Differentials
Common
Chronic obstructive pulmonary disease (COPD)
History
progressive dyspnoea over a period of years, slowly worsening exercise tolerance; chronic productive cough (may be unproductive), typically worse in the morning and after exercise; risk factors, for example, current or prior history of smoking, family history of COPD, childhood respiratory infections, occupational exposure to smoke, fumes, chemicals; may be comorbidities; exacerbations present with fever, subacute increase in dyspnoea, increased sputum production, change in sputum character; severe degree of impairment in young patient or patient with minimal or no smoking history suggests alpha-1 antitrypsin deficiency
Exam
facial plethora, cyanosis, laryngeal height of 4 cm or less, pursed lip breathing, hyper-expanded chest, prolonged exhalation, rhonchi, and wheeze; may be clubbing; severe cases: resting or exercise hypoxaemia; may be pulsus paradoxus, mental state changes
1st investigation
- spirometry:
decreased forced expiratory volume in the first second of expiration (FEV1), decreased FEV1/forced vital capacity (FVC) ratio
More
Congestive heart failure
History
orthopnoea, paroxysmal nocturnal dyspnoea, exertional dyspnoea, dyspnoea may be chronic with acute exacerbations, chest pain, ankle swelling; rapidly progressive failure; dyspnoea dominates the clinical picture
Exam
distended neck veins, fine bibasal rales, displaced apex beat, S3 gallop rhythm, peripheral oedema, may be increased abdominal girth, may be cyanosis and altered mental state
1st investigation
- chest x-ray:
cardiomegaly, bilateral lower lobe shadowing, pleural effusion, enlarged hilar vessels, upper lobe diversion, fluid in horizontal fissure, Kerley B-lines
More - echocardiogram:
valvular heart disease or regional/global wall motion abnormalities
- B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP):
elevated
More
Other investigations
- serum electrolytes:
may be hyponatraemia
- bedside lung ultrasonography:
point of care ultrasound (POCUS) may demonstrate the presence of B-lines
More - ECG:
no specific pattern associated with heart failure exacerbation; Q wave, ST segment depressions, T wave inversion, left bundle branch block, and rhythm changes (atrial fibrillation and flutter) can all be seen
- cardiac enzymes:
may be elevated, as a reflection of myocardial strain and injury
More
Asthma
History
episodic wheezing, cough, chest tightness and dyspnoea, symptom variability - may be seasonal, or following viral infection or exposure to aeroallergen, cool air, or exercise; possible history of other atopic diseases; onset of symptoms normally in childhood
Exam
may be normal in between exacerbations, prolonged expiratory phase, wheeze, and rhonchi; acute severe asthma attack may include: severe breathlessness (including too breathless to complete sentences in one breath), tachypnoea, tachycardia, silent chest, cyanosis, accessory muscle use, altered consciousness or collapse
1st investigation
Other investigations
- bronchial provocation testing:
airway hyper-responsiveness
More - fractional exhaled nitric oxide test (FeNO):
elevated FeNO (≥40 parts per billion) supports the diagnosis of asthma
- FBC:
normal or elevated eosinophils and/or neutrophilia
- immunoassay for allergen-specific IgE:
may be positive for allergen
More - skin prick allergy testing:
may be positive for allergen
More - 6-week trial of inhaled corticosteroids:
symptomatic and objective improvement in response
More
Pneumonia (bacterial, viral, fungal, tuberculous)
History
sudden or sub-acute onset of fever, chills, cough, pleuritic chest pain, and dyspnoea; cough typically produces purulent sputum, but may be dry in some viral pneumonias and early bacterial pneumonia; onset is more insidious in fungal and tuberculous infections; night sweats, weight loss and malaise may occur in tuberculous infection
Exam
fever, tachycardia, tachypnoea, crackles, may be focal chest signs of consolidation: dullness on percussion, asymmetric chest expansion, bronchial breathing; may be signs of effusion: focal decreased breath sounds, and decreased vocal resonance and tactile fremitus; less frequently, jaundice; severe cases: hypoxaemia, cyanosis, altered mental state, and respiratory failure
1st investigation
- chest x-ray:
lobar infiltrate, cavitation, interstitial infiltrates
- sputum Gram stain and culture:
may demonstrate presence of bacteria
More
Other investigations
- FBC:
elevated WBC with/without neutrophilia and left shift may be present
- C-reactive protein:
elevated
More - LFTs:
elevated serum transaminases may be present with atypical pneumonia
More - procalcitonin:
elevated in bacterial pneumonia
More - ABG:
hypoxaemia and respiratory alkalosis may be present in severe pneumonia
- blood cultures:
may be positive for specific organism
More - serum urea or serum urea/serum albumin ratio:
elevated levels of either test predict poor prognosis
More - urinary antigen testing for Legionella and pneumococcus:
positive for Legionella or pneumococcal antigens
More - influenza molecular assay:
positive in influenza
More - respiratory virus PCR:
may be positive for respiratory syncytial virus, human metapneumovirus, adenovirus, rhinovirus, or parainfluenxavirus.
Coronavirus disease 2019 (COVID-19)
History
dyspnoea may be accompanied by dry cough and fever; other common symptoms include anosmia, ageusia, fatigue, anorexia, myalgia, and sore throat; may be a travel history to an affected area or close contact with a suspected or confirmed case in the 14 days prior to symptom onset.
