Differentials
Common
Trauma
History
history of trauma (including gunshot wounds, major fractures, crush injuries); history of prior bleeding episodes; or use of anticoagulants or non-steroidal anti-inflammatory drugs (NSAID)
Exam
evidence of injury (wounds, bruises, deformities), hypotension, pallor, tachycardia, thready pulse, dyspnoea/air hunger, altered mental status or confusion; flat neck veins when supine indicate volume loss
1st investigation
- FBC:
normal or decreased haematocrit; decreased haemoglobin; hyperproliferative; reactive leukocytosis and thrombocytosis due to a stress response, thrombocytopenia from dilutional effect of multiple transfusions
- prothrombin time/activated partial thromboplastin time:
usually normal; prolonged with anticoagulants, underlying defects in haemostasis, or consumptive coagulopathy
More - joint or spine x-rays:
identification of fractures
Other investigations
- diagnostic laparotomy:
identification of bleeding source
- CT scan of affected body region:
identification of internal injuries
Acute gastrointestinal bleeding
History
history of prior episodes of gastrointestinal bleeding, gastritis, peptic ulcer disease, hiatal hernia, neoplastic disease, non-steroidal anti-inflammatory drug (NSAID) or corticosteroid use, alcohol use, cirrhosis, anticoagulants, ulcerative colitis, diverticular disease; symptoms of rectal bleeding, melaena, haematemesis, abdominal pain
Exam
hypotension, pallor, tachycardia, thready pulse, dyspnoea/air hunger, altered mental status or confusion; flat neck veins when supine indicate volume loss; ascites, hepatomegaly/splenomegaly, cirrhotic hard liver, caput medusae, gynaecomastia, melaena, or bright red blood on rectal examination
1st investigation
- FBC:
normal or decreased haematocrit; decreased haemoglobin; hyperproliferative; reactive leukocytosis and thrombocytosis due to a stress response
- reticulocyte count:
>2%
More - prothrombin time/activated PTT:
usually normal; prolonged in cirrhosis, anticoagulant therapy, or underlying defects in haemostasis; elevated urea may be seen
- upper gastrointestinal endoscopy:
bleeding varices or ulcers if source is from upper gastrointestinal tract
- colonoscopy:
visualisation of bleeding lesion or mass
Other investigations
Rupture of a vascular aneurysm
History
sudden tearing pain, affecting the back, abdomen or chest depending on aneurysm location, may be accompanied by loss of consciousness if major vessel involved; history of hypertension, collagen disorders, trauma, cocaine or amphetamine use
Exam
hypotension, pallor, tachycardia, dyspnoea/air hunger, altered mental status or confusion; flat neck veins when supine indicate volume loss; wide pulse pressure or absent distal pulses; thready pulse, may rapidly progress to circulatory collapse and death
1st investigation
- FBC:
normal or decreased haematocrit; decreased haemoglobin; hyperproliferative; reactive leukocytosis and thrombocytosis due to a stress response
- reticulocyte count:
>2%
More - ultrasonography of affected region:
shows extent and nature of aneurysm
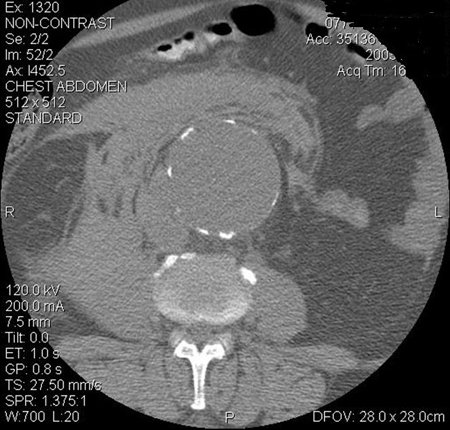
More - CT scan of affected region:
shows extent and nature of aneurysm
More
Other investigations
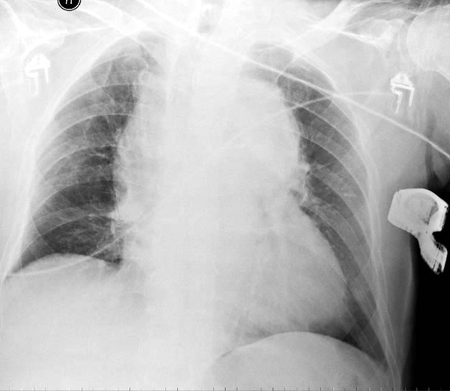
- chest x-ray:
may show widened mediastinum in thoracic aortic aneurysm
More
Surgery
History
recent surgery with at least moderate blood loss; history of bleeding disorders or excessive bruising; use of antibiotics
Exam
hypotension, pallor, tachycardia, thready pulse, continuous bleeding from surgical wound, petechiae, purpura; severe bleeding produces dyspnoea/air hunger, altered mental status or confusion; flat neck veins when supine indicate volume loss
1st investigation
- FBC:
normal or decreased haematocrit; decreased haemoglobin; hyperproliferative; reactive leukocytosis and thrombocytosis due to a stress response
Other investigations
- reticulocyte count:
>2%
- ultrasound of affected region:
shows source and extent of bleeding
- CT scan of affected region:
shows source and extent of bleeding
- diagnostic laparotomy:
shows source and extent of bleeding
Menorrhagia
History
excessive menstrual bleeding; fatigue, dyspnoea on exertion, pica; history of fibroids
