Investigations
1st investigations to order
ECG
Test
Provides only supportive evidence. Echocardiography is required to confirm the presence of AR.
Chronic severe AR: may demonstrate non-specific ST-T wave changes, left ventricular hypertrophy (LVH) with left axis deviation due to compensatory LV chamber enlargement, or isolated premature ventricular contraction. In later stages of LV dysfunction, LV conduction delays may be seen.
Acute AR: may reveal some non-specific ST-T wave changes and sinus tachycardia or arrhythmias; evidence of myocardial ischaemia may also be present.
Conduction abnormalities can also be seen in active infective endocarditis resulting from paravalvular abscess.
Result
may show non-specific ST-T wave changes, left axis deviation, or conduction abnormalities
chest x-ray
Test
Chronic AR may produce cardiomegaly in the leftwards and inferior direction due to compensatory eccentric hypertrophy from increased end-diastolic volume. The aortic knob is typically prominent in severe hypertensive patients and those with aortic root dilation.
In chronic severe AR, the aortic root sometimes progressively enlarges due to increased stroke volume and increased systolic blood pressure; calcification of the aortic valve is uncommon in pure AR but can be seen in patients with combined atrial stenosis and AR.
Result
may show cardiomegaly
echocardiogram
Test
The preferred method for non-invasive detection and evaluation of the severity and aetiology of AR.
Result
visualisation of the origin of regurgitant jet and its width; detection of cause of aortic valve pathology
M-mode and 2-dimensional imaging
Test
Helps indirectly assess AR. Two-dimensional echocardiography is very important in evaluating the valvular anatomy, assessing aortic root dilation, and monitoring the left ventricular response to volume overload.[Figure caption and citation for the preceding image starts]: Parasternal long-axis view demonstrating aortic regurgitation jetFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].
Possible findings include premature closure of the mitral valve (severe/acute AR), diastolic fluttering of the anterior mitral leaflet from the regurgitant aortic jet, and hyperdynamic interventricular septal motion.
Result
assessment of valvular anatomy, aortic root dilation, and left ventricular response to volume overload
colour flow Doppler
Test
One of the most specific and sensitive techniques used to judge the severity of the regurgitant flow by using the ratio of proximal jet width to left ventricular outflow tract and ratio of cross-sectional area of jet to left ventricular outflow tract. Vena contracta, which is the narrowest region of regurgitant jet just below the aortic valve, may also be used.[24][Figure caption and citation for the preceding image starts]: Parasternal long-axis view demonstrating aortic regurgitation jet width and heightFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].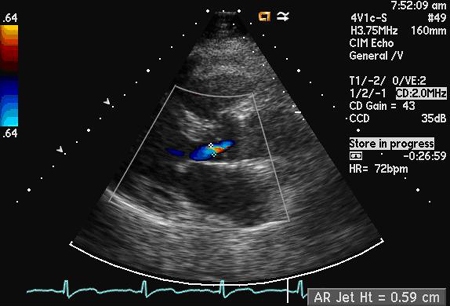 [Figure caption and citation for the preceding image starts]: Parasternal long-axis view demonstrating left ventricular outflow tract diameterFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal long-axis view demonstrating left ventricular outflow tract diameterFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].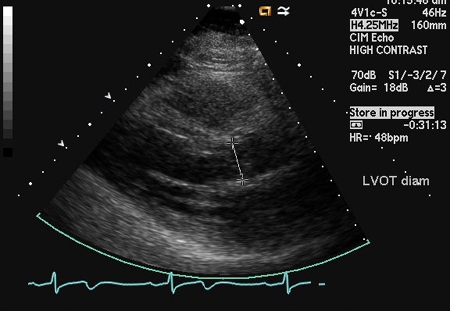 [Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing vena contracta of the aortic regurgitation jetFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing vena contracta of the aortic regurgitation jetFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].
The length of the jet column in the ventricle was previously used but is no longer considered a measure of severity.
Parasternal views are preferred over the apical view because of better axial resolution.
Result
detection and quantification of regurgitant flow
pulsed wave Doppler
Test
As AR gets worse, a greater degree of flow reversal occurs and holodiastolic flow reversal indicates severe AR; pulsed wave Doppler can quantitate this effect by assessing the regurgitant stroke volume and effective regurgitant orifice area.
