Aetiology
The majority of anorectal abscesses result from infections of the anal glands (cryptoglandular infections).[12] The anal canal has 6 to 14 glands that lie in the plane between the internal and external anal sphincters. Ducts from these glands pass through the internal sphincters and drain into the anal crypts at the dentate line. These glands may become infected when a crypt is occluded by impaction of food matter, by oedema from trauma secondary to a hard stool or foreign body, or as a result of an adjacent inflammatory process such as Crohn's disease.
Pathophysiology
If the crypt does not spontaneously drain into the anal canal, an infection of the inter-sphincteric space may occur. This infection may spread along the inter-sphincteric space and result in an inter-sphincteric, perianal, or supra-levator abscess. The infection may also pass through the external anal sphincter and result in a perirectal abscess.[2][7]
Anorectal abscesses are associated with anal fistulas in 30% to 70% of patients.[4] If these fistulas are not recognised and treated, perirectal abscesses may recur. Perirectal abscesses are also a common manifestation of Crohn's disease and this diagnosis must be considered in patients with recurrent anorectal abscesses.[1]
Classification
Clinical anatomical classification[7]
Anorectal abscesses are usually classified clinically, based on the anatomy of the abscess.
Inter-sphincteric abscesses are located in the space between the internal and external anal sphincter.
Perianal abscesses occur in the superficial soft tissues overlying the inter-sphincteric space.
Perirectal abscesses are found in the ischio-rectal or post-anal spaces.
Supra-levator abscesses occur above the anorectal ring in the supra-levator space.
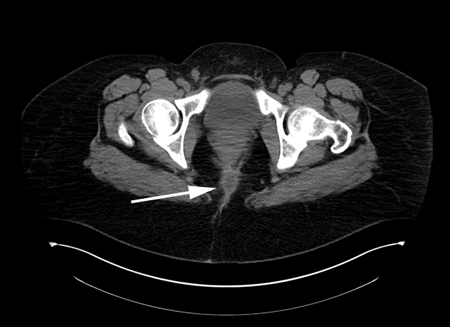
[Figure caption and citation for the preceding image starts]: CT demonstrating a perirectal abscessFrom the collection of Dr C. Neal Ellis; used with permission [Citation ends].
Use of this content is subject to our disclaimer