Exam
dyspnoea, may also have fever; patients with pneumonia or respiratory distress syndrome may have inspiratory crackles, rales, and/or bronchial breathing; patients with respiratory distress syndrome may have tachycardia, tachypnoea, or cyanosis accompanying hypoxia
1st investigation
- real-time reverse transcription polymerase chain reaction (RT-PCR):
positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA
More
Other investigations
- ABG:
may show low partial oxygen pressure
More - FBC:
leukopenia; lymphopenia; leukocytosis
More - coagulation screen:
elevated D-dimer; prolonged prothrombin time
More - comprehensive metabolic panel:
elevated liver transaminases; decreased albumin; renal impairment
More - serum procalcitonin:
may be elevated
More - serum C-reactive protein:
may be elevated
More - serum lactate dehydrogenase:
may be elevated
More - blood and sputum cultures:
negative for bacterial infection
More - chest x-ray:
unilateral or bilateral infiltrates
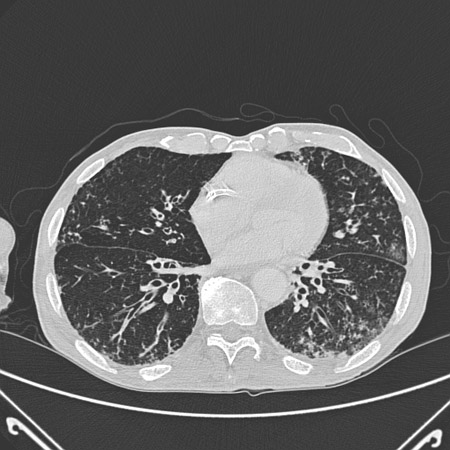
- chest CT:
bilateral ground-glass opacity or consolidation
Croup
History
Sudden-onset ‘seal-like’ barking cough, voice hoarseness; typically affects children aged 6 months to 3 years; symptoms worse at night and when agitated
Exam
Stridor, respiratory distress, sternal and/or intercostal recession; asynchronous chest and abdominal wall movement, fatigue and hypoxia indicate impending respiratory failure
1st investigation
- none:
clinical diagnosis
Other investigations
- x-ray anteroposterior and lateral neck:
steeple sign in anteroposterior view or normal
More
Acute coronary syndrome (ACS)
History
typically presents with central chest pain radiating to shoulders and neck; may cause dyspnoea alone in atypical presentations (especially in women and patients with diabetes); risk factors may be present: smoking, age >45 years (men) or >55 years (women), positive family history of premature coronary artery disease, hypertension, hyperlipidaemia, diabetes, stroke, or peripheral arterial disease
Exam
may be clammy and hypotensive; S3 or S4 gallop rhythm and pulmonary rales may be present
1st investigation
- ECG:
ST elevation (ST-elevation myocardial infarction [STEMI]), T-wave inversion and ST-segment depression (non-ST-elevation myocardial infarction [NSTEMI] and unstable angina); presence of Q waves indicates myocardial injury
More - cardiac enzymes:
elevated troponin I/T, elevated creatine kinase (CK) in STEMI and NSTEMI; not elevated in unstable angina
More - chest x-ray:
normal or signs of heart failure, such as increased alveolar markings
Other investigations
- echocardiogram:
wall motion abnormalities
More - coronary angiography:
STEMI: critical occlusion of a coronary artery; NSTEMI, unstable angina: may be evidence of coronary artery narrowing
Stable angina
History
chest pain from exertion lasting less than 20 minutes, pain not rapidly increasing, relieved by glyceryl trinitrate or rest; may not be associated with dyspnoea; risk factors may be present: smoking, age (men >45, women >55 years), positive family history of premature coronary artery disease, hypertension, hyperlipidaemia, diabetes, stroke, or peripheral arterial disease
Exam
exam may be normal or may have abnormal pulses if peripheral vascular disease present
1st investigation
- ECG:
may be normal/unchanged; may be non-specific ST changes and P-wave flattening; pathological Q waves or left bundle branch block may indicate previous infarction
- cardiac enzymes:
not elevated
Other investigations
- chest x-ray:
normal or cardiomegaly
- stress test:
≥1 mm of horizontal or down-sloping ST-segment depression or ST-segment elevation during or after exercise considered positive for ischaemia; high-risk disease: regional wall motion abnormalities and left ventricular dysfunction
More - coronary angiography:
may be evidence of coronary artery narrowing
- CT coronary angiography:
identification of stenosis
More
Arrhythmias
History
may be sudden-onset weakness, light-headedness, syncope, palpitations; possible history of coronary artery disease or previous arrhythmia
Exam
tachycardia or bradycardia; signs of inadequate cardiac output (pallor, diaphoresis, decreased mental status); peripheral oedema and pulmonary rales may be present
1st investigation
- ECG:
arrhythmia (e.g., atrial fibrillation, atrial flutter, complete heart block)
More
Other investigations
- Holter monitor:
episodic arrhythmia
Interstitial lung disease
History
slowly progressive dyspnoea and a chronic, dry cough; may be risk factors including smoking, rheumatological diseases, exposure to solvents, organic dust, and moulds, chemotherapy and radiotherapy, and certain medications, although many cases are idiopathic
Exam
dry crackles; hypoxaemia, cyanosis, and clubbing may be present
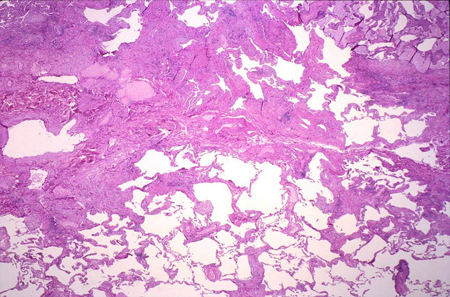
1st investigation
- chest x-ray:
diffuse reticulonodular changes, decreased lung volume
- CT chest:
diffuse reticulonodular changes
More
Other investigations
- lung biopsy:
interstitial pneumonitis
More - pulmonary function tests:
restrictive pattern; isolated reduction in DLCO may be the first sign.
