Hereditary spherocytosis (HS) is most commonly diagnosed as a mild condition in children, where there may be jaundice (variable in severity over time) and splenomegaly. Routine laboratory tests usually confirm the diagnosis by detection of:
Increased red-cell turnover (reticulocytosis) ± anaemia
Typical spherocytes on the blood smear
Associated absence of an immune cause (negative direct anti-globulin test [DAT]).
Confirmatory laboratory tests may be required in people with atypical features.[19]King MJ, Garçon L, Hoyer JD, et al. ICSH guidelines for the laboratory diagnosis of nonimmune hereditary red cell membrane disorders. Int J Lab Hematol. 2015 Jun;37(3):304-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.12335
http://www.ncbi.nlm.nih.gov/pubmed/25790109?tool=bestpractice.com
Rarely, additional specialised tests are required.
When a diagnosis of HS is suspected, patients should be referred to a haematology specialist for definitive diagnosis and routine monitoring.
[Figure caption and citation for the preceding image starts]: Diagnostic algorithm for HSCopyright © BMJ Best Practice - All Rights Reserved [Citation ends].
History
HS is found in all populations but is most common in people of Northern European ancestry.[14]Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet. 2008 Oct 18;372(9647):1411-26.
http://www.ncbi.nlm.nih.gov/pubmed/18940465?tool=bestpractice.com
HS is, however, rare in black people.[17]Elmezughi K, Ekpebegh C. Hereditary spherocytosis with successful splenectomy in a pregnant black South African lady: a case report. Pan Afr Med J. 2019 Aug 7:33:288.
https://www.panafrican-med-journal.com/content/article/33/288/full
http://www.ncbi.nlm.nih.gov/pubmed/31692845?tool=bestpractice.com
Most people with HS will have a family history of anaemia, jaundice, splenectomy, or known HS.
Presentation may be at any age. More severely affected individuals tend to present earlier in life. Clinical severity ranges from no symptoms, to fatigue from severe anaemia, and jaundice.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
Often, when there are no symptoms, the condition is detected as an incidental finding when a blood test is performed for another reason.
Parvovirus B19 infection may unmask undiagnosed HS
Children or adults may be asymptomatic until they contract parvovirus B19 infection with resultant aplastic crisis.[20]Forde DG, Cope A, Stone B. Acute parvovirus B19 infection in identical twins unmasking previously unidentified hereditary spherocytosis. BMJ Case Rep. 2014 Jul 29;2014:bcr2013202957.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4120043
http://www.ncbi.nlm.nih.gov/pubmed/25073523?tool=bestpractice.com
[21]Alavi S Md, Arabi N Md, Yazdi MK Md, et al. Hereditary spherocytosis unmasked by human parvovirus B19 induced aplastic crisis in a family. Iran J Med Sci. 2015 Sep;40(5):461-4.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4567607
http://www.ncbi.nlm.nih.gov/pubmed/26379354?tool=bestpractice.com
Parvovirus B19 directly attacks erythroid precursors in the bone marrow and results in erythroid aplasia for about 10 days. Patients with a shortened red-cell life span, such as occurs in HS (and other haemolytic conditions), have a rapidly progressive anaemia during this period of absent erythropoiesis and typically present with acute onset of marked pallor, lethargy, and fever. The haemoglobin (Hb) value is usually between 3 and 6 g/dL. Reticulocyte count is typically <1%.
During the recovery phase the reticulocyte count increases, and immunity to parvovirus B19 usually results following recovery from an aplastic crisis.
HS symptoms and signs may vary over time
Hyperhaemolytic crises are more common but less severe than aplastic episodes, and are characterised by acceleration of the usual haemolytic process with resulting exacerbation of symptoms. These episodes usually accompany non-specific viral infections, and may be repetitive.
In contrast to an aplastic crisis, the Hb is usually in the 50 to 80 g/L (5-8 g/dL) range (or even higher during milder episodes), the reticulocyte count is raised, and the patient is more jaundiced than usual. The spleen rarely may become acutely and significantly enlarged and cause left upper quadrant abdominal pain and symptoms of early satiety. The spleen generally shrinks to its previous size between episodes. [Figure caption and citation for the preceding image starts]: Presentation of HS by ageCopyright © BMJ Best Practice - All Rights Reserved [Citation ends].
Physical examination
Many individuals with HS have mild jaundice. It is a common feature when HS presents in the neonatal period.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
Severity of the jaundice is not necessarily related to future severity of HS.
