Investigations
1st investigations to order
CT abdomen/pelvis
Test
Radiological assessment of potential lesions using CT (with or without contrast) is the definitive test for initial diagnosis and staging of RCC.[1][61]
CT allows for characterisation of renal lesions; interpretation as benign or malignant; assessment of renal mass invasiveness, lymph node and venous involvement, and the condition of the adrenal glands and other solid organs.[18]
Contrast-enhanced CT with renal protocol has been found to have 100% specificity and ≥90% sensitivity for characterising a renal mass as malignant.[71] There is evidence to suggest that the overall accuracy of tumour extent on CT is 93% specific and 96% sensitive when compared with final pathological staging; accuracy is 99% specific for adrenal involvement but with variable positive predictive values (35% to 92%); there is a 10% false-negative rate and a 58% false-positive rate for lymph node assessment.[71][Figure caption and citation for the preceding image starts]: CT scan showing localised right upper pole kidney cancerFrom the collection of M. Jewett; used with permission [Citation ends].
Result
renal mass, regional lymphadenopathy, and/or visceral/bone metastases
CT chest
MRI abdomen/pelvis
Test
MRI is an alternative to CT for diagnosis and staging, particularly in patients where contrast dye is contraindicated (due to allergy or renal dysfunction).[61]
MRI provides information about adrenal invasion, and the extent of vena cava involvement by tumour or thrombus if poorly defined on CT.[18][61][Figure caption and citation for the preceding image starts]: CT scan showing localised right upper pole kidney cancerFrom the collection of M. Jewett; used with permission [Citation ends].
MRI may be more useful than CT in assessing potential benign lesions such as angiomyolipoma.[72]
Result
renal mass, regional lymphadenopathy, and/or visceral/bone metastases
abdominal/pelvic ultrasound
Test
Diagnosis may be suggested by ultrasound.[18] However, it is not possible to assess complex cystic masses and/or solid renal masses with ultrasound alone.
Ultrasound can be used to detect cystic and solid renal lesions, and determine if cystic renal lesions are benign, but it is less accurate than MRI and CT, especially in detecting smaller lesions and characterising more complex renal masses especially in hereditary syndromes prone to cystic disease (e.g., VHL).[64][65]
If lesions are detected on abdominal ultrasound performed for other indications, the next investigation should be CT or MRI of the abdomen and pelvis.[63]
Result
abnormal renal cyst/mass, lymphadenopathy, and/or other visceral metastatic lesions
FBC
Test
Laboratory findings in paraneoplastic syndromes may include anaemia from chronic disease, and erythrocytosis from excess erythropoietin production.[19]
Result
paraneoplastic syndrome: reduced Hb, or elevated red blood cells
LDH
Test
Poor prognostic marker in advanced RCC as per the Memorial Sloan Kettering Cancer Center (MSKCC) score for metastatic RCC.[62]
Result
advanced RCC: >1.5 times the upper limit of normal
corrected calcium
Test
Poor prognostic marker in advanced RCC as per the Memorial Sloan Kettering Cancer Center (MSKCC) score for metastatic RCC.[62]
Result
advanced RCC: >2.5 mmol/L (>10 mg/dL)
liver function tests
Test
Transaminitis (elevated liver transaminases, aspartate aminotransferase/alanine aminotransferase) and/or poor liver function may be indicative of metastatic lesions.
In the absence of liver metastases, cholestasis (elevated bilirubin, alkaline phosphatase, gamma-GT), with concomitant elevated prothrombin time, thrombocytosis, and hepatosplenomegaly, is a paraneoplastic presentation of RCC known as Stauffer syndrome.[19]
Result
metastatic disease/paraneoplastic syndrome: abnormal
coagulation profile
Test
In the absence of liver metastases, cholestasis (elevated bilirubin, alkaline phosphatase, gamma-GT), with concomitant elevated prothrombin time (PT), thrombocytosis, and hepatosplenomegaly, is a paraneoplastic presentation of RCC known as Stauffer syndrome.[19]
Result
paraneoplastic syndrome: elevated PT
creatinine
Test
May be indicative of chronic kidney disease either preceding or due to RCC. Important to know baseline function in choosing surgical approach and/or systemic treatment.