Bronchiectasis
History
chronic cough, chronic daily purulent sputum production, and dyspnoea; possible history of prior pulmonary infections or viral pneumonias in childhood
Exam
prolonged expiratory phase, crackles, rhonchi, and wheeze; clubbing, cyanosis, and hypoxaemia may be present
1st investigation
- high-resolution CT chest:
thickened airways, irregular opacities (predominantly in lower zones), areas of atelectasis, bronchial dilation, tram-tracking, lack of airway size tapering
More - chest x-ray:
thickened airways, irregular opacities (predominantly in lower zones), areas of atelectasis
More - pulmonary function tests:
obstructive ventilatory deficit
Other investigations
Non-infective pneumonitis (eosinophilic, radiation, aspiration, hypersensitivity pneumonitis)
History
fever, chills, cough (dry or productive), and dyspnoea; myalgias, pleuritic chest pain, and night sweats may be present; history of radiation to chest 1 to 6 months before presentation in radiation pneumonitis; episodes of clouded consciousness, choking, and aspiration in aspiration pneumonitis; exposure to organic antigens (e.g., bath tub, birds, hay) in hypersensitivity pneumonitis
Exam
crackles; wheeze and rhonchi less common; hypoxaemia and respiratory failure may be present in severe cases
1st investigation
Other investigations
- pulmonary function test:
Restrictive; mixed restrictive/obstructive
More - bronchoscopic biopsy:
granulomata in hypersensitivity pneumonitis
Acute bronchitis
History
upper respiratory tract symptoms; cough; prolonged coughing and dyspnoea (especially on exposure to cold air, exercise, or irritants) may occur
Exam
fever, cough, inability to take deep breaths ('cough readiness'); lung examination may be normal or reveal rhonchi and wheeze
1st investigation
- none:
clinical diagnosis
More
Other investigations
- chest x-ray:
may be helpful to exclude pneumonia, other causes of cough and fever
Laryngitis
History
upper respiratory tract symptoms; hoarseness; dyspnoea; history of excessive vocal use, e.g., singers
Exam
may be hyperaemia of oropharynx; enlarged tonsils with or without exudate
1st investigation
- none:
clinical diagnosis
More
Other investigations
- laryngoscopy:
oedema and erythema of the vocal folds
Pulmonary embolism (thrombotic, air, amniotic fluid, tumour)
History
sudden-onset dyspnoea and chest pain; may be pre-syncope or syncope, haemoptysis, palpitations, may be asymptomatic; possible history of previous venothromboembolic disease, inadequate anticoagulation, immobilisation, admission to hospital, travel, vascular access, leg injury, malignancy, or childbirth
Exam
tachycardia, tachypnoea, may be hypotension, cyanosis, hypoxaemia, and neck vein engorgement, may present with lower extremity oedema
Other investigations
- ventilation-perfusion (V/Q) scan:
V/Q mismatch
More - ABG:
may show hypoxaemia and hypocapnia
- chest x-ray:
usually normal, but may show peripheral, triangular opacity (Hampton's hump), regional oligaemia (Westermark sign), or enlarged pulmonary artery (Fleischner sign); may also demonstrate a pleural effusion
More - echocardiogram:
right ventricular wall hypokinesis (McConnell's sign) may indicate a major embolus
- ECG:
may show atrial arrhythmias, tachycardia, new right axis deviation, new right bundle branch block, S wave in lead I, Q wave with T-wave inversion in lead III
- serum brain natriuretic peptide (BNP):
may be elevated or normal; insensitive/non-specific for diagnosis; useful for prognosis, may predict a major embolus
More
Pleural effusion
History
symptoms depend on rate of fluid accumulation and fluid volume; pleuritic chest pain and a dull ache may be present
Exam
asymmetrical chest expansion, 'stony' dullness to percussion, decreased tactile fremitus, decreased vocal resonance and absent breath sounds are typical in pleural effusion; examination may be normal in pleural tumours
1st investigation
- chest x-ray:
blunting of costophrenic angle and opacification of lower lung field in pleural effusion; pleural thickening in pleural tumours
More
Other investigations
- bedside ultrasonography:
may demonstrate the presence of hypoechogenic fluid or hyperechogenic pleural tumour
Pleuritis
History
unilateral chest pain significantly exacerbated by deep breathing
Exam
splinting of the chest (i.e., preferential movement of unaffected side) may be present; dullness to percussion and decreased breath sounds may be present on the affected side in the presence of a pleural effusion
1st investigation
Other investigations
Anaemia
History
symptoms depend on severity and acuity of anaemia; presentation ranges from insidious onset of exertional dyspnoea to severe dyspnoea at rest; associated symptoms related to impaired oxygen delivery to tissues (confusion, lethargy, syncope, coma) and compensatory mechanisms (palpitations, bounding pulses) occur
Exam
characterised by nail-bed and conjunctival pallor; jaundice and hepatosplenomegaly may be present in haemolytic anaemia
Other investigations
Gastro-oesophageal reflux disease (GERD)
History
presents with heartburn, overt regurgitation of gastric contents into the throat, and dysphagia; nausea, odynophagia, and chest pain may be present; symptoms are typically post-prandial, occur in supine position, and may be associated with certain foods
Exam
typically normal
1st investigation
Other investigations
- 24-hour pH monitoring:
periods of low oesophageal pH
More
Ascites
History
insidious-onset weight gain and increased abdominal girth; possible history of liver disease (e.g., viral hepatitis, liver cirrhosis) or alcohol misuse
Exam
