Aetiology
Oestrogen stimulates breast duct development in both men and women in the presence of permissive levels of growth hormone, follicle-stimulating hormone (FSH), and luteinising hormone (LH) from the pituitary. Progesterone stimulates development of breast alveoli. Androgens oppose oestrogen action. Prolactin is not a growth factor for the breast in men, but high prolactin levels suppress the hypothalamic generator of gonadotropin-releasing hormone (GnRH) pulses that stimulate production of LH and FSH. Gynaecomastia results from a relative excess of oestrogen or oestrogen action or a relative deficiency of androgen or androgen action.[Figure caption and citation for the preceding image starts]: Hormones involved in male breast developmentFrom the collection of Catherine B. Niewoehner, MD [Citation ends].
In men, 95% of testosterone is produced in the Leydig cells of the testes in response to LH. The remaining 5% of testosterone and the weak androgen androstenedione are produced by the adrenal glands. Testosterone can be converted to the more potent androgen dihydrotestosterone by the enzyme 5-alpha reductase. Testosterone is converted to oestrogen by the enzyme aromatase, which also converts androstenedione to the weak oestrogen oestrone. Aromatase is found predominantly in adipose tissue. In the blood, 50% to 60% of testosterone is tightly bound to sex hormone binding globulin.[17] Most of the rest is weakly bound to albumin and is considered bio-available. Only the small free testosterone fraction (0.5% to 3%) is active. Free testosterone declines slowly with age.[18][19] Oestrogen is less strongly bound to sex hormone binding globulin than testosterone. Defects in any of these pathways can cause gynaecomastia.[20][21]
Approximately 10% to 20% of gynaecomastia is believed to be attributable to prescribed drugs; many medicines have been implicated, but the quality of the evidence is often very poor.[22][23][24][25]
Causes of elevated oestrogen levels or activity:
Excess aromatase activity: obesity, congenital activating mutation of aromatase, tumours (Sertoli cell, Leydig cell, germ cell)[26]
Excess androgen converted to oestrogen: testicular feminisation, anabolic steroid use, excessive androgen replacement therapy, cirrhosis
Differences in sex development: co-existing functional ovarian and testicular tissue (along with oestrogen production from ovarian tissue)
Chronic illness or starvation and re-feeding: more profound suppression of testosterone than oestrogen with fasting, and earlier increase in oestrogen than testosterone with re-feeding
Oestrogen-producing tumours: Sertoli cell, Leydig cell, germ cell, human chorionic gonadotrophin (hCG)-producing tumours (stimulate Leydig cell oestrogen production), feminising adrenal adenoma and carcinoma[27]
Exogenous oestrogen exposure
Drugs that stimulate oestrogen receptors: diethylstilbestrol, digitalis, phenytoin
Hyperthyroidism.
Causes of testosterone deficiency:
Hypothalamic: hypogonadotrophic hypogonadism (Kallmann syndrome, the failure of GnRH-producing neurons)
Hyper-prolactinaemic: pituitary tumour, hypothyroidism, renal disease (GnRH pulse generator suppression)
Normo-prolactinaemic pituitary disease or tumour (decrease in gonadotrophin production)
Differences in sex development: co-existing functional ovarian and testicular tissue (along with oestrogen production from ovarian tissue), Klinefelter syndrome (47XXY)
Testicular: castration, infection (e.g., orchitis), infiltration (e.g., haemochromatosis), chemotherapy- or radiation-related damage to Leydig cells, neurological diseases (spinal cord injury, myotonic dystrophy)
Medications: gonadotropin-releasing hormone (GnRH) agonists, cancer chemotherapeutic agents, ketoconazole, metronidazole, spironolactone, some antipsychotic agents.