In some cases, the jaundice is severe enough to warrant exchange transfusion.[7]Bolton-Maggs PH, Langer JC, Iolascon A, et al; General Haematology Task Force of the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of hereditary spherocytosis - 2011 update. Br J Haematol. 2012 Jan;156(1):37-49.
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2141.2011.08921.x/full
http://www.ncbi.nlm.nih.gov/pubmed/22055020?tool=bestpractice.com
Very rarely, HS may present with hydrops foetalis or stillbirth due to severe anaemia.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
[22]Hannah DM, Tressler TB, Taboada CD. Nonimmune hydrops fetalis due to autosomal recessive hereditary spherocytosis. Case Rep Womens Health. 2017 Oct;16:4-7.
https://www.sciencedirect.com/science/article/pii/S2214911217300577
http://www.ncbi.nlm.nih.gov/pubmed/29594000?tool=bestpractice.com
The diagnosis of HS should be considered in any individual with unexpected or unexplained splenomegaly at any age. Splenomegaly (mild to moderate enlargement) is very common in HS of all severities but is not specific to this disorder.[7]Bolton-Maggs PH, Langer JC, Iolascon A, et al; General Haematology Task Force of the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of hereditary spherocytosis - 2011 update. Br J Haematol. 2012 Jan;156(1):37-49.
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2141.2011.08921.x/full
http://www.ncbi.nlm.nih.gov/pubmed/22055020?tool=bestpractice.com
The splenomegaly generally does not have any symptoms or clinical consequences. However, during hyperhaemolytic crises the spleen rarely may become acutely and significantly enlarged and cause left upper quadrant abdominal pain and symptoms of early satiety. The spleen generally shrinks to its previous size between episodes.
Individuals with HS may or may not have signs of anaemia.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
Depending on the severity of the condition, signs of anaemia will be variable: from no obvious signs to severe pallor. [Figure caption and citation for the preceding image starts]: Jaundiced sclera in eye of child with HSFrom the collection of Paula Bolton-Maggs, University of Manchester, UK; used with permission [Citation ends].
Initial tests
Many cases are detected as an incidental finding when a blood count is done for another purpose. The diagnosis should also be considered in any patient with jaundice or splenomegaly, or with family history of HS in a first-degree relative.[23]Christensen RD, Yaish HM, Gallagher PG. A pediatrician's practical guide to diagnosing and treating hereditary spherocytosis in neonates. Pediatrics. 2015 Jun;135(6):1107-14.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4444801
http://www.ncbi.nlm.nih.gov/pubmed/26009624?tool=bestpractice.com
The diagnosis should be considered in the context of an unexpectedly low Hb result at any age.
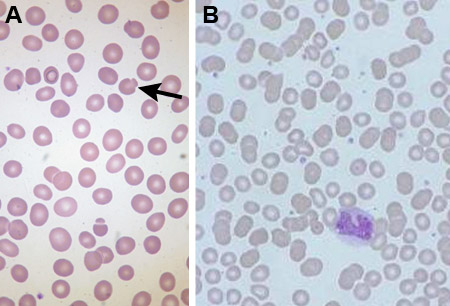
Full blood count and smear
In most cases a blood count and smear is diagnostic. The patient has a normal or reduced Hb, normal or reduced MCV, and often an raised MCHC (>350 g/L [>35 g/dL]).[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
[23]Christensen RD, Yaish HM, Gallagher PG. A pediatrician's practical guide to diagnosing and treating hereditary spherocytosis in neonates. Pediatrics. 2015 Jun;135(6):1107-14.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4444801
http://www.ncbi.nlm.nih.gov/pubmed/26009624?tool=bestpractice.com
Abnormal red-cell morphology of spherocytes is present on the blood smear, with increased reticulocytes.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
The blood smear may demonstrate pincer cells (mushroom-shaped cells) in addition to spherocytes, which are due to band 3 protein mutations.[23]Christensen RD, Yaish HM, Gallagher PG. A pediatrician's practical guide to diagnosing and treating hereditary spherocytosis in neonates. Pediatrics. 2015 Jun;135(6):1107-14.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4444801
http://www.ncbi.nlm.nih.gov/pubmed/26009624?tool=bestpractice.com
Anaemia may be absent in HS when the marrow output increases sufficiently to keep the Hb normal, but there will be an increase in reticulocytes (known as compensated haemolysis).
Neonatal blood smears can be difficult to interpret. Careful review of the blood smear is needed with follow-up if the diagnosis is not clear. Typical blood smear appearances of spherocytes are easier to see after a few months.
