Approach
Barrett's oesophagus is a histological diagnosis, and endoscopy with mucosal biopsy is required to establish the diagnosis. The physical examination is essentially normal.
Symptoms
Key factors in the patient's history are symptoms of GORD:
Heartburn and regurgitation
Can occur during the day or at night
Many patients are asymptomatic.
Atypical symptoms include:
Chest pain
Voice changes (i.e., laryngitis)
Respiratory symptoms (i.e., reflux-induced asthma, reactive airway disease, or aspiration pneumonia)
Dysphagia (suggests advanced reflux, and may indicate stricture formation or ineffective oesophageal motility).
See also Gastroesophageal reflux disease (Diagnosis Approach).
Upper GI endoscopy with biopsy
The key diagnostic test is upper GI endoscopy with identification of the mucosal changes of Barrett's oesophagus. High-resolution/high-definition white light endoscopy, with or without electronic chromoendoscopy, should be used for detailed inspection of the oesophagus. Systematic endoscopic biopsies must be obtained cephalad to the anatomical gastro-oesophageal junction of all abnormal-appearing oesophageal mucosa.[7] Pathologically, histology reveals columnar-lined epithelium with goblet cells, with or without dysplasia.[1][4][Figure caption and citation for the preceding image starts]: Barrett's oesophagus; note salmon-coloured mucosa extending superior to the gastro-oesophageal junction as a continuous columnFrom the personal collection of Dr Vic Velanovich; used with permission [Citation ends].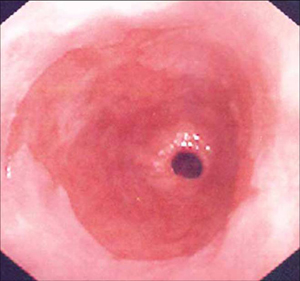 [Figure caption and citation for the preceding image starts]: Barrett's oesophagus; note salmon-coloured mucosa extending superior to the gastro-oesophageal junction with marked irregular borderFrom the personal collection of Dr Vic Velanovich; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Barrett's oesophagus; note salmon-coloured mucosa extending superior to the gastro-oesophageal junction with marked irregular borderFrom the personal collection of Dr Vic Velanovich; used with permission [Citation ends].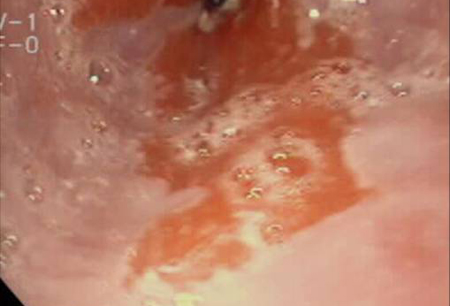 [Figure caption and citation for the preceding image starts]: Barrett's metaplasia without dysplasia, demonstrating columnar epithelium with goblet cells from superior to the gastro-oesophageal junctionCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].
[Figure caption and citation for the preceding image starts]: Barrett's metaplasia without dysplasia, demonstrating columnar epithelium with goblet cells from superior to the gastro-oesophageal junctionCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends]. [Figure caption and citation for the preceding image starts]: Barrett's metaplasia with low-grade dysplasia; note the more irregular cells and nucleiCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].
[Figure caption and citation for the preceding image starts]: Barrett's metaplasia with low-grade dysplasia; note the more irregular cells and nucleiCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].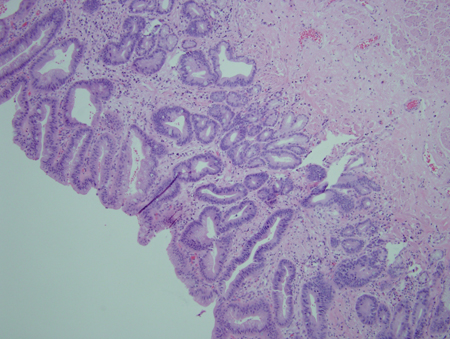 [Figure caption and citation for the preceding image starts]: Barrett's metaplasia with high-grade dysplasia; note more advanced irregularity of the cellsCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].
[Figure caption and citation for the preceding image starts]: Barrett's metaplasia with high-grade dysplasia; note more advanced irregularity of the cellsCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].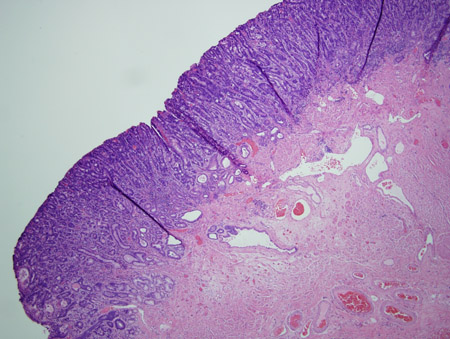 [Figure caption and citation for the preceding image starts]: Barrett's metaplasia with high-grade dysplasia associated with a focus of intramucosal carcinoma; note the frankly malignant cells beyond the confines of the basement membrane to involve the lamina propriaCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].
[Figure caption and citation for the preceding image starts]: Barrett's metaplasia with high-grade dysplasia associated with a focus of intramucosal carcinoma; note the frankly malignant cells beyond the confines of the basement membrane to involve the lamina propriaCourtesy of Adrian Ormsby, MD, Henry Ford Hospital, Detroit, MI [Citation ends].
Upper GI contrast radiography
Barium oesophagogram is still used by some clinicians as the initial diagnostic test in patients with dysphagia, as it is a non-invasive test with good sensitivity for the detection of structural abnormalities in the oesophagus. Abnormal findings on barium oesophagogram require confirmation and further endoluminal evaluation by endoscopy. The identification of a type I (sliding) hiatal hernia is common in patients with Barrett's oesophagus, and is an important risk factor for chronic gastro-oesophageal reflux.[34]
Emerging tests
Transnasal endoscopy permits office-based, unsedated evaluation of the oesophagus, but requires a special, thin-calibre digital endoscope, which is not readily available in most practices.[35]
Capsule endoscopy using a specially designed video capsule (swallowed by the patient in the supine position) provides adequate images of the oesophagus. However, it does not permit tissue sampling and its diagnostic characteristics are still sub-optimal.[36]
A gelatin-coated sponge attached to a string can be swallowed by the patient and then pulled out, obtaining cytology samples from the distal oesophagus. This removes the need for sedation or endoscopy, being performed using local anaesthetic spray to reduce discomfort. Studies are ongoing but sponge cytology may be an acceptable alternative to endoscopy.[7]
Novel techniques aimed at discerning non-dysplastic Barrett's oesophagus from dysplasia or neoplasia include chromoendoscopy (with the use of methylene blue, indigo carmine, or lugol's solution), autofluorescence imaging, confocal laser endomicroscopy, optical coherence tomography, and spectroscopy. However, the recommendations for use of these techniques in guidelines is mixed.[1][7][32]
Use of this content is subject to our disclaimer