Urgent considerations
See Differentials for more details
Conditions that cause hypokalaemia can result in varying degrees of clinical severity depending on duration of the insult and presence of other co-morbid conditions.
Certain conditions, such as unreplaced gastrointestinal or urinary losses, are more likely to result in severe hypokalaemia. Potassium replacement is required urgently in patients with severe hypokalaemia (serum potassium <2.5 mmol/L [<2.5 mEq/L]) or in patients who are symptomatic.
Caution is required when replacing potassium in patients with a concurrent disorder (such as anuric patients or those with chronic kidney disease), or therapy (such as during diuretic therapy for heart failure or insulin therapy for diabetic ketoacidosis or hyperosmolar hyperglycaemic state [HHS]).
Urgent potassium replacement
Potassium replacement is required urgently in patients with severe hypokalaemia (serum potassium <2.5 mmol/L [<2.5 mEq/L]) or in patients who are symptomatic.[44] Serum potassium concentration is monitored frequently during repletion, to avoid hyperkalaemia. The method of replacement depends on the clinical situation:
Patients able to tolerate oral intake: if the patient does not have diabetic ketoacidosis or HHS, potassium repletion is most easily done orally, even in people with severe hypokalaemia. The serum potassium concentration can rise acutely by as much as 1 to 1.5 mEq/L after an oral dose of 40 to 60 mEq of potassium. Intravenous potassium chloride may be used as an adjunct to oral replacement if large doses are required, as these can cause gastric irritation. Intravenous replacement can, however, cause discomfort at the infusion site.
Patients unable to tolerate oral intake: intravenous potassium replacement is required. However, even low rates of administration can sometimes result in hyperkalaemia, so caution is required.
Patients with diabetic ketoacidosis or HHS: intravenous potassium replacement is needed if hypokalaemia occurs, as there are usually marked potassium losses.[11]
Consult local protocols for detail on potassium administration. Throughout repletion, careful monitoring of the physiologic effects of severe hypokalaemia (ECG abnormalities with continuous cardiac monitoring, muscle weakness, or paralysis) is essential.
Any potassium supplement in patients who are taking a potassium-sparing diuretic requires particularly careful monitoring to prevent inadvertent over-treatment and the possible development of hyperkalaemia. This can be a problem in patients with moderate to severe heart failure. These patients have decreased renal perfusion, due to the fall in cardiac output, and are often treated with an ACE inhibitor and/or angiotensin II receptor blocker, plus an aldosterone antagonist (spironolactone or eplerenone). This combination of factors results in a marked reduction in urinary potassium excretion and an increased risk of hyperkalaemia.
Concurrent hypomagnesaemia
It is important to determine whether there is hypomagnesaemia (<0.75 mmol/L [<1.5 mEq/L]) because hypokalaemia can often only be corrected once the magnesium deficit has been addressed.[34][35]
Intravenous magnesium replacement therapy is indicated in cases of severe (<1 mEq/L) or symptomatic hypomagnesaemia.[45] Patients with mild magnesium depletion are usually asymptomatic and can be managed with oral magnesium replacement.
Patients suspected of having hypomagnesaemic-hypokalaemic ventricular arrhythmias should receive intravenous magnesium slowly over 8 to 24 hours. Consult local protocols for detail on magnesium administration.
Severe muscle weakness or paralysis
Severe muscle weakness is a complication of hypokalaemia. Provided the hypokalaemia develops slowly, it does not usually occur at potassium concentrations greater than 2.5 mmol/L (2.5 mEq/L).[11] Weakness usually begins with the lower extremities, progresses to the torso and upper extremities, and can worsen to the point of paralysis. Respiratory muscle weakness can sometimes be severe enough to result in respiratory failure and death. Involvement of the GI muscles can result in ileus and its associated symptoms of distension, anorexia, nausea, and vomiting. Cramps, paraesthesias, tetany, muscle tenderness, and atrophy can also occur. Urgent potassium replacement is required.