stigmata of chronic liver disease (e.g., spider naevi, palmar erythema) and jaundice are usually present; abdominal examination reveals abdominal distension and distended abdominal wall superficial veins
1st investigation
- none:
clinical diagnosis
More
Shock
History
possible history of infection/sepsis, anaphylaxis, cardiac pump failure, toxin exposure, or hypovolaemia leading to inadequate tissue perfusion and end-organ dysfunction; may be a history of urinary, respiratory, or intra-abdominal sepsis, exposure to medications and insect bites, cardiac chest pain, or haemorrhage (e.g., haematemesis, melaena)
Exam
hypotension, tachycardia, tachypnoea, and decreased oxygen saturation are common; brain underperfusion causes varying degrees of decreased mental status; pallor or hyperaemia may accompany shock; distributive shock results in warm and flushed extremities; cardiogenic shock leads to cold and clammy extremities; diffuse rash may accompany bacterial toxin production; rhonchi, wheeze, and crackles may be present; abdominal tenderness may reflect an intra-abdominal infectious process or gut ischaemia
1st investigation
- FBC:
elevated or decreased WBC, low haemoglobin
More - serum urea nitrogen:
elevated
More - serum creatinine:
elevated
More - serum bicarbonate:
decreased
More - serum lactate:
elevated
More - ECG:
tachycardia, may be ST-segment and T-wave changes
More - chest x-ray:
may be unilateral infiltrate, signs of pulmonary oedema
More - blood cultures:
may be positive
More
Pulmonary tumours
History
cough; haemoptysis (usually low volume) may be present in proximal airway tumours; chest pain; hoarseness; confusion, focal neurological defects, and bone pain may reflect extrathoracic spread; asymptomatic disease may be incidentally detected by presence of a lung nodule on chest x-ray
Exam
may be normal; may be unilateral wheeze and decreased breath sounds in large airway lesions; crackles and rhonchi may be present in post-obstructive pneumonia; dullness to percussion and decreased fremitus may indicate malignant pleural effusion
Other investigations
- biopsy (bronchoscopic or transthoracic):
lung cancer
More
Anxiety and panic attacks
History
most commonly young to middle-aged women, but may affect both sexes at any age; possible prior history of anxiety, phobias, and panic; dyspnoea may be accompanied by a choking sensation, discomfort in various locations, dizziness, and a sense of fear
Exam
tachycardia, tachypnoea, and sweating may be present; patient may hyperventilate and sigh frequently; Chvostek's and Trousseau's signs may be present
1st investigation
- no initial test:
usually a clinical diagnosis; although, if diagnosis is in doubt, tests may be done to rule out other conditions
Other investigations
- ABG:
respiratory alkalosis
More
Normal ageing, deconditioning, and obesity
History
dyspnoea typically of insidious onset and exertional, and may be associated with undertaking an unusual degree of physical exercise
Exam
typically normal
1st investigation
- none:
clinical diagnosis
More
Other investigations
- exercise testing:
low exercise capacity
Uncommon
Sepsis
History
symptoms of localised infection, non-specific symptoms include fever or shivering, dizziness, nausea and vomiting, muscle pain, feeling confused or disoriented; may be history of risk factors e.g., immunosuppression, pregnancy or postpartum period, frailty, recent surgery or invasive procedures, intravenous drug use or breach of skin integrity
Exam
tachycardia, tachypnoea, hypotension, fever (>38ºC) or hypothermia (<36ºC), prolonged capillary refill, mottled or ashen skin, cyanosis, low oxygen saturation, newly altered mental state, reduced urine output
1st investigation
- blood culture:
may be positive for organism
More - serum lactate:
may be elevated; levels >2 mmol/L (>18 mg/dL) associated with adverse prognosis; even worse prognosis with levels ≥4 mmol/L (≥36 mg/dL)
More - FBC with differential:
WBC count >12 x 10⁹/L (>12,000/microlitre) (leukocytosis); WBC count <4 x 10⁹/L (<4000/microlitre) (leukopenia); or a normal WBC count with >10% immature forms; low platelets
More - C-reactive protein:
elevated
- blood urea and serum electrolytes:
serum electrolytes may be deranged; blood urea may be elevated
- serum creatinine:
may be elevated
More - liver function tests:
may show elevated bilirubin, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, and gamma glutamyl transpeptidase
More - coagulation studies:
may be abnormal
- ABG:
may be hypoxia, hypercapnia, elevated anion gap, metabolic acidosis
Other investigations
- ECG:
may show evidence of ischaemia, atrial fibrillation, or other arrhythmia; may be normal
More - chest x-ray:
may show consolidation; demonstrates position of central venous catheter and tracheal tube
- urine microscopy and culture:
may be positive for nitrites, protein or blood; elevated leukocyte count; positive culture for organism
- lumbar puncture:
may be elevated WBC count, presence of organism on microscopy and positive culture
More - sputum cultures:
may be positive for organism
Aortic dissection
History
typically presents with sudden, severe chest pain that may radiate to the back
Exam
may be normal, may be pallor, tachycardia, tachypnoea, hypotension with increased pulse pressure, and diminished peripheral pulses (especially lower extremities); diastolic precordial murmur suggesting aortic regurgitation may be heard over the precordium
1st investigation
Other investigations
Sarcoidosis
History
frequently diagnosed in asymptomatic stage based on chest x-ray abnormalities; cough, dyspnoea, and chest pain are common; fever, myalgias, subcutaneous nodules, and erythema nodosum may be present
Exam
may be normal; may be wheeze and dry crackles
1st investigation