Differentials
Careful analysis of the red-cell morphology from the blood smear is very important in order not to miss alternative less-common disorders.[24]Bolton-Maggs PH, King MJ. Hereditary spherocytosis, hereditary elliptocytosis and related disorders. In: Young NS, Gershon SL, High KA, eds. Clinical hematology. Philadelphia, PA: Mosby Elsevier; 2006:293-307. The presence of spherocytes is not limited to HS and other diagnoses must be ruled out by appropriate history, the clinical setting, and investigations.[24]Bolton-Maggs PH, King MJ. Hereditary spherocytosis, hereditary elliptocytosis and related disorders. In: Young NS, Gershon SL, High KA, eds. Clinical hematology. Philadelphia, PA: Mosby Elsevier; 2006:293-307.
The most important differential is auto-immune haemolytic anaemia (AIHA). In AIHA, abnormal antibodies coat the red cells and can be detected by the direct anti-globulin test (DAT), which is negative in HS. In infancy, haemolysis caused by irregular maternal IgG antibodies must also be excluded as a possible cause.
Differentiation of HS from other inherited red-cell membrane disorders is important. Many of these are obvious from the blood smear appearances (e.g., elliptocytosis), but where the red-cell appearances are atypical, other diagnoses should be considered. It is particularly important to rule out hereditary stomatocytosis with membrane transport defects, because splenectomy carries a particularly high risk of venous thromboembolism postoperatively.[25]Crary SE, Buchanan GR. Vascular complications after splenectomy for hematologic disorders. Blood. 2009 Oct 1;114(14):2861-8.
https://ashpublications.org/blood/article/114/14/2861/107813/Vascular-complications-after-splenectomy-for
http://www.ncbi.nlm.nih.gov/pubmed/19636061?tool=bestpractice.com
Serum bilirubin and liver aminotransferases are performed if jaundice is suspected clinically. Cases of congenital dyserythropoietic anaemia have been misdiagnosed as HS.[26]Kedar P, Parmar V, Devendra R, et al. Congenital dyserythropoietic anemia type II mimicking hereditary spherocytosis in Indian patient with SEC23B-Y462C mutations. Ann Hematol. 2017 Dec;96(12):2135-9.
http://www.ncbi.nlm.nih.gov/pubmed/28879554?tool=bestpractice.com
[27]Danise P, Amendola G, Nobili B, et al. Flow-cytometric analysis of erythrocytes and reticulocytes in congenital dyserythropoietic anaemia type II (CDA II): value in differential diagnosis with hereditary spherocytosis. Clin Lab Haematol. 2001 Feb;23(1):7-13.
http://www.ncbi.nlm.nih.gov/pubmed/11422224?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Blood smear of a patient with HS; spherocyte indicatedFrom the collection of Shelley Crary, University of Texas Southwestern Medical Center, TX; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Blood smear of patient with HS (A) compared with normal blood smear (B); Pincer cell (mushroom-shaped cell) indicatedFrom the collection of Paula Bolton-Maggs, University of Manchester, UK; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Blood smear of patient with HS (A) compared with normal blood smear (B); Pincer cell (mushroom-shaped cell) indicatedFrom the collection of Paula Bolton-Maggs, University of Manchester, UK; used with permission [Citation ends].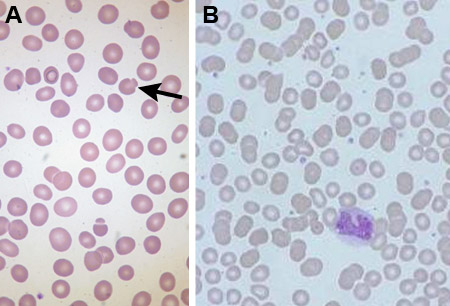
Confirmatory tests to consider
The typical case of HS does not require any confirmatory test. If the diagnosis is equivocal, a confirmatory test may be considered.
