Approach
Most patients are asymptomatic, and medullary sponge kidney (MSK) may be diagnosed based on incidental findings following radiological investigation for other reasons. When symptoms are present, they are related to urinary tract infection (UTI) or renal stones.
History
For patients with symptoms, flank pain, haematuria (microscopic or gross), recurrent UTI, recurrent renal stones, hypocitraturia, nephrolithiasis, and nephrocalcinosis are well-described presentations of MSK.[3] Chronic severe pain is a rare presentation in some patients.[29] The disorder is more common among patients with hemi-hypertrophy, Beckwith-Wiedemann's syndrome, Caroli's disease, congenital hepatic fibrosis, Ehlers-Danlos' syndrome, family history of polycystic kidney disease, and chronic kidney disease.
Physical examination
With the exception of patients with complications, such as renal stones or UTI, the physical examination is usually unremarkable. Costovertebral angle tenderness and ipsilateral groin pain may be signs of nephrolithiasis. Associated fever, tachycardia, and hypotension might indicate an obstructing stone with infection, warranting emergency referral to urology.
Imaging
MSK tends to be diagnosed based on incidental findings following radiological investigation for other reasons such as renal stones, infection, or colic. However, if MSK is suspected, intravenous urography (IVU) will confirm the diagnosis.
Plain abdominal x-ray
This may be ordered for non-specific abdominal pain. It is less sensitive and less specific than IVU. However, it is inexpensive and fast, and requires less radiation. In a patient known to have previous radiopaque stones seen on a plain x-ray, it is a diagnostic test of good predictive value for MSK. It may show nephrocalcinosis in one or several papillae; also, renal stones may be observed in the calyces, pelvis, or ureter.[2]
Renal ultrasound
This may be ordered for non-specific abdominal pain, or if urinary tract obstruction is suspected. This is less sensitive and less specific than IVU but more sensitive than plain x-rays, but will usually show no more than nephrocalcinosis that might suggest MSK. A tetrad of ultrasonographic characteristics support a diagnosis of MSK: hypoechoic medullary areas; hyperechoic spots; microcystic dilatation of papillary zone; and multiple calcifications (linear, small stones or calcified intracystic sediment) in each papilla.[12]
Intravenous urography
This test may be ordered first when MSK is strongly suspected because of recurrent stones, or, if surgery is planned for complex stones. It is the principal method for diagnosing MSK. This will show dilated collecting tubules that may or may not have nephrolithiasis. Contrast pools within the dilated, ectatic tubules within the tips of the papilla lead to the appearance of a 'papillary blush' or 'paintbrush' pattern. Most cases usually have bilateral involvement, although the disorder may be limited to a single papilla. The minimal degree of involvement to make the diagnosis is not established. Medullary nephrocalcinosis may be present or absent.
Non-contrast computed tomography (CT)
This is the diagnostic standard method for detecting renal stones. Unfortunately, non-contrast CT is not likely to detect MSK. If non-contrast CT is performed for renal colic, MSK will not be diagnosed. However, multidetector CT has potential for MSK diagnosis; in one study, results showed a sensitivity and specificity of 90% and 100%, respectively, when compared with IVU.[3][30]
CT urogram
Patients may have a CT urogram as a first test for the evaluation of haematuria that incidentally makes the diagnosis of MSK.[31] Multi-detector-row CT scan is performed with intravenous contrast media. It provides images of contrast-filled renal collecting systems, ureters, and the bladder.[32][Figure caption and citation for the preceding image starts]: Computed tomography (CT) urogram showing papillary blush with calculi within dilated collecting tubules (arrows)From Maw AM, et al. Am J Kidney Dis. 2007 Jul;50(1):146-50, with permission [Citation ends].

Laboratory tests
Urinalysis, serum electrolytes, urea/creatinine (to assess renal function), calcium, phosphorus, uric acid, and full blood count should be ordered in the workup for nephrolithiasis, UTI, or pyelonephritis. Urinalysis may reveal microscopic haematuria with or without stones and pyuria (urine containing pus) with UTI. An elevated white blood cell count may indicate infection (pyelonephritis). Urine culture will confirm infection. Stone-risk profiles help determine metabolic risk factors for calcium stones such as hypocitraturia, hyperoxaluria, hypercalciuria, or elevated urine pH. Analysis of stone composition provides information for preventive management.
Pathology assessment at time of percutaneous nephrostolithotomy for stone removal
One study described the findings of patients with MSK who underwent percutaneous nephrostolithotomy (PCNL) for stone removal.[25] The endoscopic appearance was of papillary malformation, either segmental or diffuse. The affected papillae were enlarged and 'billowy', due to enlarged inner medullary collecting ducts, with small, mobile stones in place. Also noted was dilation of Bellini ducts, occasionally plugged by calcium precipitates. Whether most urologists can reliably recognise this appearance as that of MSK during urological procedures has not been determined.
Older literature on the pathology of kidneys removed from patients with radiographically demonstrated MSK reported that the renal papillae included undifferentiated interstitial cells, with dilated inner medullary collecting ducts containing abnormal multilayered epithelium.[33][34] These findings would not be demonstrated by percutaneous kidney biopsy as performed in diagnosing glomerular lesions, but have been shown by papillary biopsies obtained at the time of PCNL for stone removal.[25] As in those older reports based on samples taken at nephrectomy, there were multilayered hyperplastic epithelia in undilated inner medullary collecting ducts, single layered epithelia in dilated collecting ducts, and primitive interstitial cells that resembled embryonic cells. The authors concluded, however, that while papillary biopsy was definitive, it was not practical or necessary for clinical diagnosis. [Figure caption and citation for the preceding image starts]: Endoscopic images of renal papilla from medullary sponge kidney (MSK) stone formers. The affected papillae are characterised by a rounding of contours and enlargement, which creates a billowy appearance (a and b). As part of the general rounding of contours, the papillary tips are blunted. These papillae also show sites of white (panel a, arrowhead) and yellow (a, arrows) plaque, and dilated opening of ducts of Bellini with (c, double arrow) and without deposits (a, asterisk). An occasional calyceal stone is noted (c). The unaffected papillae possess a normal morphology as seen in the compound papillum in (d) and single papillum in (e) (case 5); note numerous sites of white plaque (arrowheads) and an attached stone (double arrowhead). The unique morphology of affected papillae of MSK patients can be characteristic of all papillae (diffuse pattern) of a kidney or only some of the papillae (segmental pattern)From Evan AP, et al. Anat Rec. 2015 May;298(5):865-77, with permission [Citation ends].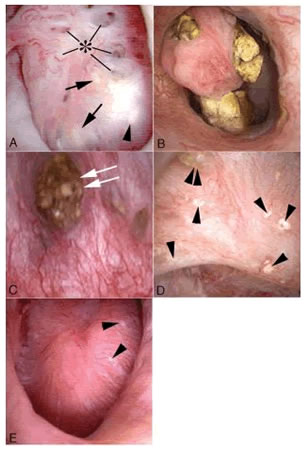
Use of this content is subject to our disclaimer