Fibrocystic breasts
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
mastalgia
supportive measures
Reassurance through an explanation of the effects of menstrual hormonal cycling and oestrogen effects is effective in relieving patient anxiety.
Most women find the use of a bra that provides good support to be helpful.
Some women seem to experience less discomfort when restricting caffeine or sodium intake in their diet; however, this has not been scientifically documented. Additionally, dietary supplementation with isoflavones (soy products) and a low fat, high fibre diet have been suggested as helpful for women with mastalgia; however, the evidence for these interventions is weak.[31]Murshid KRA. Review of mastalgia in patients with fibrocystic breast changes and the non-surgical treatment options. J Taibah Uni Med Sci. 2011;6(1):1-18.
In post-menopausal women receiving hormone replacement therapy (HRT), modification of therapy regimens is a reasonable approach given that the reported rates of HRT-induced breast pain vary for different combinations and preparations compared with placebo.[13]Cady B, Steele GD Jr, Morrow M, et al. Evaluation of common breast problems: guidance for primary care providers. CA Cancer J Clin. 1998 Jan-Feb;48(1):49-63. http://www.ncbi.nlm.nih.gov/pubmed/9449933?tool=bestpractice.com [28]Smith RL, Pruthi S, Fitzpatrick LA. Evaluation and management of breast pain. Mayo Clin Proc. 2004 Mar;79(3):353-72. http://www.ncbi.nlm.nih.gov/pubmed/15008609?tool=bestpractice.com
analgesia
Additional treatment recommended for SOME patients in selected patient group
A trial of a non-narcotic analgesic such as paracetamol, ibuprofen, or aspirin is suggested.
Primary options
paracetamol: 500-1000 mg every 4-6 hours when required, maximum 4000 mg/day
OR
ibuprofen: 300-400 mg every 6-8 hours when required, maximum 2400 mg/day
OR
aspirin: 300-900 mg every 4-6 hours when required, maximum 4000 mg/day
evening primrose oil (EPO)
Additional treatment recommended for SOME patients in selected patient group
Gamma-linolenic acid (GLA) is the active component of EPO.
Placebo-controlled, randomised trials have studied GLA with variable results. A meta-analysis of these trials demonstrates significant heterogeneity among them with overall absence of demonstrable benefit.[37]Srivastava A, Mansel RE, Arvind N, et al. Evidence-based management of Mastalgia: a meta-analysis of randomised trials. Breast. 2007 Oct;16(5):503-12. http://www.ncbi.nlm.nih.gov/pubmed/17509880?tool=bestpractice.com
Despite the lack of overwhelming data, EPO may be useful for some patients and has limited untoward effects.
May add on to initial supportive measures if pain persists despite treatment and advice, or has already been severe or prolonged by time of initial presentation. A trial of 3 to 6 months is necessary to observe a definitive effect.[24]Pruthi S, Wahner-Roedler DL, Torkelson CJ, et al. Vitamin E and evening primrose oil for management of cyclical mastalgia: a randomized pilot study. Altern Med Rev. 2010 Apr;15(1):59-67. http://www.ncbi.nlm.nih.gov/pubmed/20359269?tool=bestpractice.com
Primary options
evening primrose oil: 1 g/day orally initially for 3 weeks, increase by 1 g/day increments every 3-4 weeks according to response, maximum 3 g/day
hormonal therapy
If breast pain is severe, has persisted for more than 6 months, and significantly interferes with daily activities, hormonal therapy with tamoxifen, bromocriptine, or danazol can be considered.[25]Fentiman IS, Caleffi M, Hamed H, et al. Dosage and duration of tamoxifen treatment for mastalgia: a controlled trial. Br J Surg. 1988 Sep;75(9):845-6. http://www.ncbi.nlm.nih.gov/pubmed/3052691?tool=bestpractice.com [26]Parlati E, Polinari U, Salvi G, et al. Bromocriptine for treatment of benign breast disease. A double-blind clinical trial versus placebo. Acta Obstet Gynecol Scand. 1987;66(6):483-8. http://www.ncbi.nlm.nih.gov/pubmed/3321867?tool=bestpractice.com [27]Mansel RE, Wisbey JR, Hughes LE. Controlled trial of the antigonadotropin danazol in painful nodular benign breast disease. Lancet. 1982 Apr 24;1(8278):928-30. http://www.ncbi.nlm.nih.gov/pubmed/6122770?tool=bestpractice.com
Tamoxifen is a competitive inhibitor of oestrogen acting as an oestrogen agonist/antagonist; bromocriptine is a prolactin inhibitor; and danazol suppresses gonadotrophins resulting in androgenic, anti-oestrogenic, and antiprogestogenic activity.[25]Fentiman IS, Caleffi M, Hamed H, et al. Dosage and duration of tamoxifen treatment for mastalgia: a controlled trial. Br J Surg. 1988 Sep;75(9):845-6. http://www.ncbi.nlm.nih.gov/pubmed/3052691?tool=bestpractice.com [26]Parlati E, Polinari U, Salvi G, et al. Bromocriptine for treatment of benign breast disease. A double-blind clinical trial versus placebo. Acta Obstet Gynecol Scand. 1987;66(6):483-8. http://www.ncbi.nlm.nih.gov/pubmed/3321867?tool=bestpractice.com [27]Mansel RE, Wisbey JR, Hughes LE. Controlled trial of the antigonadotropin danazol in painful nodular benign breast disease. Lancet. 1982 Apr 24;1(8278):928-30. http://www.ncbi.nlm.nih.gov/pubmed/6122770?tool=bestpractice.com
Danazol is the only one of these medicines approved for breast pain; however, tamoxifen is more frequently used because it may be more effective and surgeons are more familiar with its use and adverse-effect profile. Danazol is rarely used owing to its masculinising adverse effects.