Eosin-5-maleimide (EMA) binding test
Confirmation using the eosin-5-maleimide binding test is recommended when the features are not typical (e.g., the morphology on the blood smear is not quite typical or there is no family history).[19]King MJ, Garçon L, Hoyer JD, et al. ICSH guidelines for the laboratory diagnosis of nonimmune hereditary red cell membrane disorders. Int J Lab Hematol. 2015 Jun;37(3):304-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.12335
http://www.ncbi.nlm.nih.gov/pubmed/25790109?tool=bestpractice.com
The EMA binding test is based on fluorescent intensity measured by flow cytometry.[28]King MJ, Behrens J, Rogers C, et al. Rapid flow cytometric test for the diagnosis of membrane cytoskeleton-associated haemolytic anaemia. Br J Haematol. 2000 Dec;111(3):924-33.
http://www.ncbi.nlm.nih.gov/pubmed/11122157?tool=bestpractice.com
[29]King MJ, Smythe JS, Mushens R. Eosin-5-maleimide binding to band 3 and Rh-related proteins forms the basis of a screening test for hereditary spherocytosis. Br J Haematol. 2004 Jan;124(1):106-13.
http://www.ncbi.nlm.nih.gov/pubmed/14675415?tool=bestpractice.com
[30]King MJ, Telfer P, MacKinnon H, et al. Using the eosin-5-maleimide binding test in the differential diagnosis of hereditary spherocytosis and hereditary pyropoikilocytosis. Cytometry B Clin Cytom. 2008 Jul;74(4):244-50.
https://onlinelibrary.wiley.com/doi/10.1002/cyto.b.20413
http://www.ncbi.nlm.nih.gov/pubmed/18454487?tool=bestpractice.com
The EMA binds to band 3 protein, which is disrupted in HS resulting in decreased fluorescence. The EMA binding test has been reported to have a sensitivity of 92.7% for HS and a specificity of 99.1%, but may be abnormal in other red-cell disorders (particularly congenital dyserythropoietic anaemia type II (CDA-II).[28]King MJ, Behrens J, Rogers C, et al. Rapid flow cytometric test for the diagnosis of membrane cytoskeleton-associated haemolytic anaemia. Br J Haematol. 2000 Dec;111(3):924-33.
http://www.ncbi.nlm.nih.gov/pubmed/11122157?tool=bestpractice.com
Acidified glycerol lysis test
Uses 20 microlitres of whole blood and measures the time taken for the absorbance to fall to one half of its original value using a red-cell suspension before and after addition of glycerol. This test has a reported sensitivity of 98.3% for HS and a specificity of 91.1%, but is also positive in AIHA, pregnancy, myelodysplasia, and some other conditions.[31]Hoffmann JJ, Swaak-Lammers N, Breed WP, et al. Diagnostic utility of the pre-incubated acidified glycerol lysis test in haemolytic and non-haemolytic anaemias. Eur J Haematol. 1991 Nov;47(5):367-70.
http://www.ncbi.nlm.nih.gov/pubmed/1761123?tool=bestpractice.com
Cryohaemolysis test
Red blood cells with membrane defects are susceptible to lysis when subjected to severe cold. Sensitivity and specificity of 95% and 96%, respectively, have been reported for HS using a cryohaemolysis threshold of 15%.[32]Iglauer A, Reinhardt D, Schröter W, et al. Cryohemolysis test as a diagnostic tool for hereditary spherocytosis. Ann Hematol. 1999 Dec;78(12):555-7.
http://www.ncbi.nlm.nih.gov/pubmed/10647879?tool=bestpractice.com
Genetic analysis
Used in association with standard tests.[4]Polizzi A, Dicembre LP, Failla C, et al. Overview on hereditary spherocytosis diagnosis. Int J Lab Hematol. 2025 Feb;47(1):18-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.14376
http://www.ncbi.nlm.nih.gov/pubmed/39467036?tool=bestpractice.com
Mutations have been described in five cytoskeletal proteins (alpha- and beta-spectrin, ankyrin, band 3, and protein 4.2).[6]Iolascon A, Avvisati RA. Genotype/phenotype correlation in hereditary spherocytosis. Haematologica. 2008 Sep;93(9):1283-8.
http://www.haematologica.org/content/93/9/1283.full
http://www.ncbi.nlm.nih.gov/pubmed/18757847?tool=bestpractice.com
[33]Qin L, Nie Y, Zhang H, et al. Identification of new mutations in patients with hereditary spherocytosis by next-generation sequencing. J Hum Genet. 2020 Apr;65(4):427-34.
http://www.ncbi.nlm.nih.gov/pubmed/31980736?tool=bestpractice.com
Mutations in genes for ankyrin, band 3, or beta-spectrin may cause a secondary defect of other skeletal proteins. Non-dominant HS can occur as a result of inheritance of a pathogenetic mutation from one parent and a silent low expressed allele from the other, or from de novo mutations. Mutations in the gene for protein 4.2 are more common among Japanese patients with non-dominant HS.[34]Yawata Y, Kanzaki A, Yawata A, et al. Characteristic features of the genotype and phenotype of hereditary spherocytosis in the Japanese population. Int J Hematol. 2000 Feb;71(2):118-35.