Exam
pallor, adnexal masses or fibroids
1st investigation
- FBC:
chronic microcytic anaemia with normal WBC; reactive thrombocytosis if iron deficient
- serum ferritin:
<100 picomol/L (<45 micrograms/L) is suggestive of iron deficiency anaemia
More
Other investigations
- pregnancy test:
negative
- prothrombin time/activated partial thromboplastin time:
usually normal; prolonged with anticoagulants, underlying defects in haemostasis
- thyroid-stimulating hormone (TSH)/free thyroxine (T4):
elevated TSH with low free T4 in hypothyroidism
- transvaginal ultrasound:
may see hyperplasia, dysplasia, fibroids, or polyps
More
Iron deficiency
History
history of poor dietary iron intake, coeliac disease, Crohn's disease, ulcerative colitis, small bowel resection, peptic ulcer disease, regular running, chronic blood loss (melaena, haematuria, menorrhagia, haemoptysis, frequent blood donation, self-harm), pica, salicylate ingestion, gastric bypass, hookworm infestation, pregnancy
Exam
pallor, dyspnoea, poor exercise tolerance, koilonychia, angular cheilosis, glossitis, thinning hair, systolic flow murmur; haemorrhoids, fresh blood or melaena on rectal examination; evidence of pregnancy; adnexal masses or fibroids
1st investigation
- FBC with peripheral smear:
microcytic anaemia with thrombocytosis
- serum iron studies:
low serum iron, elevated total iron-binding capacity, low ferritin, elevated soluble transferrin receptor
- tissue transglutaminase (tTG) IgA test and total IgA test (on gluten containing diet):
tTG IgA level elevated in the presence of normal IgA indicates celiac disease
- faecal occult blood (FOBT):
positive if gastrointestinal bleeding is present
- faecal immunochemical test (FIT):
positive quantitative FIT suggests bleeding from lower gastrointestinal tract
More
Other investigations
- upper gastrointestinal endoscopy:
identification of source of upper gastrointestinal bleeding; elevated gastric pH in achlorhydria
- colonoscopy:
identification of source of lower gastrointestinal bleeding or chronic inflammation
- CT colonography:
identification of source of lower gastrointestinal bleeding
More - flow cytometry:
identification of paroxysmal nocturnal haemoglobinuria
- transvaginal ultrasound:
may see hyperplasia, dysplasia, fibroids, or polyps
More - stool microscopy:
visualisation of hookworm, whipworm, or Schistosoma eggs
- Helicobacter pylori test:
positive result if H pylori present
More
Vitamin B12 deficiency
History
history of coeliac or Crohn's disease, autoimmune thyroid disease, gastric bypass, chronic antibiotic use (intestinal bacterial overgrowth syndrome), vegan diet or alcohol misuse; fatigue, palpitations, distal paraesthesias, depression, confusion, tinnitus, dementia
Exam
impaired vibration sense and extremity numbness, vitiligo, glossitis, poor balance or co-ordination, tachycardia, pallor, hepatosplenomegaly
1st investigation
- FBC with peripheral smear:
megaloblastic macrocytic anaemia; basophilic stippling may be seen
More - serum vitamin B12 levels:
low
More - serum methylmalonic acid levels:
elevated
More - anti-intrinsic factor antibodies:
positive in pernicious anaemia
- antiparietal cell antibodies:
positive in pernicious anaemia
- tissue transglutaminase (tTG) IgA test and total IgA test (on gluten containing diet):
tTG IgA level elevated in the presence of normal IgA indicates coeliac disease
Other investigations
- homocysteine levels:
elevated
More
Folate deficiency
History
history of coeliac or Crohn's disease, gastric bypass, haemodialysis, pregnancy, alcohol misuse, or use of anti-seizure medications; fatigue, palpitations, headaches
Exam
mild persistent pyrexia, tachycardia, pallor, hepatosplenomegaly, glossitis, angular stomatitis, patchy hyperpigmentation of skin and mucous membranes
1st investigation
Other investigations
- serum homocysteine levels:
elevated
Myelodysplastic syndrome
History
history of prior exposure to petroleum distillates (especially benzene), chemotherapy, or radiotherapy; fever, chills, fatigue, weakness, recurrent infection, anorexia, night sweats, shortness of breath, easy bruising
Exam
pallor, petechiae, purpura
1st investigation
- FBC:
nonmegaloblastic macrocytic anaemia with leukopenia, macro-ovalocytes; associated cytopenias include neutropenia and thrombocytopenia
- reticulocyte count:
<2%
Acute lymphoblastic leukaemia
History
malaise, fatigue, easy bruising or bleeding, recurrent infections, fever, arthralgias, infection, anorexia, night sweats, shortness of breath, bony tenderness, epistaxis, bleeding gums, gingival hyperplasia
Exam
pallor, petechiae, purpura, tachycardia, hepatosplenomegaly, lymphadenopathy, painless scrotal enlargement, bleeding gums
1st investigation
- FBC with peripheral smear:
pancytopenia, with ≥20% blasts; normocytic anaemia; may see hypereosinophilia
More - reticulocyte count:
<2%
Other investigations
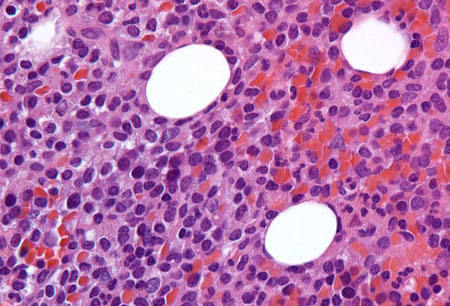
- bone marrow aspirate and biopsy:
≥20% blasts
More
Acute myeloid leukaemia
History
history of prior chemotherapy or radiotherapy; malaise, night sweats, fatigue, easy bruising or bleeding, recurrent infections, fever, bony tenderness, epistaxis, bleeding gums, gingival hyperplasia
Exam
pallor, petechiae, purpura, dyspnoea, tachycardia
1st investigation
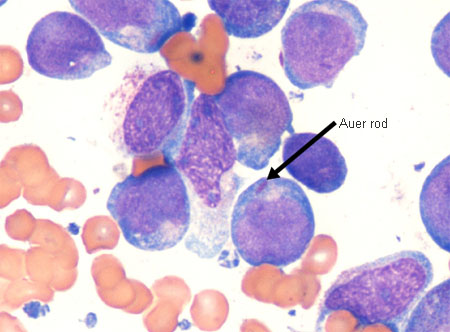
- FBC with peripheral smear:
hypoproliferative; pancytopenia, with ≥20% blasts; normocytic anaemia; may see hypereosinophilia
More - reticulocyte count:
<2%
Other investigations
- bone marrow aspirate and biopsy:
≥20% blasts
More
Chronic myeloid leukaemia
History
usually in middle-aged patients; fatigue, weight loss, night sweats, early satiety, petechiae, purpura, recurrent fevers, bone pain, gouty arthritis
Exam
tender splenomegaly, painful sternum, lymphadenopathy
1st investigation
- FBC with peripheral smear:
hypoproliferative; normocytic anaemia; myeloid maturing cells, elevated basophils, and eosinophils
- reticulocyte count:
<2%
- bone marrow aspirate and biopsy:
hypercellular with granulocytic hyperplasia
Other investigations
- cytogenetics:
t(19;22) Philadelphia chromosome - BCR::ABL1 translocation
- serum uric acid:
elevated
More
Hairy cell leukaemia
History
weakness, fatigue, weight loss, night sweats, early satiety, petechiae, purpura, recurrent fevers, abdominal discomfort or fullness due to large spleen
Exam
massive splenomegaly
1st investigation
- FBC with peripheral smear:
pancytopenia with normocytic anaemia
More - reticulocyte count:
<2%
Other investigations
- bone marrow aspirate and biopsy:
core biopsy shows hairy cells
More
Acquired aplastic anaemia
History
history of hepatitis, HIV, benzene exposure, use of known causative medications, radiation exposure, paroxysmal nocturnal haemoglobinuria; malaise, fatigue, easy bruising or bleeding, recurrent infections, fever
Exam
pallor, petechiae, purpura, dyspnoea, tachycardia
1st investigation
- FBC with peripheral smear:
hypoproliferative; pancytopenia with mild macrocytosis; normocytic anaemia
- reticulocyte count:
<2%
Infiltration by secondary malignancy
History
weight loss, malaise, fevers, fatigue, dyspnoea, easy bleeding or bruising; history of solid organ malignancy (particularly breast, prostate, lung, neuroblastoma)
Exam
pallor, petechiae, purpura, tachycardia, abnormal exam or presence of mass (if solid organ malignancy), bruising, cachexia
1st investigation
- FBC with peripheral smear:
hypoproliferative; pancytopenia, teardrop cells, poikilocytes; normocytic anaemia
- reticulocyte count:
<2%
- bone marrow aspirate and biopsy:
infiltration of marrow space by malignant cells
More
Other investigations
- CT imaging:
identification of site of primary malignancy
Pure red cell aplasia
History
self-limiting disease: history of use of known causative medications, clinical features of causative infections (parvovirus B19, infectious mononucleosis, viral hepatitis, malaria, respiratory infections, gastroenteritis, primary atypical pneumonia, mumps); chronic disease: history of autoimmune disease (systemic lupus erythematosus [SLE], rheumatoid arthritis, dermatomyositis, scleroderma, polyarteritis nodosa), persistent infection, or thymoma
Exam
clinical signs of underlying infection or autoimmune disease
1st investigation
- FBC:
hypoproliferative; normocytic anaemia
- reticulocyte count:
<2%
- trial of discontinuation of causative medication:
anaemia resolves