Cardiac arrhythmias
A variety of arrhythmias may be associated with hypokalaemia. Arrhythmias include sinus bradycardia, premature atrial and ventricular beats, paroxysmal atrial or junctional tachycardia, atrioventricular block, and ventricular tachycardia or fibrillation.[11] Typically, there is depression of the ST segment, decrease in the amplitude of the T wave, and an increase in the amplitude of U waves (often seen in the lateral precordial leads V4 to V6).[Figure caption and citation for the preceding image starts]: 12-lead ECG demonstrating prominent U-waves in a patient with hypokalaemiaFrom: Lin HW, Chau T, Lin CS, Lin SH, Recurring paralysis, BMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0577 [Citation ends].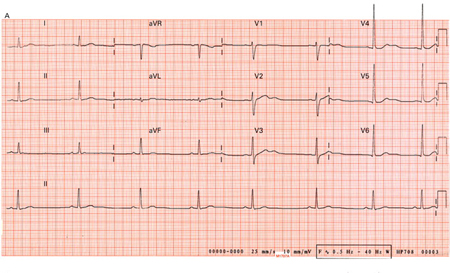
The presence of concomitant factors, such as coronary ischaemia, digitalis use, increased beta-adrenergic activity, and magnesium depletion, can promote arrhythmias due to hypokalaemia. In addition, diuretic-induced magnesium depletion promotes arrhythmias, particularly in patients also treated with drugs that prolong the QT interval, which can predispose to torsades de pointes.[46] Urgent potassium replacement is required.
Renal abnormalities
Chronic hypokalaemia may result in renal dysfunction. It can induce impaired urinary concentrating ability (which may be symptomatic with nocturia, polyuria, and polydipsia), increase renal ammonia production due to intracellular acidosis, increase renal bicarbonate reabsorption, and lead to hypokalaemic nephropathy.[47]
Hypokalaemic periodic paralysis
This is a rare disorder characterised by potentially fatal episodes of muscle weakness or paralysis that can affect the respiratory muscles. Hypokalaemic periodic paralysis is often precipitated by exercise, stress, an excessively large carbohydrate meal, or conditions associated with increased release of adrenaline, cortisol, aldosterone, or insulin.[8] Acute attacks can lower the plasma potassium concentration by 1.5 to 2.5 mmol/L (1.5 to 2.5 mEq/L) and are often accompanied by hypophosphataemia and hypomagnesaemia.[9] Urgent potassium replacement is required.
Thyrotoxic periodic paralysis is characterised by hypokalaemia, flaccid paralysis, and thyrotoxicosis. Complications include hypercapnic respiratory failure and ventricular fibrillation. Early diagnosis is essential because thyrotoxic periodic paralysis is potentially reversible; prompt treatment can lead to rapid resolution.[48]
Diabetic ketoacidosis and hyperosmolar hyperglycaemic state
Renal potassium excretion increases are primarily related to the glucose osmotic diuresis and to hypovolaemia-induced hyperaldosteronism. However, in diabetic ketoacidosis, because of a shift of potassium out of the cells, serum potassium is often elevated at presentation. With the administration of insulin, the serum potassium concentration often falls dramatically.
Serum potassium is maintained between 4.0 and 5.0 mmol/L (4.0 and 5.0 mEq/L) to prevent hypokalaemia. Potassium chloride is generally added to the intravenous replacement fluids once the serum potassium concentration falls below 5.0 mmol/L (5.0 mEq/L).[49] Insulin therapy is delayed until the serum potassium is more than 3.5 mmol/L (3.5 mEq/L) to avoid possible arrhythmias, cardiac arrest, and respiratory muscle weakness.[49]
Potassium repletion is more urgent in patients with massive potassium deficits who are hypokalaemic before therapy. Consult local protocols for detail on potassium administration.
Use of this content is subject to our disclaimer