http://www.ncbi.nlm.nih.gov/pubmed/10745622?tool=bestpractice.com
[35]Yawata Y, Kanzaki A, Yawata A, et al. Hereditary red cell membrane disorders in Japan: their genotypic and phenotypic features in 1014 cases studied. Hematology. 2001;6(6):399-422.
https://www.tandfonline.com/doi/10.1080/10245332.2001.11746596
http://www.ncbi.nlm.nih.gov/pubmed/27405697?tool=bestpractice.com
Additional tests in difficult cases
The typical case of HS does not require additional tests. Additional tests are indicated:
When the clinical phenotype is more severe than expected from the red-cell appearances
When the red-cell abnormalities are more severe than seen in the one known affected parent
Where splenectomy is considered and the morphology is atypical.
Quantitative protein analysis by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) may be undertaken in atypical cases. SDS-PAGE analyses red-cell membrane content and establishes which membrane protein is deficient by demonstrating protein bands for spectrin, ankyrin, band 3, and protein 4.2 (the membrane proteins that can be affected in HS).[5]Mariani M, Barcellini W, Vercellati C, et al. Clinical and hematologic features of 300 patients affected by hereditary spherocytosis grouped according to the type of the membrane protein defect. Haematologica. 2008 Sep;93(9):1310-7.
http://www.haematologica.org/content/93/9/1310.full
http://www.ncbi.nlm.nih.gov/pubmed/18641031?tool=bestpractice.com
[19]King MJ, Garçon L, Hoyer JD, et al. ICSH guidelines for the laboratory diagnosis of nonimmune hereditary red cell membrane disorders. Int J Lab Hematol. 2015 Jun;37(3):304-25.
https://onlinelibrary.wiley.com/doi/10.1111/ijlh.12335
http://www.ncbi.nlm.nih.gov/pubmed/25790109?tool=bestpractice.com
[36]Eber S, Lux SE. Hereditary spherocytosis--defects in proteins that connect the membrane skeleton to the lipid bilayer. Semin Hematol. 2004 Apr;41(2):118-41.
http://www.ncbi.nlm.nih.gov/pubmed/15071790?tool=bestpractice.com
[37]Lee YK, Cho HI, Park SS, et al. Abnormalities of erythrocyte membrane proteins in Korean patients with hereditary spherocytosis. J Korean Med Sci. 2000 Jun;15(3):284-8.
https://jkms.org/DOIx.php?id=10.3346/jkms.2000.15.3.284
http://www.ncbi.nlm.nih.gov/pubmed/10895969?tool=bestpractice.com
[38]Jarolim P, Murray JL, Rubin HL, et al. Characterization of 13 novel band 3 gene defects in hereditary spherocytosis with band 3 deficiency. Blood. 1996 Dec 1;88(11):4366-74.
https://www.sciencedirect.com/science/article/pii/S0006497120611831
http://www.ncbi.nlm.nih.gov/pubmed/8943874?tool=bestpractice.com
[39]Agre P, Casella JF, Zinkham WH, et al. Partial deficiency of erythrocyte spectrin in hereditary spherocytosis. Nature. 1985 Mar 28-Apr 3;314(6009):380-3.
http://www.ncbi.nlm.nih.gov/pubmed/3982506?tool=bestpractice.com
It is important to exclude rare forms of red-cell disorder where splenectomy is contraindicated.[7]Bolton-Maggs PH, Langer JC, Iolascon A, et al; General Haematology Task Force of the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of hereditary spherocytosis - 2011 update. Br J Haematol. 2012 Jan;156(1):37-49.
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2141.2011.08921.x/full
http://www.ncbi.nlm.nih.gov/pubmed/22055020?tool=bestpractice.com
Splenectomy is of little value in congenital dyserythropoietic anaemia type II (CDA-II), which may be confused with HS.

 [Figure caption and citation for the preceding image starts]: Blood smear of patient with HS (A) compared with normal blood smear (B); Pincer cell (mushroom-shaped cell) indicatedFrom the collection of Paula Bolton-Maggs, University of Manchester, UK; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Blood smear of patient with HS (A) compared with normal blood smear (B); Pincer cell (mushroom-shaped cell) indicatedFrom the collection of Paula Bolton-Maggs, University of Manchester, UK; used with permission [Citation ends].