- antiparvovirus B19 antibodies:
positive in parvovirus infection
More
Other investigations
- thick and thin peripheral smear:
intracellular parasites seen with Wright's or Giemsa staining in malaria infection
- serum IgM + IgG anti-HAV:
positive in hepatitis A infection
- serum IgM + IgG HBcAb:
positive in hepatitis B infection
- serum HBsAg:
positive in hepatitis B infection
- serum IgM + IgG anti-HCV:
positive in hepatitis C infection
- antinuclear antibodies:
positive in SLE or scleroderma
- ds-DNA, Smith's antigen:
positive in SLE
- rheumatoid factor:
positive in rheumatoid arthritis
- serum creatine kinase:
elevated in dermatomyositis
- chest x-ray:
infiltrates in atypical pneumonia; smooth mass in thymoma, typically projecting into one of the hemi-thoraces and obscuring the aortic arch, or silhouette sign
Drug toxicity
History
known or suspected ingestion of causative drug prior to onset of anaemia, poor exercise tolerance
Exam
pallor, jaundice (with haemolytic anaemia only), dyspnoea
1st investigation
- FBC with peripheral smear:
hypoproliferative or hyperproliferative; typically normocytic anaemia; inhibitors of DNA synthesis, folate, or vitamin B12 produce megaloblastic macrocytic anaemia
- reticulocyte count:
<2% if drugs suppress bone marrow; >2% if drugs produce haemolysis
- trial of discontinuation of causative medication:
anaemia resolves
Other investigations
- serum bilirubin:
elevated in haemolytic anaemia
Anaemia of chronic disease
History
history of known chronic inflammatory, autoimmune, or infectious states; sustained physiological stress, renal failure, liver disease, heart failure, hypothyroidism, vasculitis or collagen vascular diseases, inflammatory bowel disease, hypogonadism; poor exercise tolerance; anaemia correlates with severity of inflammatory process
Exam
pallor, fatigue, dyspnoea; specific signs of underlying disease
1st investigation
Other investigations
- serum erythropoietin level:
normal or elevated; often decreased in chronic kidney disease
More
Chronic kidney disease
History
chronic kidney disease, poor exercise tolerance; features of secondary hypoparathyroidism: muscle cramps, bone pain
Exam
pallor, fatigue, dyspnoea; signs of renal failure: jaundice, skin bruising, lung rales, pericardial rub, oedema, poor concentration or memory, myoclonus; positive Chvostek's sign or Trousseau's sign in associated hyperparathyroidism
1st investigation
- FBC:
hypoproliferative; normocytic or microcytic anaemia with thrombocytosis
- reticulocyte count:
<2%
- serum creatinine:
elevated
- urinalysis:
haematuria and/or proteinuria
- serum iron studies:
low serum iron and normal/elevated ferritin, high total iron-binding capacity in iron deficiency
- serum erythropoietin level:
normal or decreased
Other investigations
- serum calcium level:
decreased in associated secondary hyperparathyroidism
- serum intact parathyroid hormone level:
increased in associated secondary hyperparathyroidism
- renal ultrasound:
small kidney size; presence of obstruction or hydronephrosis; kidney stones
- kidney biopsy:
identification of underlying kidney pathology
Chronic liver disease
History
history of chronic liver disease, poor exercise tolerance; may be asymptomatic or with fatigue, weakness, weight loss, recurrent infections, decreased libido; altered mental status in hepatic encephalopathy
Exam
pallor, fatigue, dyspnoea, jaundice, lower-extremity swelling; hand and nail features: leukonychia, palmar erythema, finger clubbing, spider angiomata; facial features: telangiectasia, bruising, rhinophyma, parotid gland swelling, paper-dollar appearance of skin, seborrhoeic dermatitis, xanthelasma; abdominal features: caput medusae, bruising, hepatomegaly, splenomegaly, abdominal distension; in males, loss of secondary sexual hair and testicular atrophy, gynaecomastia
1st investigation
- FBC:
non-megaloblastic macrocytic anaemia; thrombocytopenia may be present
- prothrombin time:
decreased in hepatic synthetic dysfunction
- LFTs:
abnormal; pattern depends on underlying cause
Other investigations
- abdominal ultrasound, CT, or MRI scanning:
liver surface nodularity, small liver, possible hypertrophy of left/caudate lobe, evidence of ascites or collateral circulation
- liver biopsy:
diagnosis of underlying cause or subsequent cirrhosis
Pregnancy
History
pregnancy, especially in third trimester
Exam
abdominal distension consistent with pregnancy, pallor
1st investigation
- FBC:
microcytic anaemia with thrombocytosis in iron deficiency; megaloblastic macrocytic anaemia in folate deficiency; microangiopathic haemolytic anaemia with RBC fragmentation is a finding in HELLP (haemolysis, elevated liver enzyme levels, and thrombocytopaenia) syndrome
Other investigations
- serum iron studies:
low serum iron, elevated total iron-binding capacity, low ferritin, elevated soluble transferrin receptor in iron deficiency
- serum folate:
low in folate deficiency
More
Uncommon
Generalised malnutrition
History
protein calorie deprivation; malabsorption syndrome; neglect; history of an eating disorder
Exam
loss of subcutaneous fat, apathy and lethargy, depigmentation, enlarged abdomen, winged scapula, flaky skin, bipedal oedema
1st investigation
- FBC with peripheral smear:
microcytic anaemia in iron deficiency; megaloblastic macrocytic anaemia in vitamin B12 and folate deficiency; normocytic anaemia with combined vitamin and mineral deficiencies
- serum iron studies:
low serum iron, elevated total iron-binding capacity, and low ferritin in iron deficiency
Cytotoxic chemotherapy
Radiotherapy
History
history of recent radiation exposure, especially to pelvic or sternal areas; fatigue, headaches, poor exercise tolerance
Exam
pallor, lethargy, dyspnoea, skin erythema on radiation sites
1st investigation
- FBC:
anaemia (pancytopenia)
- reticulocyte count:
<2%
Other investigations
- bone marrow aspirate and biopsy:
marrow fibrosis or malignant infiltration
Alcohol misuse
History
history of chronic high alcohol intake
Exam
overweight status, increased prominence of superficial cutaneous vasculature, peripheral neuropathy, alterations in normal dentition and halitosis, possible signs of liver disease: hepatomegaly or small liver, jaundice, ascites
1st investigation
- FBC:
macrocytic anaemia; megaloblastic or nonmegalobastic
Other investigations
- diagnostic interview:
diagnosis of alcohol dependence
- alcohol level (breath and blood):
elevated
Lead toxicity
History
history of occupational or recreational exposure to lead products or old paint; neuropsychiatric disturbance, insomnia, abdominal pain, poor appetite, pica
Exam
blue gingival line (Burton's line), hypertension, gout (saturnine gout); wrist or foot drop
1st investigation
- FBC with peripheral smear:
normocytic anaemia with basophilic stippling; microcytic anaemia if associated iron deficiency is present
- reticulocyte count:
>2%
- whole blood lead level:
elevated
Other investigations
Hypothyroidism
History
weakness, lethargy, slow speech, feeling cold, forgetfulness, constipation, weight gain, poor exercise tolerance
Exam
pallor; dyspnoea; coarse, dry skin; eyelid oedema; thick tongue; facial oedema; bradycardia
1st investigation
- FBC:
hypoproliferative; normocytic anaemia; macrocytic, megaloblastic if hypothyroidism is associated with autoimmune disease
- serum thyroid-stimulating hormone:
elevated
- serum thyroxine:
reduced
- reticulocyte count:
<2%
Other investigations
Autoimmune haemolytic anaemia
History
history of autoimmune diseases (systemic lupus erythematosus [SLE], rheumatoid arthritis, or scleroderma), lymphoproliferative disorders (non-Hodgkin's lymphoma or chronic lymphocytic leukaemia), recent viral illness, or mononucleosis; may be asymptomatic; symptoms include weakness, fatigue, headaches, poor exercise tolerance, prior gallstones, dark urine, clay-coloured stools
Exam
pallor, lethargy, dyspnoea, tachycardia, jaundice, splenomegaly (especially if extravascular haemolysis)
1st investigation
Other investigations
- antinuclear antibodies:
positivein SLE or scleroderma
- ds-DNA, Smith antigen:
positive in SLE
- rheumatoid factor:
positive in rheumatoid arthritis
Transfusion reaction
History
multiple prior transfusions; fever, back pain, and dyspnoea, usually within 6 hours of transfusion; recent blood transfusion may be associated with normocytic anaemia, haemolysis and hyperproliferation of reticulocytes due to a transfusion reaction
Exam