These treatments are infrequently used because of unwanted adverse effects.
Primary options
tamoxifen: 10 mg orally once daily on days 15-25 of menstrual cycle for 3 months
Secondary options
bromocriptine: 1.25 mg orally once daily at bedtime initially, increase by 1.25 mg/day increments over 2 weeks, usual dose is 2.5 mg twice daily
Tertiary options
danazol: 100 mg orally twice daily initially, starting on day 2 of menstrual cycle, decrease to 100 mg once daily starting on day 2 of cycle after 2 months, and then decrease to 100 mg once daily on days 14-28 of cycle or 100 mg on alternate days if amenorrhoeic
analgesia
Additional treatment recommended for SOME patients in selected patient group
A trial of a non-narcotic analgesic such as paracetamol, ibuprofen, or aspirin is suggested.
Primary options
paracetamol: 500-1000 mg every 4-6 hours when required, maximum 4000 mg/day
OR
ibuprofen: 300-400 mg every 6-8 hours when required, maximum 2400 mg/day
OR
aspirin: 300-900 mg every 4-6 hours when required, maximum 4000 mg/day
cyst aspiration
Treatment recommended for ALL patients in selected patient group
No treatment is required for an asymptomatic patient in whom a simple cyst is discovered on a screening examination or mammography.[32]Vargas HI, Vargas MP, Gonzalez KD, et al. Outcomes of sonography-based management of breast cysts. Am J Surg. 2004 Oct;188(4):443-7. http://www.ncbi.nlm.nih.gov/pubmed/15474446?tool=bestpractice.com
Aspiration is performed in most patients with a palpable cyst, especially if it is symptomatic (painful) or if there is concern about the exact diagnosis from the appearance on ultrasound (and aspiration is therefore for diagnostic purposes). The American Society of Breast Surgeons recommends that if an ultrasound confirms that a breast mass is a simple cyst, it does not need to be drained unless it is bothersome to the patient or has concerning features.[33]The American Society of Breast Surgeons. Benign breast disease. Five things physicians and patients should question. Jan 2018 [internet publication].
https://www.choosingwisely.org/societies/american-society-of-breast-surgeons-benign-breast-disease/
[Figure caption and citation for the preceding image starts]: Ultrasound image of a breast cyst (note the characteristic smooth and sharp margins of the anechoic lesion with posterior acoustic enhancement)Courtesy of Limin Yang, MD, and Justin Boatsman, MD, Department of Radiology, University of Iowa Hospital and Clinics; used with permission [Citation ends].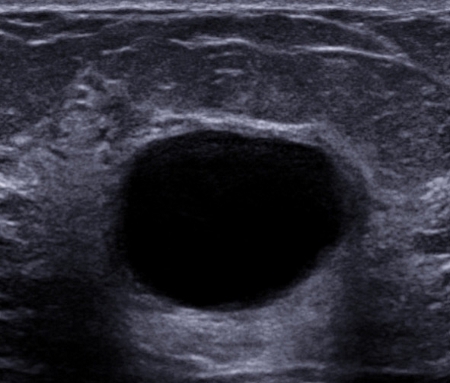
removal of lesion and risk reduction strategies
Treatment recommended for ALL patients in selected patient group
Patients with a breast mass require accurate diagnosis to exclude breast cancer or identify a high-risk histology. If biopsy reveals fibrocystic breast without atypia, no further therapy is necessary.
If there is evidence of atypical ductal hyperplasia, removal of the entire lesion and consideration of breast cancer risk reduction strategies is advised.[21]Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985 Jan 17;312(3):146-51. http://www.ncbi.nlm.nih.gov/pubmed/3965932?tool=bestpractice.com [34]Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005 Jul 21;353(3):229-37. https://www.nejm.org/doi/full/10.1056/NEJMoa044383#t=article http://www.ncbi.nlm.nih.gov/pubmed/16034008?tool=bestpractice.com [35]Fisher B, Constantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998 Sep 16;90(18):1371-88. https://jnci.oxfordjournals.org/content/90/18/1371.full.pdf http://www.ncbi.nlm.nih.gov/pubmed/9747868?tool=bestpractice.com
nipple discharge
reassurance with observation
Patients with non-suspicious nipple discharge require no further intervention. Reassurance and observation are sufficient.
referral to a surgeon
Patients with any nipple discharge and a palpable accompanying mass or mammographic abnormality should be referred to a surgeon immediately.
referral and surgery
Expert consultation must be obtained when suspicious nipple discharge is encountered, even if no palpable mass is present or mammography is normal.[36]Vargas HI, Romero L, Chlebowski RT. Management of bloody nipple discharge. Curr Treat Options Oncol. 2002 Apr;3(2):157-61. http://www.ncbi.nlm.nih.gov/pubmed/12057078?tool=bestpractice.com
If discharge is bloody and very profuse, it may be necessary to perform either microductectomy (removal of single symptomatic milk duct) or central duct excision.
In patients with non-suspicious nipple discharge and negative imaging studies for malignancy and prolactinoma, but in whom the discharge is profuse and significantly impacts a patient's quality of life, excision of the central duct complex may help control the discharge.[36]Vargas HI, Romero L, Chlebowski RT. Management of bloody nipple discharge. Curr Treat Options Oncol. 2002 Apr;3(2):157-61. http://www.ncbi.nlm.nih.gov/pubmed/12057078?tool=bestpractice.com [38]Vargas HI, Vargas MP, Eldrageely K, et al. Outcomes of clinical and surgical assessment of women with pathological nipple discharge. Am Surg. 2006 Feb;72(2):124-8. http://www.ncbi.nlm.nih.gov/pubmed/16536240?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer