apoplexyBMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0902 [Citation ends].
[Figure caption and citation for the preceding image starts]: T2-weighted axial MRI scan showing a lesion in the pituitary fossa (arrow), displaying heterogeneous signal intensity suggesting recent apoplexyBMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0902 [Citation ends].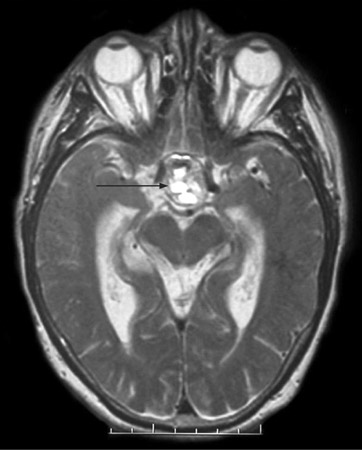
Bone density measurement may be indicated in selected patients such as those with chronic hypo-oestrogenaemia. This test may be less useful in younger patients who have not reached peak bone mass density (BMD). Use of steroidal contraceptives may also affect BMD.[34]
Asherman's syndrome can be diagnosed by transvaginal ultrasound (may lack typical trilaminar appearance of endometrial echo found during normal proliferative phase); however, sonohysterography or hysterosalpingography are typically the initial tests. Hysteroscopy remains the gold standard for diagnosis.[Figure caption and citation for the preceding image starts]: Lower uterine segment in patient with Asherman's syndrome, seen on hysterosalpingogramFrom the collection of Dr Meir Jonathon Solnik [Citation ends].

Other: leptin
Leptin, a cytokine secreted by adipocytes, the hypothalamus, and the pituitary gland, seems to have a significant impact on neuroendocrine and reproductive function as well as energy modulation. Serum leptin levels are affected by percentage of body fat, so women with eating disorders or poor nutritional status tend to have lower levels, representative of an alteration of the hypothalamic-pituitary-ovarian axis. Therefore, replacement of leptin restores ovulatory menstruation in women with hypothalamic amenorrhoea.[35][36]
Use of this content is subject to our disclaimer