Approach
The diagnostic approach follows the pattern of history, examination, and radiological evaluation. Emergency surgical consultation is appropriate before obtaining any diagnostic studies if midgut volvulus is suspected, as emergency surgical exploration without pre-operative studies may be warranted if peritonitis is present or a gas-less abdomen is seen on abdominal x-ray. If the patient appears stable, an urgent upper gastrointestinal (GI) contrast study should be performed to identify the patient who will need an operation for malrotation and/or midgut volvulus. If the history and physical findings are more suggestive of bowel ischaemia/necrosis (e.g., peritonitis), which may occur with midgut volvulus, then immediate surgical intervention is performed without radiological investigation in order to expedite diagnosis and reversal of ischaemia.
History
Of patients with malrotation who become symptomatic, 50% to 75% do so in the first month and about 90% within the first year of life.[2]
The presence of bilious (dark green) emesis is the key factor in immediately alerting the carer to consider the possibility of midgut volvulus. Bilious vomiting should be considered to have a surgical cause until proved otherwise; prompt discussion with a paediatric surgical team is advised in this situation, to ensure appropriate referral, investigation and treatment.[11] Therefore, any patient without previous abdominal surgery and/or an upper GI contrast study showing normal rotation, who has a history of green vomiting, should undergo emergency investigation to rule out midgut volvulus.
In the presence of malrotation with midgut volvulus, the vomiting is often sudden in onset and can be associated with severe abdominal pain. Carers of infants may give a history of the child becoming inconsolable for a period of time. Abdominal pain may be out of proportion to physical findings. However, history or duration of abdominal pain can otherwise be challenging to elicit in infants and young children, who account for most of the patients with symptomatic malrotation.
More subtle and chronic symptoms are frequently found in malrotation patients without volvulus. Moreover, patients may be asymptomatic and are discovered to have malrotation incidentally on work-up of other unrelated conditions.
Some less common congenital anomalies can be found with various degrees of malrotation (i.e., gastroschisis, omphalocoele, congenital diaphragmatic hernia, and heterotaxy). The presence of heterotaxy adds another layer of complexity to the variation of malrotation patterns. Although a high percentage of these patients have some element of malrotation, the risk of volvulus is still evident, albeit lower than with classic incomplete rotation.
The carer may also see dark blood in the nappy.
Physical examination
Abdominal exam findings can vary substantially depending on the presence and duration of midgut volvulus. Without volvulus, the exam is frequently benign and history is more elaborative. Early in the setting of midgut volvulus, the exam may demonstrate only minimal or no tenderness and no distention, as the initial point of bowel obstruction is in the duodenum. Later during midgut volvulus, examination can reveal a more worrying and obvious presentation of abdominal distention, peritoneal signs, and septic shock with tachycardia and tachypnoea. These are ominous signs of ongoing intestinal ischaemia/infarction.
Summary of clinical findings
Features of obstruction with ischaemia (midgut volvulus with vascular compromise) include:
Bilious vomiting
Acutely ill patient with severe abdominal pain
Abdominal tenderness
Signs of peritoneal catastrophe (distension and guarding)
Tachycardia
Acidosis
Tachypnoea
Features of obstruction without ischaemia (midgut volvulus without vascular compromise) include:
Bilious vomiting
Crampy abdominal pain in waves
Non-tender abdomen
Non-distended abdomen
No severe physiological perturbation
Features of intermittent or partial volvulus or obstructing Ladd's bands include:
Intermittent vomiting
No signs of acute illness
Intermittent abdominal pain (typically post-prandial)
Weight loss
Features of questionable malrotation or asymptomatic/incidental findings in investigating for reflux (fussiness, arching, apnoeic events, reactive airways, pneumonia) include:
Intermittent vomiting
No signs of acute illness
Radiological evaluation
Upper GI contrast series
This is the diagnostic standard for malrotation with or without midgut volvulus and must include anteroposterior and lateral projections.[12][13]
In normal rotation, the duodeno-jejunal junction at the ligament of Treitz is located to the left of the left vertebral pedicle and is at the approximate height of the pylorus.
In malrotation, the duodeno-jejunal junction is located to the right of the spine and inferior to the level of the pylorus, with a more anterior projection than normal.