pallor, lethargy, dyspnoea, dark urine, jaundice
1st investigation
- ABO typing:
discrepancy to blood used for transfusion
More - inspection of plasma in centrifuged, anticoagulated venous blood sample:
clear or pink-red within first few hours of haemoglobinaemia
- inspection of centrifuged urine:
clear red in haemoglobinaemia
Other investigations
- direct antiglobulin (Coombs') test:
IgG anti-A, anti-B, or anti-AB detected on circulating red cells
- serum bilirubin:
elevated
Malaria
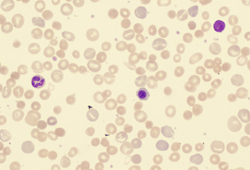
History
history of mosquito bite or habitation in malaria-prone region; fatigue, dyspnoea, fevers and prostration, decreased exercise tolerance, headaches, malaise; symptoms usually cycle every 48 to 72 hours, coinciding with red blood cell (RBC) destruction
Exam
jaundice or pallor, splenomegaly, dyspnoea, high flow cardiac murmur, pulmonary oedema, dark urine, fevers
1st investigation
Other investigations
- serum bilirubin:
elevated
- rapid diagnostic tests (RDTs):
detection of parasite antigen or enzymes
More
Viral hepatitis
History
perinatal exposure, direct body fluid transmission, exposure to foodborne outbreak (in hepatitis A); nausea, vomiting, abdominal pain, fever, malaise, fatigue and headache, dark urine, acholic (clay-coloured) stools, jaundice, pruritus (in hepatitis B); hepatitis C is usually asymptomatic
Exam
jaundice, hepatomegaly, right upper quadrant pain, acholic stools, maculopapular or urticarial skin rash (in hepatitis B); usually normal in hepatitis C
1st investigation
- FBC:
hypoprolifeartive; normocytic anaemia
- reticulocyte count:
<2%
- serum aminotransferases:
elevated
- serum IgM + IgG anti-HAV:
positive in hepatitis A infection
- serum IgM + IgG HBcAb:
positive in hepatitis B infection
- serum HBsAg:
positive in hepatitis B infection
- serum IgM + IgG anti-hepatitis C virus:
positive in hepatitis C infection
Other investigations
Toxoplasmosis
History
usually seen in pregnant or immunosuppressed patients and newborns; history of exposure to domestic cats, sheep, or cattle, or to raw meat
Exam
jaundice, fever, fatigue, lethargy, rash, hepatosplenomegaly; newborns infected in utero may have chorioretinitis, microcephaly, seizures, intellectual disability
1st investigation
- FBC:
hypoproliferative; normocytic anaemia and thrombocytopenia; may see leukocytosis and eosinophilia
- reticulocyte count:
>2%; usually 4%
- IgM enzyme-linked immunosorbent assay (ELISA) or IgG avidity test:
IgM detected in acute infection; IgG detected in chronic or previous exposure
More - Sabin-Feldman dye test:
IgG antibodies positive
Other investigations
- polymerase chain reaction for Toxoplasma gondii:
positive
Leishmaniasis
History
history of exposure to sandfly bite, especially in tropical or subtropical zones; AIDS, immunosuppression, or malnutrition; fatigue and anorexia; prolonged, persistent, low-grade intermittent fevers; failure to thrive, distended abdomen
Exam
pallor, jaundice, hepatosplenomegaly, lymphadenopathy, diarrhoea, skin ulcerations, nasopharyngeal ulcerations
1st investigation
- FBC:
hypoproliferative; normocytic anaemia, thrombocytopenia, leukopenia, erythroblastosis
- Leishmania serology:
positive for Leishmania antibodies, or antibody titre above locally validated threshold
More
Parvovirus B19 infection
History
acute infection: characteristic skin rash with or without arthralgia
Exam
acute infection: 'slapped cheek' appearance followed by a reticular erythematous eruption on extremities, and arthritis of hands, wrists, knees, or ankles
1st investigation
- FBC:
hypoproliferative; normocytic anaemia
- reticulocyte count:
<2%
Other investigations
- antiparvovirus B19 antibodies:
positive
More
Infectious mononucleosis
History
fatigue, malaise, sore throat, nausea, ocular pain, photophobia
Exam
fever, lymphadenopathy, pharyngitis, rash, tender splenomegaly, palatal petechiae, periorbital oedema, jaundice
1st investigation
- FBC with peripheral smear:
hypoproliferative or hyperproliferative; normocytic anaemia, with spherocytes and atypical lymphocytes
- reticulocyte count:
>2% and usually 4% in haemolytic anaemia, <2% in pure red cell aplasia
Other investigations
- LDH:
elevated
- haptoglobin:
low