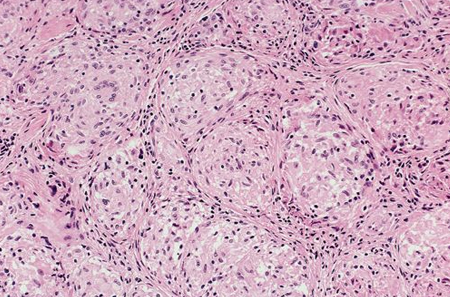
Other investigations
- lung biopsy:
non-caseating granulomata
More
Pulmonary contusion
History
history of blunt or penetrating trauma
Exam
signs of pulmonary oedema
1st investigation
- chest x-ray:
infiltrates, which may be patchy or confluent; pulmonary oedema
Other investigations
- CT of the chest:
infiltrates, pulmonary oedema
- bedside ultrasonography:
may be B-lines and C-lines
More
Epiglottitis
History
commonly in young children (aged 3-5 years), but may occur at any age; rapidly progressive sore throat, fever, odynophagia, dysphonia, drooling, hoarseness and stridor
Exam
child typically adopts the 'tripod' position (postures neck and head anteriorly and places hands on his/her knees); anterior oral examination may be normal; tenderness over anterior and lateral neck and hyoid bone, swelling on laryngoscopy; note: direct airway examination may precipitate airway obstruction
1st investigation
- none:
clinical diagnosis
More
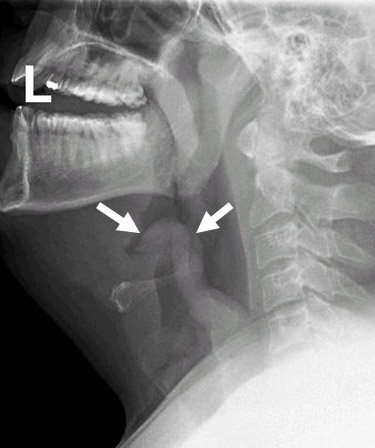
Other investigations
- lateral neck x-ray:
enlarged epiglottis - the 'thumb sign'[Figure caption and citation for the preceding image starts]: Lateral neck film demonstrating thumbprint sign (arrows)From the collection of Dr Petri [Citation ends].
- laryngoscopy:
swollen epiglottis, aryepiglottic folds, and arytenoid cartilages
Anaphylaxis
History
history of exposure of predisposed host to a medication, food product, or insect sting or bite; sudden dyspnoea and wheezing, choking sensation, voice changes, tongue swelling, rash, and itching; nausea, vomiting, and diarrhoea may be present
Exam
prolonged expiratory phase, wheeze, tachycardia, hypotension, facial and tongue oedema, cutaneous manifestations (urticaria, angio-oedema)
1st investigation
- none:
clinical diagnosis
Other investigations
- serum tryptase:
usually elevated
More
Angio-oedema
History
rapid development of skin or mucosal surface swelling; lips, mouth, larynx, and bowel most commonly involved; possible history of atopic diseases or ACE inhibitor use; dyspnoea may be present if larynx is involved
Exam
asymmetrical, prominent swelling of the involved part; urticaria may be present; respiratory compromise may be present if larynx is involved
1st investigation
- none:
clinical diagnosis
Other investigations
- complement studies:
C4 reduced in acquired angio-oedema; C1-esterase inhibitor reduced in hereditary angio-oedema; C1q normal in hereditary angio-oedema and reduced in acquired angio-oedema
More
Foreign body aspiration
History
possible history of epilepsy, syncope, altered mental status (e.g., intoxication, hypoglycaemia), or choking and coughing after ingestion of food (particularly nuts); history of choking not always present; may have had recurrent pneumonia
Exam
cyanosis, stridor, unilateral wheeze
1st investigation
- chest x-ray:
unilateral atelectasis or hyperlucency
More - CT chest:
foreign body in airways
Other investigations
- bronchoscopy:
presence of foreign body
More
Tracheobronchial tumours (benign or malignant)
History
dyspnoea may be constant or positional; cough (usually dry) and haemoptysis may be present; airway obstruction may lead to pneumonia, which markedly exacerbates symptoms
Exam
may be wheeze and stridor; hypoxaemia is a late finding
Other investigations
- bronchoscopy:
tracheal tumour
More
Retrosternal goitre
History
dyspnoea and wheezing are common; cough may be present; symptoms may be positional; chest pain, hoarseness, and Horner syndrome are less common; enlargement of ectopic thyroid tissue is accompanied by enlargement of orthotopic thyroid; may be history of orthotopic thyroid removal
Exam
goitre typically present; may be stridor, dyspnoea, and wheeze (especially with forced respiration); Pemberton manoeuvre (passive elevation of arms above head for 1 minute) may reveal symptoms by forcing thyroid tissue into the thoracic inlet
1st investigation
Other investigations
- spirometry:
flattened inspiratory and expiratory portions of flow-volume loop
Vocal cord dysfunction
History
exertional dyspnoea that may be associated with wheezing and stridor; symptoms may appear only in certain positions and are typically associated with a degree of anxiety
Exam
examination may be normal; forced exhalation or series of deep breaths may induce wheezing/stridorous sound
1st investigation
Other investigations
Pulmonary hypertension
History
insidious onset resulting in limitation of exercise capacity; exertional chest pain, exertional syncope, and symptoms of right-sided heart failure may develop
Exam
increased intensity of pulmonary component of S2 may be the only sign; distended neck veins, hepatomegaly, and peripheral oedema may be present in severe cases
1st investigation
- echocardiogram:
elevated estimated pulmonary artery pressure, right ventricular strain
Other investigations
- right heart catheterisation:
elevated pulmonary artery pressure
More
Hepatopulmonary syndrome
History
typical presentation includes dyspnoea; platypnoea (dyspnoea that is relieved on lying down) may be present; history of chronic liver disease
Exam
hypoxaemia with platypnoea-orthodeoxia (i.e., dyspnoea and hypoxia in upright position that improves in recumbent position) is typical; stigmata of chronic liver disease (e.g., spider naevi), jaundice, and ascites may be present
1st investigation
- ABG:
hypoxaemia
- contrast echocardiography:
extracardiac shunt
More
Other investigations
Pulmonary arteriovenous malformations
History
most commonly a manifestation of autosomal dominant hereditary haemorrhagic telangiectasia (HHT), but may be isolated; epistaxis, haemoptysis, dyspnoea, and gastrointestinal bleeding; large malformations associated with platypnoea (dyspnoea that is relieved on lying down)
