Approach
The diagnosis of trachoma will differ depending on the geographical area. Trachoma almost exclusively occurs in resource-poor settings, where expensive tests are not available.
Presence of risk factors
Risk factors for trachoma at any stage of the disease include:[1][9][10][11][12][14][16][17][18][19]
Children (aged 1 to 9 years)
Poor facial hygiene
Female sex
Poverty
Poor community hygiene
Crowded households
Residence in, or emigration from, an area where trachoma is endemic
Eye-seeking flies
Active trachoma occurs predominantly in children.
Assessment in a typical setting where trachoma is endemic
In areas with poor resources, the diagnosis of trachoma is generally made in an asymptomatic individual as part of a screening programme. People who live in or come from trachoma-endemic areas should be examined for trachoma as part of routine health examination.
Diagnosis is generally based on clinical grading using the Simplified WHO grading system, with the aid of a good light source and a loupe with adequate magnification:[30][31]
Trachomatous inflammation, follicular (TF): 5 or more follicles greater than 0.5 mm on the upper tarsal (eyelid) conjunctiva. [Figure caption and citation for the preceding image starts]: Eyelid eversion demonstrating follicles on the upper tarsal conjunctivaFrom the collection of Dr Hugh R. Taylor [Citation ends].
 [Figure caption and citation for the preceding image starts]: A normal eyelidFrom the collection of Dr Hugh R. Taylor [Citation ends].
[Figure caption and citation for the preceding image starts]: A normal eyelidFrom the collection of Dr Hugh R. Taylor [Citation ends].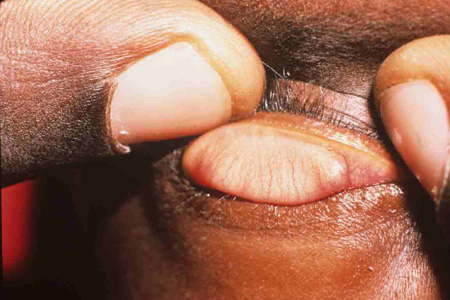
Trachomatous inflammation, intense (TI): papillary hypertrophy and inflammatory thickening of the upper tarsal conjunctiva obscuring more than half of the deep tarsal vessels. [Figure caption and citation for the preceding image starts]: Eyelid eversion demonstrating intense inflammation of the upper tarsal conjunctivaFrom the collection of Dr Hugh R. Taylor [Citation ends].

Trachomatous conjunctival scarring (TS): the presence of scarring on the tarsal conjunctiva. [Figure caption and citation for the preceding image starts]: Eyelid eversion demonstrating scars on the tarsal conjunctivaFrom the collection of Dr Hugh R. Taylor [Citation ends].

Trachomatous trichiasis (TT): at least one eyelash from the upper eyelid touching the globe, or evidence of recent epilation of inturned eyelashes from the upper eyelid.[Figure caption and citation for the preceding image starts]: A red eye due to at least 1 inturned eyelash touching the globe (trachomatous trichiasis)From the collection of Dr Hugh R. Taylor [Citation ends].

Corneal opacity (CO): corneal opacity blurring part of the pupil margin. [Figure caption and citation for the preceding image starts]: Corneal opacity due to trachomaFrom the collection of Dr Hugh R. Taylor [Citation ends].

During examination, the upper lid is everted and examined with the aid of 2.5 times loupes and a good light source. Each component of the grading system is individually marked as present or absent. The diagnosis of an individual with trachoma should trigger a community-wide assessment of the prevalence of trachoma, which may indicate the need for a public health intervention.
A diagnosis of trachoma should be considered in an individual who has been living in, or has emigrated or is visiting from, a trachoma-endemic region. Australia is the only developed country that still has endemic trachoma, where it is confined to remote Aboriginal and Torres Strait Islander communities.[2] Trachoma does not occur in developed cities.
History and examination findings
Children with active disease may be asymptomatic or present with foreign body sensation, ocular discharge, or a red eye. Adults may present with a painful watery eye, but are often asymptomatic. Signs of active infection include:
Subtarsal follicles
Limbal follicles
Subtarsal inflammation
Pannus (vessels growing over the clear cornea, generally from the superior aspect).
Recurrent episodes of inflammation will lead to the development of scar tissue on the superior tarsal conjunctiva. Examination may reveal subtarsal scarring, possibly with a superior transverse condensation called an Arlt line; however, this is not always visible.[Figure caption and citation for the preceding image starts]: Eyelid eversion demonstrating scars on the tarsal conjunctivaFrom the collection of Dr Hugh R. Taylor [Citation ends].
Pannus is common and Herbert's pits (small pits around the margin of the cornea), the result of limbal follicles, are pathognomonic for trachoma. Trichiasis and corneal opacity should be looked for in patients.
Eventually scarring will become sufficient to alter the architecture of the eyelid, rolling the lid margin inwards and causing one or more lashes to abrade the cornea. Trichiasis is painful and can cause symptoms of epiphora (watering eye) or dry eye. Adults with scarring must be followed up regularly to assess for the development of trichiasis. The consistent trauma of lash on cornea leads to corneal scarring. Late presentation may be with corneal opacities or vision loss. Blindness due to trachoma is almost always irreversible as patients are not good candidates for corneal transplant. Adults with trichiasis must be immediately referred to an ophthalmologist (or trained eye health worker) for consideration of corrective lid surgery to prevent vision loss.
Polymerase chain reaction (conjunctival swab)
The diagnosis can be confirmed with nucleic acid amplification tests such as polymerase chain reaction (PCR).
PCR may be used to determine population prevalence, particularly in hyper-endemic regions, and the effect of public health interventions. Cost and availability may inhibit the routine use of laboratory tests in trachoma-surveillance programmes in resource-poor settings.
Microbiological tests such as Giemsa stain, direct fluorescent antibody testing, and culture are no longer routinely used.[32]
Novel molecular and serological tests
Include point of care lateral flow testing for chlamydial lipopolysaccharide (optimised for use with conjunctival swabs); a rapid diagnostic device that amplifies DNA from the chromosomal porB gene of Chlamydia trachomatis; and immunoassays to measure antibodies to the C trachomatis Pgp3 antigen.[33][34][35]
Community survey in resource-poor settings
A community survey should be conducted in an area known or suspected to have endemic trachoma, or in response to the discovery of trachoma in an individual within a community suspected of having endemic trachoma.
Assessment in a resource-rich setting
The clinical signs and symptoms will be largely the same as those in a resource-poor setting. A history of having lived in a trachoma-endemic area should be present. PCR should be ordered; however, this is unlikely to be positive in cicatricial disease.
Use of this content is subject to our disclaimer