- monospot test or viral capsid antigen (VCA) IgM:
positive
Cytomegalovirus (CMV)
History
infection is usually asymptomatic; a maculopapular rash following administration of antibiotics may occur; fatigue occurs due to anaemia; symptomatic infection is a sign of underlying immunosuppression
Exam
usually normal; jaundice occurs due to haemolytic anaemia; symptomatic infection produces fever, lymphadenopathy, pharyngitis, rash, tender splenomegaly, palatal petechiae, periorbital oedema
1st investigation
- FBC:
hyperproliferative; normocytic anaemia
- reticulocyte count:
>2%; usually 4%
Other investigations
- LDH:
elevated
- haptoglobin:
low
- monospot test or viral capsid antigen (VCA) IgM:
negative
More - CMV IgM:
positive
Sickle cell anaemia
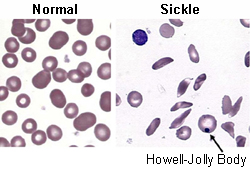
History
known diagnosis of sickle cell disease in patient and/or parents; prior painful vaso-occlusive crises; fatigue, poor exercise tolerance, persistent pain in skeleton, chest, or abdomen, priapism, gallstones, stroke, lower-extremity skin ulcers, pneumonia-like syndrome
Exam
high fever, pallor, lethargy, dyspnoea, jaundice during acute crisis
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia with sickle cells
More - reticulocyte count:
>2%
- haemoglobin (Hb) isoelectric focusing:
elevated HbS/A ratio (close to 100/0)
- LDH:
elevated
- serum bilirubin:
elevated
Other investigations
Thalassaemias
History
family history of blood disorders, especially requiring repeated transfusions; Mediterranean, Middle Eastern, or Southeast Asian descent; variable severity ranging from asymptomatic to severe transfusion-dependent symptoms
Exam
splenomegaly, jaundice, abdominal distension, skeletal abnormalities, large head, chipmunk facies, and misaligned teeth seen in beta-thalassaemia intermedia and major
1st investigation
- FBC with peripheral smear:
hypoproliferative or hyperproliferative; microcytic anaemia with MCV typically closer to 70 fL, low mean corpuscular haemoglobin (Hb); target cells seen
- reticulocyte count:
usually <2%, which differentiates impaired erythrocytosis from increased consumption of erythrocytes (which would result in a reticulocyte count of >2%)
More - Hb analysis:
elevated HbF; other Hb patterns consistent with respective thalassaemias
Other investigations
- serum ferritin:
elevated in iron overload
Hereditary spherocytosis
History
family history of blood disorder, splenectomy, or pigmented gallstones; may be asymptomatic if extramedullary haematopoiesis compensates
Exam
may be normal or show pallor, jaundice, lower leg skin ulcers, splenomegaly
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia, with increased mean corpuscular haemoglobin and spherocytes
- reticulocyte count:
>2%
- osmotic fragility test:
positive (cells lyse on exposure to hypo-osmotic solution)
Other investigations
- direct antiglobulin (Coombs') test:
negative
More
Glucose-6-phosphate dehydrogenase deficiency (G6PD)
History
usually in males of African, Mediterranean, Sardinian, or Sephardic Jewish descent; self-limiting episodes of acute haemolysis when exposed to oxidant stress; life-threatening symptoms more common with the Mediterranean variant
Exam
pallor, jaundice, mild dyspnoea
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia with Heinz bodies, eccentrocytes, or bite cells
More - reticulocyte count:
>2%
- serum haptoglobin:
decreased
- LDH:
elevated
Bone marrow failure syndromes
History
recurrent infection shortly after birth, fever, easy bleeding or bruising, organ abnormalities, short stature
Exam
ill-appearing, with weight loss, pallor, lethargy, dyspnoea, petechiae, purpura, and/or thrush
1st investigation
- FBC with peripheral smear:
pancytopenia with normocytic or macrocytic nonmegaloblastic anaemia
More - reticulocyte count:
<2%
Other investigations
- bone marrow aspiration and biopsy:
varies depending on underlying cause
- diepoxybutane or mitomycin-c fragility test:
positive in Fanconi anaemia
- genetic testing:
characteristic genetic mutations detected
Haemolytic uraemic syndrome
History
acute renal failure usually following an enteric bacterial infection (Escherichia coli 0157:H7) with bloody diarrhoea, or Streptococcus pneumoniae; ciclosporin, tacrolimus, clopidogrel, oral contraceptive pills, and some chemotherapy drugs may cause haemolytic uraemic syndrome