Exam
small, red, elevated vascular malformations of the skin and mucous membranes are typical of HHT; hypoxaemia may be present; examination may be normal in isolated, non-HHT-related malformations
1st investigation
Other investigations
- technetium-macroaggregated albumin scintigraphy:
may show extracardiac shunting with abnormal peripheral accumulation of aggregates
Pulmonary veno-occlusive disease
History
slowly progressive dyspnoea that may be accompanied by chronic cough, chest pain, abdominal pain, or syncope
Exam
cyanosis, clubbing, loud P2, right ventricular heave, liver congestion, peripheral oedema
1st investigation
- chest x-ray:
prominent pulmonary arteries, Kerley B-lines, pleural effusions
Other investigations
- CT chest:
demonstrates mosaic ground glass opacities, centrilobular infiltrates, and pleural effusions; right heart catheterisation shows elevated pulmonary artery pressures but normal capillary wedge pressure
Mesothelioma
History
asbestos exposure, often employment-related, with a latency period of 20 to 40 years; shortness of breath, dry non-productive cough, chest pain; non-specific symptoms (such as fatigue, fever, sweats, and weight loss) also common
Exam
decreased breath sounds and dullness to percussion on the affected side as a result of pleural effusion or bronchial obstruction on the affected side
1st investigation
Other investigations
Pneumothorax and pneumomediastinum
History
sudden-onset dyspnoea and unilateral chest pain; patient may be tall and asthenic; possible history of crack cocaine use, HIV, or lymphangioleiomyomatosis
Exam
unilaterally absent breath sounds and tympany on percussion of ipsilateral chest in pneumothorax; tracheal shift away from side of lesion in tension pneumothorax; subcutaneous emphysema in pneumomediastinum
1st investigation
Other investigations
Haemothorax
History
history of blunt or penetrating trauma to the chest
Exam
signs of volume depletion, circulatory collapse, and shock
1st investigation
- chest x-ray:
fluid in the pleural space with blunting costophrenic angle
More
Other investigations
- bedside ultrasonography:
POCUS may identify hyperechogenic fluid within the pleural space, suggestive of haemothorax
Acquired valvular heart disease
History
dyspnoea on exertion, episodic chest pain, symptoms of congestive heart failure (weight gain, orthopnoea, paroxysmal nocturnal dyspnoea, ankle swelling); possible history of rheumatic fever; acute valvular dysfunction may follow a coronary event
Exam
murmur reflecting turbulence due to flow through a narrowed valve or regurgitation of blood; jugular venous distension, heart rhythm disturbances (especially atrial fibrillation), peripheral oedema, and hepatomegaly may be present
1st investigation
- echocardiogram with Doppler:
valvular insufficiency or stenosis
More
Other investigations
- chest x-ray:
enlarged heart chambers
More
Congenital heart disease
History
may be detected in newborn period, although may present at a later age; impaired exercise tolerance; chest pain, hypertension, and exertional syncope may be present; infrequently may present with consequences of intracardiac shunt (e.g., brain abscesses)
Exam
patent ductus arteriosus is characterised by wide pulse pressure, palpable, dynamic left apical impulse with a continuous machinery-like murmur; aortic coarctation is characterised by absent lower extremity pulses with hypertension in the upper extremities; tetralogy of Fallot is characterised by systolic murmur, absent P2, and cyanosis; cyanosis may be present in Eisenmenger's syndrome
1st investigation
- echocardiogram with Doppler:
abnormality specific to underlying defect
More
Other investigations
- chest x-ray:
enlargement of heart chambers, pulmonary vascular congestion
More
Cardiac drugs
Myocardial disease (cardiomyopathy, myocarditis)
History
fatigue and decreased exercise tolerance; symptoms of heart failure (ankle swelling, increased abdominal girth, orthopnoea, paroxysmal nocturnal dyspnoea, chest pain) may be present; myocarditis frequently follows a viral infection; cardiomyopathy may be incidentally detected on chest x-ray
Exam
tachycardia, S3 or S4 gallop rhythm, systolic murmur of mitral or tricuspid regurgitation, neck vein distension, peripheral oedema, ascites, and hepatomegaly may be present
1st investigation
Other investigations
Pericardial disease
History
chest pain; dyspnoea is typically ameliorated by assuming a sitting position and bending forwards; ankle swelling and increased abdominal girth may be the presenting symptoms; patients with constrictive pericarditis may have a history of chest surgery or chest radiation
Exam
tachycardia, distended neck veins, pulsus paradoxus (>10 mmHg decrease in systolic blood pressure with inspiration), peripheral oedema, ascites, pulsatile hepatomegaly, and pleural effusion may be present; pericardial friction rub is best heard over the left sternal border with the patient leaning forwards at end-expiration; distant heart sounds
1st investigation
Other investigations
- chest x-ray:
enlarged cardiac silhouette in pericardial effusion/cyst/tamponade; small heart in constrictive pericarditis
Superior vena cava syndrome
History
insidious-onset dyspnoea, facial oedema, and head fullness
Exam
facial plethora, distension of neck and head veins[Figure caption and citation for the preceding image starts]: Prominent collateral vein on the anterior chest and abdominal wall in a patient with superior vena cava syndrome.From the collection of E Kempny. Reproduced under the Creative Commons CC BY-SA 4.0 license (https://creativecommons.org/licenses/by-sa/4.0/) [Citation ends].
