Approach
Treatment of adhesive capsulitis requires a multi-faceted and individualised approach, depending on specific symptoms and their severity. A stepwise approach, beginning with non-invasive treatment, gives way to invasive interventions if early treatment options prove to be ineffective.
Activity modification
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may necessitate significant time off work or away from leisure activities.
Physiotherapy
Physiotherapy is the cornerstone of successful treatment, and should be initiated as early as possible in the disease course. A home exercise regimen, consisting of active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal.[38]
Data support the use of high-grade mobilisation techniques for improving mobility.[38][39] These include passive mobilisation techniques in end-range positions of the glenohumeral joint, versus low-grade mobilisation techniques that are passive mobilisation in the pain-free zone. Preliminary findings from a systematic review of 7 different mobilisation techniques have shown that the Maitland technique (a high-grade mobilisation technique) and combined mobilisations have beneficial effects. However, more research is needed to determine the most successful mobilisation technique.[40]
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear, and a systematic review showed no clear benefit to ultrasound therapy.[41]
A useful exercise that can be performed in the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it towards the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
Oral medical therapy
As the initial stages of adhesive capsulitis are associated with an inflammatory process, early in the disease course a scheduled regimen of oral non-steroidal anti-inflammatory drugs (NSAIDs) may provide symptomatic relief as well as decrease the severity of the disease. NSAIDs should be considered for all patients presenting with evidence of adhesive capsulitis, providing that there are no contraindications, and are regarded as the mainstay of treatment. Choices include ibuprofen, meloxicam, or naproxen.
There is some limited evidence that oral corticosteroids may offer early pain relief, but the benefits are short-term and may not last beyond 6 weeks.[42] Their use may be considered in the earlier phases of the disease during painful periods and flare-ups associated with decreased range of glenohumeral motion. One randomised controlled trial has shown, however, that intra-articular injection provides greater improvement in range of motion and patient satisfaction after 4 weeks, compared with oral corticosteroids.[43]
Several different oral corticosteroid regimens have been studied, with similar short-term results.[42][44][45] One type of regimen is methylprednisolone taken daily for 6 days. There is a theoretical risk of avascular bone necrosis with the use of oral corticosteroids.[46] However, this is an extremely rare event when prescribing oral corticosteroids for short-term use.
Corticosteroid injection
Provides a concentrated, local treatment of the inflammatory process involved in adhesive capsulitis. It also provides the added benefit of pain relief, especially with active and passive range of motion early in the disease course, which is invaluable for participation in physiotherapy.[43][47][48][49][50][51][52] It may therefore be considered for those patients who present with pain despite initial physiotherapy and use of NSAIDs.
One randomised controlled trial found that an intra-articular corticosteroid injection given prior to the start of a physiotherapy programme provided faster improvement in pain, range of motion, and function compared with oral NSAIDs and physiotherapy for up to 8 weeks after treatment. However, no significant difference was found at the final follow-up at 3 months. This finding is similar to previous studies; therefore, it is reasonable to consider offering a corticosteroid injection prior to the start of a physiotherapy programme in order to facilitate early, aggressive physiotherapy.[53][54]
One meta-analysis shows that multiple injections are beneficial for up to 16 weeks on average, with as many as three injections having a positive effect.[49]
The preferred technique is an intra-articular glenohumeral injection using triamcinolone acetonide administered together with a local anaesthetic (e.g., lidocaine without epinephrine [adrenaline]). Injections should primarily occur into the glenohumeral joint. However, there is some evidence that corticosteroid injection into the subacromial space can be equally beneficial when compared with intra-articular injections, with the potential for fewer corticosteroid-related adverse effects. This may be particularly true in patients with diabetes, as some studies have demonstrated smaller fluctuations in serum blood glucose levels when the injection was performed in the subacromial space instead of intra-articular.[55]
Manipulation under anaesthesia
If oral pharmacotherapeutic interventions and corticosteroid injections do not provide sufficient pain relief, and the patient is not progressing in physiotherapy, then manipulation under general anaesthesia and pharmacological muscle relaxation can free adhesive and fibrotic tissues and may allow for a gain in range of motion.[56]
Early manipulation is more effective than manipulation later in the disease course.[56]
Patients may experience an increase in pain following manipulation. Placement of an inter-scalene anaesthetic block or inter-scalene infusion pump can allow for post-manipulative analgesia, and thus more aggressive post-manipulative physiotherapy. Care should be exercised when treating patients with previous surgery or poor bone quality, to prevent disruption of previous surgical repairs or fractures.
Concern over fracture or intra-articular pathology has led some to advocate for arthroscopic capsular release over manipulation under anaesthesia.[57][58] The two procedures may also be performed in conjunction.