Result
may be elevated
estimated GFR
Test
Used to determine renal function. If reduced, chronic kidney disease staging is important to guide management options and for prognosis.[1]
Result
may be reduced
urinalysis
Test
The presence of non-visible haematuria should prompt investigation for urinary tract pathology.
Proteinuria is neither sensitive nor specific, but the presence of significant proteinuria can indicate renal dysfunction from a variety of causes, including RCC. Proteinuria is also often seen in chronic kidney disease and hypertension, which are risk factors for RCC.
Result
haematuria and/or proteinuria
Investigations to consider
MRI brain/spine
bone scan
Test
Only recommended if patient presents with localising bone pain and/or elevated alkaline phosphatase.[18]
Result
normal, or abnormal uptake in bone site consistent with metastases
biopsy
Test
Renal mass biopsy is not required in cases where imaging demonstrates a malignant renal mass with no evidence of distant metastatic disease, as management usually includes surgical resection and diagnosis is confirmed on surgical pathology.[1][69]
Indeterminate (and usually smaller) renal lesions found on imaging can be biopsied to support which candidates are suitable for active surveillance based on tumour histology.[73]
In advanced disease, the most easily and safely biopsied metastatic lesion can provide the diagnosis, although the renal primary is sometimes still biopsied.
Renal mass biopsy should also be considered when an alternative diagnosis (e.g., abscess) is suspected.[1][69]
Result
malignancy of various histology
surgical pathology
Test
Most common histology is clear cell RCC.[1][2][34]
Localised renal mass is best assessed surgically (complete or partial nephrectomy), which also serves as potential definitive treatment. [Figure caption and citation for the preceding image starts]: Gross pathology showing localised right upper pole kidney cancerFrom the collection of M. Jewett; used with permission [Citation ends].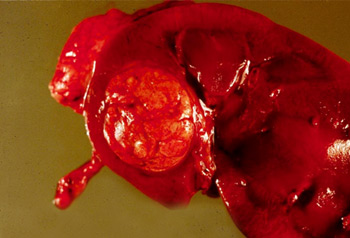
Result
malignancy of various histology
genetic risk evaluation
Test
Genetic risk assessment (which may include germline testing and genetic counselling) should be considered for patients with renal cell carcinoma (RCC) meeting any of the following criteria: age ≤46 years; bilateral or multifocal tumours; family history (close blood relative with a known pathogenic variant or first- or second-degree relative with RCC); personal or family history of mesothelioma or uveal melanoma; specific histological characteristics which suggest a hereditary form of RCC.[1][5][18][61]
Characteristics of hereditary RCC include: multifocal papillary histology; hereditary leiomyomatosis-associated RCC, RCC with fumarate hydratase deficiency or other associated histological features; multiple chromophobe, oncocytoma or oncocytic hybrid; angiomyolipomas of the kidney and one additional tuberous sclerosis complex criterion; succinate dehydrogenase-deficient RCC histology.
Patients meeting these criteria are at a significantly greater risk of having hereditary cancer. Referral to a cancer geneticist, a comprehensive clinical care centre, or hospital with expertise in hereditary cancer is warranted.[18]
Result
may suggest presence of hereditary form of RCC
fluorodeoxyglucose (FDG)-PET scan
Test
PET scanning with FDG tracers is not routinely recommended, but may be useful in certain circumstances, (e.g., for follow-up of advanced/metastatic disease, evaluation before metastasectomy, or in patients with certain hereditary syndromes).[61]
FDG-PET has higher sensitivity and accuracy than bone scan to detect bone metastasis in RCC.[66][67]
FDG-PET may have a role in pre-nephrectomy staging and surveillance of patients with fumarate hydratase (FH)-deficient, succinate dehydrogenase (SDH)-deficient, and hereditary leiomyomatosis and renal cell cancer (HLRCC) tumours.[61][68]
Result
abnormal tracer uptake
Use of this content is subject to our disclaimer