Approach
A focused history and physical examination may identify laryngeal malignancy in patients with hoarseness, sore throat, dysphagia, odynophagia (painful swallowing), otalgia, and neck mass. Diagnostic delay moderately increases the risk of mortality from head and neck cancers.[32]
History
Risk factors for laryngeal cancer include smoking and alcohol consumption, GORD and bile reflux, previous radiotherapy to the neck, history of vocal fold dysplasia, and family history of laryngeal cancer. Comprehensive documentation and quantification of tobacco use should be included in risk assessment.
Patients often present with insidious onset of hoarseness, sore throat, dysphagia, odynophagia (painful swallowing), otalgia, and neck mass.[33] Chronic laryngitis lasting >3 weeks should be referred to a consultant.
Patients with laryngeal cancer involving the true vocal cords (glottic cancer) may become symptomatic with phonic changes and seek medical attention sooner than those with supraglottic cancer. This is usually because of more obvious symptoms of voice change with even minor changes in vocal fold morphology. Patients with supraglottic cancer often present first with a persistent sore throat and odynophagia (painful swallowing). Neck metastases are more common in patients with supraglottic cancer. They may seek medical attention for a (metastatic) neck mass before having hoarseness or dysphagia.
Physical examination
A breathy, gravelly voice or aphonic condition suggests the presence of laryngeal cancer and may be apparent on initial assessment of the patient. Cachexia, weight loss, and general distress are signs of advanced disease.
The signs of laryngeal cancer include (by organ system):
Ear: otalgia (e.g., middle ear effusion).
Oral cavity and oropharynx: masses or leukoplakia of the posterior pharyngeal wall, tonsillar pillars, tonsils and palate, surfaces of the oral tongue, floor of mouth, and base of the tongue.
Laryngeal inlet: lesions of the vocal cords, aryepiglottic folds, and local extension of tumour. A handheld mirror and headlight can provide an excellent view of the base of the tongue and larynx. Indirect laryngoscopy also allows immediate evaluation for obvious lesions involving the glottis. Laryngeal squamous cell carcinoma may appear as a mucosal irregularity, erythroplasia, or leukoplakia. Examination is often limited by a strong gag reflex.
Neck: cervical lymph nodes or masses (noting approximate size, location, mobility, and degree of firmness), laryngeal crepitus (lack may indicate a more advanced stage of cancer), palpable nodules or masses of parotid or thyroid.
Lungs: stridor (biphasic, inspiratory, and expiratory), diminished breath sounds (suggests pneumonia, especially in circumstances in which aspiration is suspected). The difficulty with which the patient is breathing at rest, while speaking, and while supine should be noted. Patients who may appear comfortable while upright may have significant dyspnoea while lying supine. In advanced cases, the airway may be compromised.
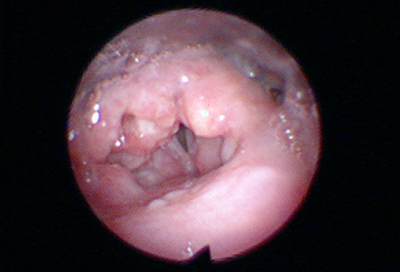
Heart: haemodynamic instability may be present (e.g., catastrophic vascular-aerodigestive fistula).[Figure caption and citation for the preceding image starts]: Irregular mass of left arytenoid and aryepiglottic folds, and the right arytenoid mucosaFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
Laboratory
Fine needle aspiration is indicated in patients who present with a palpable neck mass.[1] Cytological analysis of the aspirate may often confirm the diagnosis of squamous cell carcinoma, as well as other malignancies. A negative result does not rule out cancer. Biopsy of laryngeal findings from the initial examination is generally deferred to the specialist and follows formal radiographic investigation. Direct visualisation of a laryngeal lesion is highly suggestive of laryngeal cancer, but diagnosis must be confirmed by tissue biopsy.
Imaging
Once laryngeal malignancy is suspected, a neck computed tomography (CT) with contrast is indicated.[1] Ideally this is performed before biopsies are taken, to limit the confounding factor of post-biopsy oedema. Neck CT with contrast is essential in the complete staging of laryngeal cancer. Intravenous contrast enables better distinction between normal and abnormal soft tissue planes.[34] Cuts should be finer than 2.5 mm. Suspicious lymph nodes and cartilage invasion are more easily assessed on CT than by physical examination or magnetic resonance imaging.
