History and exam
Key diagnostic factors
common
weight loss
Found in infants with salt-wasting congenital adrenal hyperplasia.
failure to thrive
Found in infants with salt-wasting congenital adrenal hyperplasia.
vomiting
Found in infants with salt-wasting congenital adrenal hyperplasia.
hypotension
Found in infants with salt-wasting congenital adrenal hyperplasia.
atypical genitalia
In classical 21-hydroxylase deficiency, 46,XX infants may have an enlarged clitoris, fused labia, and a urogenital sinus (classical form). Degree of virilisation in females can be graded based on the Prader score. [Figure caption and citation for the preceding image starts]: Prader Score: degree of virilisation of the external genitalia of females as proposed by Prader. In type I, the only abnormality is a slight enlargement of the clitoris. In type V, there is a markedly enlarged phallus with a penile urethraPermission granted by Helvetica Paediatrica Acta [Citation ends].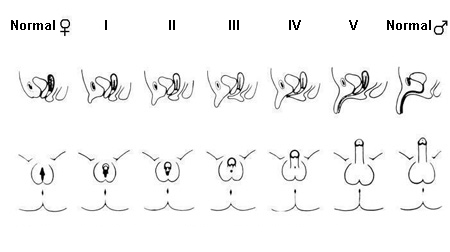
46,XY infants may have scrotal hyperpigmentation. Discordant pubertal exam and increased phallic size despite pre-pubertal testicular volume, may be noted in males with congenital adrenal hyperplasia during childhood.
hyperpigmentation
Genital hyperpigmentation may be the only presenting sign in newborn males with classical simple virilising form.
Other diagnostic factors
common
short stature
Occurring during childhood, elevated adrenal androgens, through conversion to oestrogens, promote the early fusion of epiphyseal growth plates. It is common (but not universal) that children with congenital adrenal hyperplasia have advanced bone age and accelerated linear growth velocity. As a result, these patients are often tall initially, but shorter than mid-parental target height.[18][19]
precocious puberty
Overproduction of adrenal androgens may lead to early development of pubic hair, axillary hair; and/or adult odour. Untreated or undertreated congenital adrenal hyperplasia can also cause early maturation of the hypothalamic-pituitary-gonadal axis and lead to central precocious puberty, which is clinically noted with testicular enlargement in boys and breast development in girls.
irregular menses
There is usually a medical history of irregular menses or complete absence of menstruation.
infertility
Usually diagnosed when a couple is trying to conceive. Genetic analysis is recommended. May occur in both adult males and adult females.
male-pattern baldness (females)
A sign of hyperandrogenism seen in untreated non-classical congenital adrenal hyperplasia or poorly controlled classical disease.[Figure caption and citation for the preceding image starts]: Male-pattern baldness typical of females affected with non-classical 21-hydroxylase deficiencyPermission granted by The Endocrine Society [Citation ends].
polycystic ovaries
Females with non-classical congenital adrenal hyperplasia may develop polycystic ovaries.
hirsutism
Excessive and increased hair growth in women, in a male-type of body distribution (i.e., upper lip, sideburns, mid-line abdomen).
uncommon
acne
May be severe cystic acne and involve multiple regions (i.e., face, back, and chest). [Figure caption and citation for the preceding image starts]: Skin before and after treatment with dexamethasone for 3 monthsPermission granted by The Endocrine Society [Citation ends].
Risk factors
strong
genetic predisposition
Congenital adrenal hyperplasia is an autosomal recessive disorder, caused by gene mutations which affect the enzymes involved in adrenal corticosteroid synthesis. Most cases are caused by a defect of the 21-hydroxylase enzyme due to inactivating mutations of CYP21A2 (cytochrome P450 family 21 subfamily A member 2), the gene encoding the 21-hydroxylase enzyme. More than 200 mutations of the 21-hydroxylase gene have been described, including point mutations, deletions, small insertions, and complex rearrangements.[2]
Certain mutations of the 21-hydroxylase gene, such as deletions, are associated with classical disease, while others are linked to the non-classical form. Compound heterozygotes (i.e., individuals who carry different mutations in each gene) typically have a phenotype that correlates with the less impaired allele. Otherwise, individuals who are compound heterozygotes for a 'mild' and a 'severe' mutation manifest non-classical disease. It is not always possible, however, to accurately predict the phenotype on the basis of the genotype. Studies report variable genotype-phenotype concordance, from 50% to over 97%.[9][10]
Use of this content is subject to our disclaimer