1st investigation
- chest x-ray:
paramediastinal mass
More
Other investigations
- CT angiogram:
superior vena cava narrowing
More
Methaemoglobinaemia and carbon monoxide poisoning
History
methaemoglobinaemia presents with easy fatigability and headaches; symptoms may progress to obtundation, respiratory depression, and death in severe cases; symptoms may appear after exposure to specific drugs, either by ingestion (dapsone) or mucosal exposure (lidocaine, benzocaine); carbon monoxide poisoning may mimic a viral syndrome (headache, malaise, dizziness, nausea)
Exam
cyanosis, dyspnoea, and neurological changes may be present in methaemoglobinaemia; arrhythmias and mental status changes ranging from mild confusion to seizures and coma are common in carbon monoxide poisoning; cherry-red appearance of skin may be noted in carbon monoxide poisoning
1st investigation
Other investigations
Tetanus
History
history of exposure to Clostridium tetani spores through injury, foreign body retention, or in neonatal period; presentation ranges from localised muscle spasms of a limb to tonic, painful skeletal muscle contractions in severe cases; prodrome of restlessness, sweating, and tachycardia may be present; tetanic spasms may affect any muscle group and be triggered by non-specific stimuli (e.g., light, noise)
Exam
contraction of facial muscles results in lockjaw (trismus) or a sardonic smile (risus sardonicus); contraction of back muscles leads to opisthotonus; abdominal muscle contraction raises suspicion of a surgical abdomen
1st investigation
- none:
clinical diagnosis
Botulism
History
acute onset of bilateral bulbar neuropathy with symmetrical descending weakness; possible history of ingestion of contaminated, non-pasteurised food (food-borne botulism) 12 hours to 7 days before symptom onset, or wound contamination with Clostridium botulinum; nausea, vomiting, abdominal cramps, and diarrhoea may accompany blurred vision, diplopia, and facial paralysis
Exam
any cranial nerve may be involved, resulting in blurred vision, ophthalmoplegia, diplopia, dysarthria, nystagmus, ptosis, and facial weakness
1st investigation
- none:
clinical diagnosis
More
Phrenic nerve paralysis
History
recent surgical procedure, involving neck or chest, recent chest or neck trauma; in idiopathic cases, no such history can be elicited
Exam
dullness to percussion at lung base, no respiratory variability of the lower lung border
1st investigation
- chest x-ray:
elevated, relaxed hemidiaphragm
Other investigations
- dynamic chest fluoroscopy ('sniff test'):
paradoxical (upward) movement of the affected diaphragm
Amyotrophic lateral sclerosis
History
asymmetrical weakness of the distal muscles, inability to perform fine motor hand movements, or foot drop; possible difficulty in initiating movements and maintaining erect posture; personality changes may be noted by family members
Exam
signs attributable to upper and lower motor neuron disease (weakness, hyper-reflexia, spasticity, muscle atrophy, fasciculations) and bulbar involvement (dysphagia, dysarthria) may be present; drooling and sialorrhoea may be present; patients may display inappropriate affect with laughing, crying, and impaired judgement
1st investigation
- none:
clinical diagnosis
More
Other investigations
- electromyography:
acute and chronic denervation, fasciculation potentials
- nerve conduction studies:
normal
More
Polio and other acute viral anterior horn infections
History
polio presents with asymmetrical weakness (typically affects lower more than upper extremities and proximal more than distal muscles) and diminished deep tendon reflexes; neurological symptoms may be preceded by a viral prodrome of fever, nausea, malaise, and sore throat; muscle weakness quickly progresses and may lead to quadriplegia and respiratory failure; other infections of anterior horn cells (e.g., enteroviruses, West Nile virus) produce similar symptoms
Exam
asymmetrical muscle paresis or paralysis; sensory examination is typically normal; deep tendon reflexes are diminished
1st investigation
Other investigations
Guillain-Barre syndrome
History
progressive symmetrical paralysis; muscle weakness typically starts in thigh muscles, but may involve any muscle group (e.g., arms, bulbar, ocular); patients may experience sensory phenomena (especially paraesthesias in hands and feet); urinary retention and ileus may be present
Exam
symmetrical muscle weakness is a hallmark sign; dysautonomia (tachycardia or bradycardia, labile blood pressure, orthostatic hypotension) may be present; deep tendon reflexes are characteristically absent or diminished
1st investigation
- lumbar puncture:
elevated protein level, normal pleocytosis
- nerve conduction studies:
conduction velocity slowing, patchy demyelination
More
Other investigations
Myasthenia gravis
History
muscular weakness of ocular or bulbar muscles; ptosis, diplopia, dysarthria, and dysphagia are common; muscle fatigability involving facial or limb muscles is less common
