Aetiology
The majority of sporotrichosis cases are caused by the Sporothrix schenckiicomplex, which encompasses a group of dimorphic fungi, including S schenckii sensu stricto, S pallida, S globosa, S mexicana and S brasiliensis. It is found abundantly in soil, wood, sphagnum moss, thorns, decaying vegetation, and hay.[1][2] Animals (zoonotic: cats, armadillos, dogs, rodents, insects) can also be the source of the infectious organism. In the environment, at temperatures of 25°C to 30°C (77°F to 86°F), S schenckii is a dematiaceous mould with dark or hyaline conidia arranged along delicate hyphal structures in a bouquet-like appearance. In vivo in patient tissues, at temperatures of 37°C (98.6°F), S schenckii exists in a 3- to 5-micrometre cigar- or oval-shaped yeast form.
S luriei, S cyanescens, and S globosa have been reported to cause only a small minority of sporotrichosis cases.[2][16] S brasiliensis is notable for being the only Sporothrix species with an animal reservoir (cats), rather than a reservoir in plants and for its ability to be transmitted from animal to animal. Thousands of cases in cats and humans have occurred in Brazil, beginning in the southeastern part of the country.[17] DNA sequencing is required to distinguish S. brasiliensis from other Sporothrix species.[Figure caption and citation for the preceding image starts]: Mould form of Sporothrix schenckii exhibiting conidia arranged in a characteristic 'bouquet-like' appearance along delicate hyphal structures, typically found in the environment at 25°C to 30°C (77°F to 86°F)From the collection of Dr Mihalis Lionakis and Dr John E. Bennett [Citation ends]. [Figure caption and citation for the preceding image starts]: Cigar- and oval-like yeast form of Sporothrix schenckii typically found in vivo in patient tissues at 37°C (98.6°F)From the collection of Dr Mihalis Lionakis and Dr John E. Bennett [Citation ends].
[Figure caption and citation for the preceding image starts]: Cigar- and oval-like yeast form of Sporothrix schenckii typically found in vivo in patient tissues at 37°C (98.6°F)From the collection of Dr Mihalis Lionakis and Dr John E. Bennett [Citation ends].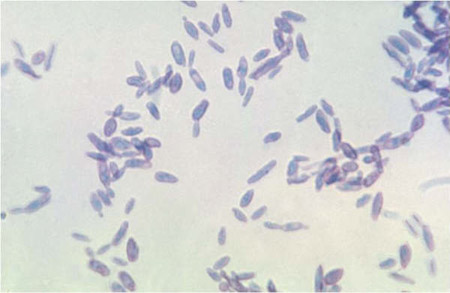
Pathophysiology
Sporothrix schenckii has virulent factors such as melanin (for free radical scavenging), extracellular proteases (for tissue invasion), and the ability to multiply at high temperatures of 37°C (98.6°F) (thermotolerance).[13] Some S schenckii strains do not grow at temperatures higher than 35°C (95°F). Such thermo-intolerant strains appear unable to cause lymphatic and visceral involvement and thus have been found only in patients with fixed cutaneous sporotrichosis, but not in those with lymphocutaneous or extracutaneous disease.[18]
Neutrophils, monocytes/macrophages, dendritic cells, mast cells, and keratinocytes appear to play a role in mounting anti-Sporothrix immune responses; TLR-2- and TLR-4-mediated signalling appears important in keratinocytes and macrophages.[19][20][21][22] Furthermore, CD4+ T-cell-mediated immune responses are important in limiting the extent of the infection as patients with more advanced HIV typically develop more severe and extensive lymphocutaneous and extracutaneous disease.[1][23] The role of CD4+ T lymphocytes in host defense against sporotrichosis is also illustrated by the granuloma formation in sporotrichosis lesions that contain interferon-gamma-producing T-helper cell 1 (TH1) lymphocytes.[24] To that end, because of the granulomatous nature of the immune response, sporotrichosis cases have occasionally been misdiagnosed as sarcoidosis.[25] On the other hand, humoral immunity does not seem to confer protection against sporotrichosis.
Most human infections arise when S schenckii is traumatically inoculated into the skin. On rare occasions, Sporothrix conidia can be aerosolised from the soil or decaying vegetation and inhaled causing isolated pulmonary sporotrichosis. The fungus may also disseminate haematogenously and cause isolated meningeal or osteoarticular disease (the osteoarticular disease may also develop secondary to contiguous spread from overlying lymphocutaneous infection) in normal hosts or extensive disseminated infection in immunocompromised individuals.[1][2]
Classification
Site of infection/clinical manifestation[1][2][3]
Cutaneous sporotrichosis
Lymphocutaneous sporotrichosis
Fixed (plaque) cutaneous sporotrichosis.
Extracutaneous sporotrichosis
Osteoarticular sporotrichosis
Pulmonary sporotrichosis
Meningeal sporotrichosis
Disseminated sporotrichosis
Other less-common presentations (e.g., laryngeal, ocular).
Use of this content is subject to our disclaimer