To date, there have not been any high-quality studies to support the use of arthroscopic release with or without the addition of a manipulation under anaesthesia. However, one systematic review demonstrated a mild benefit of arthroscopic capsular release over manipulation under anaesthesia in recalcitrant idiopathic adhesive capsulitis and adhesive capsulitis in patients with diabetes.[59]
One multi-centre, three-armed, superiority randomised trial compared manipulation under anaesthesia, arthroscopic capsular release, or early structured physiotherapy in patients with adhesive capsulitis referred to secondary care. The study reported none of the interventions as clinically superior, based on the primary outcome targets of a 5-point difference on the Oxford Shoulder Score (OSS; 0-48) between physiotherapy and either form of surgery, or 4 points difference between manipulation and capsular release at 12 months after randomisation.[60]
Hydrodilation
There is evidence that hydrodilation (arthrographic distension with saline and corticosteroid) may provide short-term benefits in pain, range of movement, and function in patients with adhesive capsulitis.[61] However, it is uncertain whether this intervention is more effective than alternative treatment options.
One randomised trial evaluating the efficacy of three injection methods (i.e., intra-articular corticosteroid, subacromial space corticosteroid, and hydrodilation) in the treatment of primary adhesive capsulitis found more rapid improvement in pain and range of motion with hydrodilation at 1- and 3-month follow-up, but similar clinical outcomes among all three groups at the final follow-up at 6 months.[62]
Arthroscopic capsular release
The role of arthroscopy in the management of adhesive capsulitis was initially to evaluate the glenohumeral joint for any underlying or associated pathology. Joint distension via fluid inflow for arthroscopy was an added advantage. Over time, arthroscopy has come to play an essential role in the surgical treatment of refractory adhesive capsulitis. Arthroscopic release of the anterior capsule, rotator interval, and/or release of the coracohumeral ligament provides improvement in pain and function.[18][63][64][65] Both short-term and long-term benefits have been shown.[18][66][67]
A posterior capsular release may be considered with loss of internal rotation despite adequate physiotherapy and stretching. Release of the intra-articular portion of the subscapularis tendon and/or an extended release of the inferior glenohumeral ligament from inferior to posterior may improve range of motion, but only short-term results are available.[68][69]
The use of arthroscopic release is being considered earlier in the course of the disease. However, optimal timing of surgical intervention has yet to be defined.[Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted anterior capsule with extensive synovitis and thickeningFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].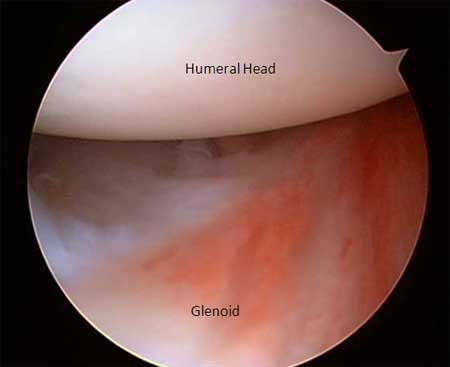 [Figure caption and citation for the preceding image starts]: Arthroscopic view of completed anterior releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of completed anterior releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].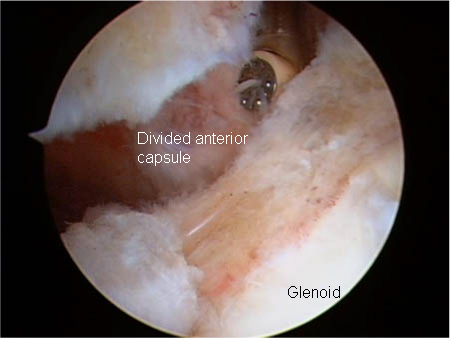 [Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted rotator interval showing extensive scarring and synovitisFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted rotator interval showing extensive scarring and synovitisFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].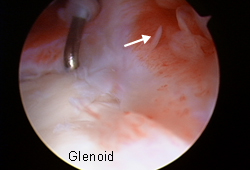 [Figure caption and citation for the preceding image starts]: Arthroscopic view of rotator interval releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of rotator interval releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].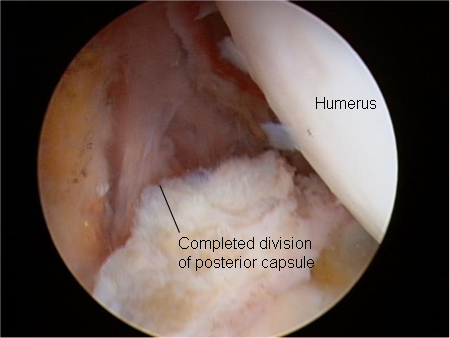 [Figure caption and citation for the preceding image starts]: Arthroscopic view of posterior capsular releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of posterior capsular releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].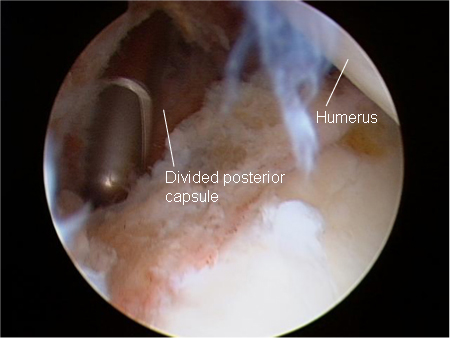
Use of this content is subject to our disclaimer