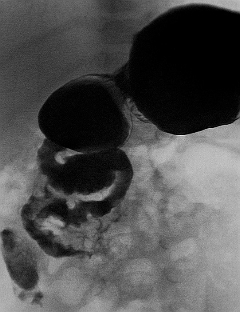
In midgut volvulus there may be a bird's beak cut-off of contrast in the second portion of the duodenum, or the duodenum may have a corkscrew appearance if contrast can get into the loops of bowel that have twisted.[Figure caption and citation for the preceding image starts]: Malrotation with volvulus without obstruction as seen on upper GI contrastFrom the collection of Dr S.D. St Peter [Citation ends].
The typical sensitivity is approximately 95%, but it may have a false-positive rate of up to 15% and false-negative rate of up to 6%.[13][14][15]
Abdominal plain x-rays
This study is usually ordered as a preliminary investigation for patients presenting with abdominal complaints. It is infrequently helpful in preventing other more definitive tests to rule out malrotation unless other conditions are highly suspected (e.g., necrotising enterocolitis or congenital duodenal obstruction).
Stomach and proximal duodenum distended with gas and little distal gas is the most consistent sign of volvulus on plain x-rays.[16]
The build-up of air in the stomach and proximal duodenum during volvulus gives the double-bubble appearance that is pathognomonic for duodenal atresia. However, if any air is present distally, malrotation with volvulus is suggested and an emergency contrast study should be performed.
A normal abdominal radiograph does not exclude the diagnosis of malrotation.[12]
Lower GI contrast series
This study may be ordered in the work-up of newborn patients with stooling difficulty or distal intestinal obstruction.[12]
Malrotation may be suspected by abnormal position of the caecum (present in 85%).[17]
If there is any concern of GI obstruction, the abnormal caecal position should prompt upper GI contrast study.
Rarely, lower GI series may augment the investigation for malrotation if the upper GI series is inconclusive.[17]
Ultrasound
This study can be done quickly without contrast or radiation, but if midgut volvulus is a concern, it may be clinically misguided to order an ultrasound.[12] An ultrasound is more commonly ordered to assess for intussusception if malrotation or midgut volvulus is not the primary consideration. However, when it is ordered to rule out intussusception, or in circumstances where the upper GI series is not conclusive, images of the mesenteric vessels may be useful, demonstrating a reversed SMA-SMV relationship or even a 'whirlpool' pattern of volvulus.[12] One meta-analysis and narrative review focused on the role of ultrasound to diagnose, or exclude, malrotation/volvulus. A careful protocol with visualisation of the course of the duodenum, as well as the relationship of the SMA/SMV, may improve diagnostic accuracy for midgut malrotation in children.[18][19]
The meta-analysis also reported a high summary sensitivity and specificity of 94% and 100%, respectively, for the use of ultrasound in diagnosing malrotation with or without midgut volvulus.[19]
Computed tomography (with oral and intravenous contrast)
CT scan is not the preferred study to assess for malrotation and/or midgut volvulus; however, when this study is performed to assess abdominal pain without bilious emesis, malrotation and/or midgut volvulus may be seen.
In the setting of volvulus, CT scan of the abdomen could potentially show oral contrast cutting off at the duodenum, and intravenous contrast may show a twirling of the superior mesenteric artery (SMA) and superior mesenteric vein (SMV). The image of the vessels may depict whether there is good arterial flow beyond the point of twisting.
In the setting of malrotation without volvulus, findings would be similar to those of the upper GI series. Furthermore, an abnormal orientation of the SMA and SMV may be noted, with the SMA located to the right and anterior to the SMV.
CT allows the detection of asymptomatic intestinal malrotation, facilitating diagnostic precision and enabling classification of intestinal malrotation that would help with identifying high-risk patients.[20]
Laboratory evaluation
Blood gas analysis (including lactate)
When bowel perfusion is compromised from twisting of the mesenteric vessels, lactic acidosis ensues dropping the serum pH with increased anion gap.
If the diagnosis of volvulus is confirmed with radiological studies, blood gas analysis is important to determine the physiological status of the patient and to guide resuscitation.
Clotting, group and save, or cross-match
Required if surgery is anticipated.[21]
Urea and electrolytes
Non-specific for diagnosis.
Patients with volvulus and resultant bowel ischaemia can develop severe metabolic derangements.
Hypochloraemia and hypokalaemia can be associated with persistent obstruction associated with nausea and vomiting.
May indicate degree of volume depletion that is secondary to the obstruction.
Full blood count
Typically required if surgery is anticipated.[21]
C-reactive protein
Likely to be raised in the presence of volvulus, particularly if ischaemia or necrosis is present.[22][23]
As volvulus is a time-critical emergency, patients in some circumstances may need to proceed directly to laparotomy while blood test results are still being awaited.
Use of this content is subject to our disclaimer