Exam
pallor, lethargy, dyspnoea, petechiae, purpura, bloody diarrhoea; usually self-limiting in children
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia, thrombocytopenia, schistocytes
- erythrocyte count:
>2%
Other investigations
- prothrombin time/activated PTT:
normal
More - serum haptoglobin:
decreased
- LDH:
elevated
- serum creatinine:
may be elevated
- serum bilirubin:
elevated
- direct antiglobulin (Coombs') test:
negative
More - stool culture and polymerase chain reaction tests:
postive for enterohaemorrhagic E. coli genes
- enzyme-linked immunosorbent assay:
positive for Shiga toxin
- urinalysis:
may show haematuria and/or proteinuria
Disseminated intravascular coagulation (DIC)
History
ongoing severe infection, sepsis (typically gram-negative), malignancy, obstetric emergency, trauma, burns, envenomations, drug overdose, any cause of endothelial damage
Exam
diffuse bleeding, especially from puncture sites or minor trauma; unprovoked clots; clinical signs of underlying cause
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia, thrombocytopenia, schistocytes
- reticulocyte count:
>3% assuming there is adequate marrow function
- prothrombin time:
prolonged
- activated partial thromboplastin time:
varies depending on factor VII levels
- DIC panel:
elevated D-dimer and fibrin degradation products with low fibrinogen
More
Other investigations
Thrombotic thrombocytopenic purpura
History
non-specific prodrome followed by headache, confusion, focal weakness, seizures, coma; menorrhagia may be seen due to bleeding
Exam
pallor, lethargy, dyspnoea, purpura, ecchymoses
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia with schistocytes
- reticulocyte count:
>2%
- direct antiglobulin (Coombs') test:
negative
More
Other investigations
Haemangioma
History
typically young child or infant with expanding vascular skin lesion; may also be hepatic or in other visceral site
Exam
depends on location of lesion(s), which are typically reddish-brown or violaceous; other symptoms consistent with anaemia
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia, thrombocytopenia
More - reticulocyte count:
>2%
Other investigations
- x-ray of suspected region:
soft-tissue shadows, phleboliths
- MRI of suspected region:
increased signal on both T1- and T2-weighted images with areas of signal void
Malignant hypertension
History
history of essential hypertension, renal disease, or eclampsia; older age, male gender, black ethnicity; dizziness, headache, mental status changes, loss of sensation or motor strength, chest pain or pressure, dyspnoea, oedema
Exam
systolic BP >210 mmHg and diastolic BP >130 mmHg, lethargy, new murmurs, third heart sound on auscultation of heart, jugular venous distension, rales or lower-extremity oedema, oliguria or polyuria, focal neurological signs, hypertensive retinopathy
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia with schistocytes
- reticulocyte count:
>2%
- ECG:
evidence of ischaemia or infarct such as ST- or T-wave changes
- serum creatinine:
elevated with renal failure
Other investigations
- chest x-ray:
evidence of pulmonary oedema indicating left ventricular failure
- head CT or MRI:
evidence of infarct or haemorrhage
Prosthetic valves and surfaces
History
history of aortic or mitral metallic valve replacement, with anticoagulation; weakness, fatigue, headaches; poor exercise tolerance, prior gallstones, dark urine
Exam
pallor, lethargy, dyspnoea, petechiae, purpura, jaundice
1st investigation
- FBC with peripheral smear:
hyperproliferative; normocytic anaemia with schistocytes
- reticulocyte count:
>2%
- direct antiglobulin (Coombs') test:
negative
More
Other investigations
Cutaneous burns
History
burn injury to at least 10% of total body surface area; multiple surgical procedures
Exam
epidermal or dermal loss consistent with burn injury
1st investigation
- FBC with peripheral smear:
normocytic anaemia with thrombocytopenia; schistocytes from peripheral destruction seen on blood smear
Other investigations
- reticulocyte count:
>2%
Use of this content is subject to our disclaimer
 ]
]