Exam
examination is variable; weakness of extra-ocular muscles (not restricted to specific cranial nerve), lack of facial expression, or peripheral muscle weakness and fatigability (typically affects arms more than legs) may be present; speech may be weak or indistinct
1st investigation
Other investigations
- serum antibodies to tyrosine kinase receptor:
positive
More
Respiratory muscle deficiency
History
onset of dyspnoea may be insidious (idiopathic diaphragmatic paralysis), or related to a known insult (e.g., trauma, surgery); dyspnoea typically worse in supine than upright position (orthopnoea) in diaphragmatic paralysis
Exam
detecting paradoxical diaphragm movement may be difficult; abdominal wall muscle weakness is easily detected by paradoxical, inward movement of abdominal wall during inspiration; weakness of non-respiratory muscles may be evident in paraparesis
1st investigation
Other investigations
Paraneoplastic myasthenic syndrome
History
weakness in pelvic girdle and ascending pattern of motor disease progression; difficulty in getting up from a chair, easy fatigability, and muscle cramps; weakness improves transiently after brief exercise (post-exercise facilitation); autonomic dysfunction (erectile dysfunction, mouth dryness) may be present; weakness of upper girdle muscles and involvement of ocular and bulbar muscles is less common
Exam
predominantly lower-extremity weakness with absent reflexes; proximal muscles most commonly affected; symmetrical distribution of muscle involvement; no oculobulbar involvement
1st investigation
- antibodies to voltage-gated calcium channel:
positive
More - electrophysiology testing:
characteristic pattern of pre-synaptic neuromuscular junction disorder
Other investigations
Thyroid disease
History
thyrotoxicosis presents with dyspnoea, decreased exercise tolerance, sweating, heat intolerance, fatigue, diarrhoea, urinary frequency, and weight loss; hypothyroidism and associated slowing of metabolism manifests with cold intolerance, constipation, and weight gain; women with hypothyroidism may experience oligomenorrhoea or amenorrhoea; snoring may appear or worsen with the development of hypothyroidism
Exam
signs of thyrotoxicosis include tachycardia (e.g., atrial fibrillation), tachypnoea, widened pulse pressure, warm and sweaty skin, exophthalmos, lid lag, and neck goitre; anxiety, restlessness, and agitation may also be present; signs of hypothyroidism include dry skin, generalised oedema, hypertension, and mental slowing
1st investigation
- serum thyroid-stimulating hormone (TSH):
elevated in hypothyroidism, decreased in hyperthyroidism
More
Other investigations
- serum free T3 and free T4:
elevated in hyperthyroidism, decreased in hypothyroidism
Cushing syndrome
History
progressive weight gain and exertional dyspnoea; careful history localises decreased exercise tolerance to muscle weakness; women may present with oligomenorrhoea or amenorrhoea
Exam
obesity with central distribution, moon facies, supraclavicular and nuchal fat pads; skin is thin and easily bruised; striae may be evident over the trunk and extremities; female patients may display hirsutism; hypertension may be present
1st investigation
- urinary cortisol:
elevated
More
Other investigations
- low-dose dexamethasone suppression test:
lack of cortisol production suppression
More
Phaeochromocytoma
History
episodic sweating, headache, and tachycardia; possible associated episodic dyspnoea and feelings of panic
Exam
examination between paroxysms of catecholamine release may be normal; some patients have sustained hypertension
1st investigation
- 24-hour urinary metanephrine and catecholamine collection:
elevated
More
Other investigations
Kyphoscoliosis and pectus excavatum
History
pectus excavatum develops in early childhood and may cause exertional dyspnoea; kyphoscoliosis develops in childhood or adolescence and is most commonly idiopathic or may be caused by neuromuscular disease, vertebral body destruction, or connective tissue disorders
Exam
pectus excavatum is characterised by lower sternum concavity and mild restriction to chest expansion, and has associated scoliosis in up to 15% of cases; kyphoscoliosis is characterised by anterior and lateral spinal deformation; degree of scoliosis and kyphosis may be under-appreciated due to compensatory changes in other bony structures
1st investigation
- spinal x-ray:
abnormal curvature of spine or sternum
More
Other investigations
Diphtheria
History
upper respiratory tract symptoms; dysphagia, dysphonia, dyspnoea, and a croupy cough can develop; immunisation and travel history are important
Exam
typical brown-grayish pseudomembrane may be seen on the tonsils and/or pharynx
1st investigation
- bacteriological culture and microscopy:
black colonies with halos on Tindale media, metachromatic granules on Loeffler media, irregular staining pleomorphic bacilli on microscopy
Other investigations
Use of this content is subject to our disclaimer