Approach
Diagnosis of hiatus hernia may be inferred through careful history and examination. It is important to stress that an unknown number of all patients with hiatus hernia (perhaps representing the majority) have minimal to no symptoms.
Signs and symptoms that might be elicited on a history and physical examination are mostly non-specific and can only suggest the presence of a hiatus hernia. The diagnosis of hiatus hernia primarily is established through the use of diagnostic testing, including:[1]
Chest x-ray
Upper gastrointestinal fluoroscopy with oral contrast
Oesophago-gastro-duodenoscopy
Computed tomography (CT) scan or magnetic resonance imaging (MRI).
Clinical history
Typical complaints from a patient with a symptomatic hiatus hernia might include: heartburn, reflux of sour liquid material (water brash), dull retrosternal chest pain (especially associated with swallowing), dysphagia, and crampy pain associated with swallowing (odynophagia).[6] Other symptoms may include vomiting undigested food, haematemesis, early satiety, bloating, hoarseness, and wheezing/dyspnoea.
None of these symptoms are pathognomonic for hiatus hernia; they are nonspecific, and may be associated with other diseases. Some of these symptoms may be exacerbated by bending over, assuming a recumbent position, physical exertion, or any manoeuver which increases intra-abdominal pressure. It is not possible to determine the type (I, II, III, or IV) of hiatus hernia using history and physical examination.
The patient presenting with a complicated hiatus hernia (involving obstruction, bleeding, and/or ischaemia) may have the following symptoms:
severe chest pain
non-bilious vomiting
haematemesis (>50 cc)
dyspnoea
fevers and chills
confusion
some, or all, of the complaints elicited with uncomplicated hiatus hernia.
Physical examination
Physical examination in a uncomplicated hiatus hernia also is non-specific; findings which may suggest the presence of a hiatus hernia include:
Oropharyngitis (secondary to reflux of gastric contents)
Wheezing (secondary to aspiration of refluxate)
Decreased left chest breath sounds
Dullness to thoracic percussion
Presence of bowel sounds in the left chest.
Physical examination in a complicated hiatus hernia may reveal the following:
Pyrexia
Tachycardia
Hypotension
Tachypnoea
Altered mental status
Some, or all, of the signs elicited with uncomplicated hiatus hernia.
Primary investigation
It is imperative that overuse of diagnostic modalities does not occur in these patients, as delay in treatment is associated with poor outcomes.[1]
A chest x-ray is a simple and inexpensive test and is indicated as the first test in all symptomatic patients.[1] Patients with hiatus hernia may have a retrocardiac air bubble in the intrathoracic portion of the stomach.
An upper gastrointestinal fluoroscopy with oral contrast is the key test for hiatus hernia, as it will delineate the anatomy and provide a qualitative assessment of oesophageal motility.[17][18] It is indicated as a primary test in patients with moderate or severe symptoms. Fluoroscopy may be performed with a barium oesophagram, but an upper gastrointestinal series evaluation is recommended if the hernia is large for a complete assessment of the stomach.[17][Figure caption and citation for the preceding image starts]: Type IV para-oesophageal hiatus hernia: (A) Frontal chest x-ray revealing a large intrathoracic gastric bubble (arrows); (B) Air-fluid level confirming intrathoracic gastric contents on the right lateral decubitus chest x-ray (arrow)BMJ Case Reports 2009 (doi:10.1136/bcr.06.2008.0302); copyright@2009 by the BMJ Publishing Group [Citation ends].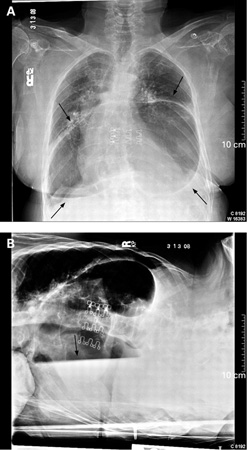
Subsequent tests
Endoscopy
Patients with moderate-to-severe reflux symptoms should undergo endoscopy to check for the presence of oesophagitis and/or oesophageal dysplasia; this information can help the clinician decide which therapy to pursue.[6] An oesophago-gastro-duodenoscopy also can provide information on the anatomy of the hiatus hernia, although endoscopic anatomy can sometimes be misleading.
CT or MRI
CT scan or MRI is indicated when the diagnosis is not clear, other pathology is suspected, or when planning surgical intervention.[1] These investigations provide 3-dimensional reconstruction of the anatomy and thus determine whether organs other than the stomach have migrated into the chest.
Oesophageal manometry and pH monitoring
Oesophageal manometry and pH monitoring are indicated in patients with hiatus hernia and atypical symptoms, dysphagia, and/or when additional confirmation of the diagnosis is required.[19] A typical double hump pattern is seen on manometry. High resolution manometry (HRM) should be utilised as it can demonstrate various anatomical landmarks, such as the level of the diaphragmatic crura or the location of the lower oesophageal sphincter. Calculating the size of a sliding component of a hiatus hernia is also possible with HRM.[1]
Abnormal pH monitoring results are seen with larger hiatus hernias. While this is not a necessary investigation for the diagnosis of hiatus hernia, it is useful when evaluating the need for anti-reflux surgery in addition to hernia repair.[1][20]
Use of this content is subject to our disclaimer