The diastolic flow reversal is measured in the descending aorta from a suprasternal probe position.[Figure caption and citation for the preceding image starts]: Pulsed wave Doppler of the regurgitant jetFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].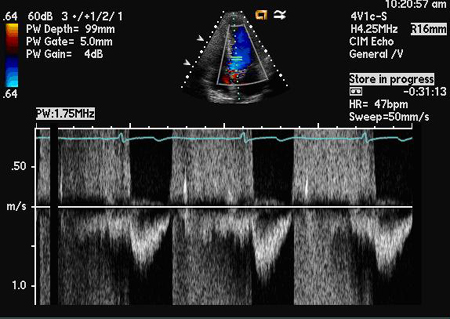 Regurgitant stroke volume can be calculated by subtracting forwards stroke volume, which can be determined at mitral valve, from total stroke volume (aortic valve). Both regurgitant stroke volume and regurgitant fraction can be calculated from this.
Regurgitant stroke volume can be calculated by subtracting forwards stroke volume, which can be determined at mitral valve, from total stroke volume (aortic valve). Both regurgitant stroke volume and regurgitant fraction can be calculated from this.
Effective regurgitant orifice area is another measure to assess the severity of AR, and can be calculated by dividing regurgitant stroke volume by jet velocity time integral of the AR assessed by continuous wave Doppler.[24]
Result
detection and quantification of holodiastolic flow reversal
continuous wave Doppler
Test
As AR gets worse, left ventricular diastolic pressure rapidly increases and aortic diastolic pressure rapidly falls, resulting in shorter pressure half-time or steeper slope of velocity deceleration. These measures can be used as part of the assessment of AR severity.[Figure caption and citation for the preceding image starts]: Continuous wave Doppler of the regurgitant jet demonstrating pressure half-time of the aortic regurgitant velocityFrom the collections of Dr Sanjeev Wasson and Dr Nishant Kalra; used with permission [Citation ends].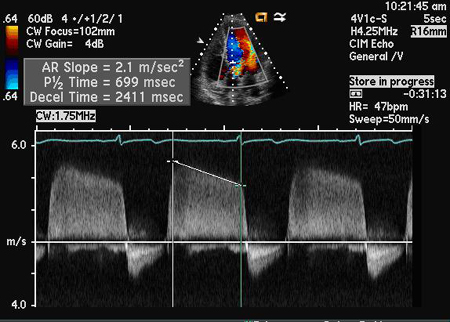
Result
may show shorter pressure half-time or steeper slope of velocity deceleration in severe AR
Investigations to consider
radionuclide angiography
Test
A useful non-invasive, accurate method of evaluating AR in patients with sub-optimal echocardiogram. Serial measurements can be helpful in early detection of systolic dysfunction.[25]
Result
measurement of ejection fraction and regurgitation fraction; detection of relative ventricular enlargement
MRI
Test
Provides accurate assessment of ventricular diameters and volumes both in systole and diastole. It also allows accurate measurement of regurgitant volume and orifice size. MRI is the most accurate non-invasive technique for assessing AR, but is seldom used due to its high cost. MRI can be used for initial and serial evaluation of left ventricular function, volume, and AR severity in patients with an inconclusive echocardiogram.
Result
measurement of ventricular diameter and volume, regurgitant volume, and orifice size
exercise stress testing
Test
Not used as a diagnostic test, but can be used to assess the symptomatic response in patients with history of equivocal symptoms and chronic AR.[1]
Result
assessment of functional capacity and symptomatic response
cardiac catheterisation
Test
Used to evaluate coronary anatomy in patients with high risk for coronary artery disease (CAD) and who will be undergoing aortic valve replacement/repair. Men aged >35 years, premenopausal women aged >35 years with risk factors for CAD, and postmenopausal women should undergo coronary angiography. Although echocardiogram accurately evaluates the severity of AR, if the results are inconclusive or discordant with clinical findings, cardiac catheterisation should be performed to assess the severity of AR and left ventricular (LV) function.[1] With the help of aortic root angiography, the severity of AR and aortic root size can be assessed.
Result
evaluation of the extent and severity of CAD and measurement of associated LV function
Use of this content is subject to our disclaimer