Whole-body positron emission tomography (PET)/CT scan is more sensitive than CT scans in detecting nodal and distant metastases, and is indicated in patients with higher grade tumours (T3-T4 primary, or ≥N1 nodal stage).[1][Figure caption and citation for the preceding image starts]: CT scan showing bulky tumour invading ala of thyroid cartilageFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].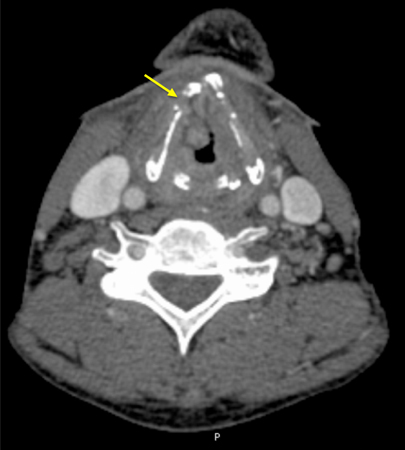 [Figure caption and citation for the preceding image starts]: Large, bulky transglottic mass and increased uptake on PET (bright yellow/orange)From the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Large, bulky transglottic mass and increased uptake on PET (bright yellow/orange)From the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
Chest CT (with or without contrast) typically accompanies neck CT, because the most common site of metastasis of head and neck cancer is to the lungs.
Specialised examinations
Flexible endoscopy allows simultaneous rapid assessment of laryngeal pathology and of the upper airway. Flexible fibre-optic laryngoscopy (usually performed by the otolaryngologist) identifies areas of leukoplakia, erythroplasia, ulceration, mass, necrosis, or bleeding. The degree of airway obstruction may also be evaluated. Flexible endoscopy is also necessary for sufficient follow-up of patients with laryngeal cancer.
Technique: the nasal cavity that is subjectively most patent is treated with topical decongestant and anaesthetic spray. A flexible fibre-optic laryngoscope is passed through the nasal cavity to evaluate the nasopharynx, oropharynx, base of the tongue, vallecula, both vallecular and laryngeal surfaces of the epiglottis, aryepiglottic folds, arytenoid mucosa, pyriform sinuses, false vocal folds, true vocal folds, and (if appropriately anaesthetised), the subglottis. The patient is asked to phonate, and vocal fold mobility is assessed.
Rigid videostroboscopy of the larynx (usually performed by an otolaryngologist or a speech pathologist) is preferred to evaluate the vibratory motion of the true vocal folds and identify smaller underlying vocal cord pathology. It is less useful in evaluating bulky tumours.
Technique: a rigid 70° telescope is advanced into the laryngeal inlet through the oral cavity while the tongue is gently retracted anteriorly. The patient is asked to breathe through the mouth.
Rigid endoscopy and biopsy under general anaesthesia with relaxation remains the preferred method for completely evaluating laryngeal findings and pathology. A rigid telescope with a magnifying lens may be used to appreciate finer detail and subtle abnormalities. A cupped biopsy forceps is passed through the laryngoscope to obtain biopsy specimens. Frozen section pathology during the procedure is useful to ascertain that sufficient tissue has been obtained to yield a diagnosis. Straight-on (0°) and angled (70°) telescopes are useful to ascertain the size and extent of a tumour, particularly in the case of subglottic cancer.
Technique: after the airway has been secured and general anaesthesia induced, the neck, oral cavity, and oropharynx are carefully palpated. Examination is much more thorough under anaesthesia. The maxillary dentition is protected with a tooth guard (or moist gauze in edentulous patients). The rigid laryngoscope is advanced into the oral cavity to examine the oral cavity, tonsils, posterior pharyngeal wall, base of the tongue, vallecula, epiglottis, aryepiglottic folds, arytenoid mucosa, pyriform sinuses, post-cricoid mucosa, false vocal folds, true vocal folds, and subglottis.
Some centres make use of fluorescence endoscopy. In auto-fluorescence endoscopy (AFE), the mucosa is examined under narrow-spectrum light from a xenon arc lamp. Under the lamp, normal mucosa and benign lesions exhibit a typical green auto-fluorescence (greatest at 515 nm), while cancerous and pre-cancerous lesions exhibit loss of auto-fluorescence, resulting in a red-violet colour. In induced fluorescence endoscopy (IFE), exogenous aminolevulinic acid is applied to the tissues 2 hours before endoscopy, and is preferentially taken up and metabolised by tumour cells, which exhibit a red-orange fluorescence (by contrast with the blue of normal tissue, under filtered blue light). AFE may be particularly useful for early diagnosis of laryngeal cancer and its precursor lesions. IFE may be more suited for detection of recurrent disease after initial surgery.[35]
Laryngeal cancer presents significant concerns for securing the airway. In patients with concerns for significant airway obstruction, an awake tracheostomy may be considered before any endoscopic evaluation under general anaesthesia. The otolaryngologist must coordinate and work closely with the anaesthesiologist in this circumstance.[Figure caption and citation for the preceding image starts]: Irregular mass of left arytenoid and aryepiglottic folds, and the right arytenoid mucosaFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].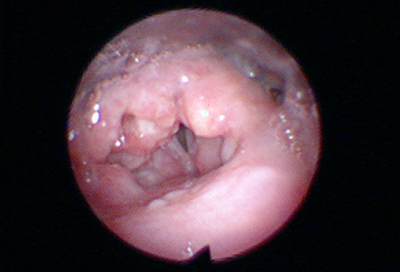 [Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
Use of this content is subject to our disclaimer