Causes of impaired testosterone action:
Ageing
Elevated oestrogen levels
Genetic factors
Medications: anticonvulsants, androgen receptor blockers (bicalutamide, flutamide), spironolactone, 5-alpha reductase inhibitors, H2 antagonists (e.g., cimetidine), proton-pump inhibitors (impair testosterone action less than H2 antagonists).[28][29][30][31]
Pathophysiology
Oestrogen excess or increased oestrogen sensitivity stimulates proliferation of breast ducts and ductal epithelium. If androgen deficiency or androgen inhibition is present, the effect of oestrogen is more pronounced, even if the oestrogen level is normal. At puberty, marked increases in growth hormone, insulin-like growth factor 1, follicle-stimulating hormone, and luteinising hormone drive both oestrogen and testosterone production, but the oestrogen peak precedes the peak in testosterone production. There are many contributors to increased oestrogen versus androgen effect in adults. Regardless of cause, the initial phase with proliferating ducts, ductal epithelium, stroma, and fibroblasts, accompanied by inflammation and oedema, often gives way to a more quiescent stage characterised by dilated ducts, stroma, and fibrosis with little inflammation. The fibrotic stage is far less likely to regress either spontaneously or with treatment. Progesterone levels in men are low, so there is little alveolar tissue in the male breast even when gynaecomastia is present. Hence, galactorrhoea is rare.[Figure caption and citation for the preceding image starts]: Histology: normal male breast; rare, isolated ducts; no lobules; 10X magnificationFrom Minneapolis Veterans Affairs Medical Center pathology collection [Citation ends].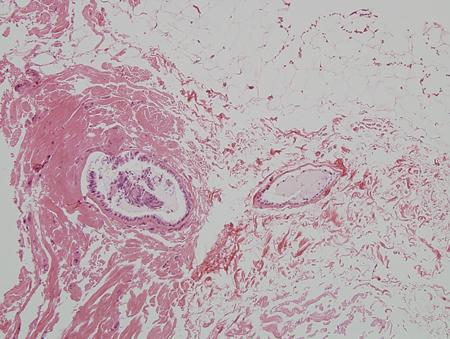 [Figure caption and citation for the preceding image starts]: Histology: gynaecomastia; clusters of ducts, halos of oedema, fibrous background; 5X magnificationFrom the collection of Catherine B. Niewoehner, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Histology: gynaecomastia; clusters of ducts, halos of oedema, fibrous background; 5X magnificationFrom the collection of Catherine B. Niewoehner, MD [Citation ends].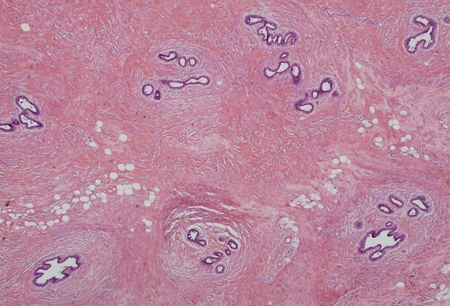 [Figure caption and citation for the preceding image starts]: Histology: normal female breast; many ducts; prominent lobules; 10X magnificationFrom Minneapolis Veterans Affairs Medical Center pathology collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Histology: normal female breast; many ducts; prominent lobules; 10X magnificationFrom Minneapolis Veterans Affairs Medical Center pathology collection [Citation ends].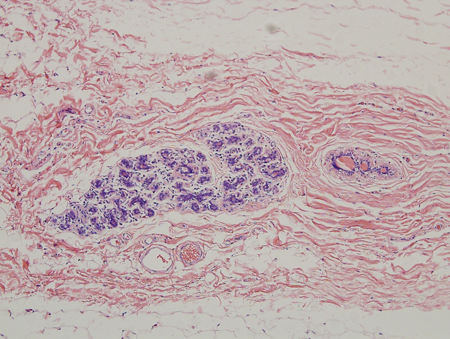
Classification
Clinical categories[1]
There is no formal classification scheme. However, there are clinically accepted categories.
Newborn gynaecomastia:
A physiological response to high levels of maternal and placental oestrogen transferred in utero. Neonatal milk secretion can often occur.
Pubertal gynaecomastia:
A physiological response to the 30-fold increase in testosterone fuelled by marked increases in growth hormone, insulin-like growth factor-1, follicle-stimulating hormone, and luteinising hormone at puberty
Oestrogen increases 3-fold, but peaks earlier than testosterone.
Adult gynaecomastia (physiological):
A physiological response to the decrease in free testosterone and the increase in adipose tissue that often accompanies ageing
Testosterone is converted to oestrogen in adipose tissue.
Adult gynaecomastia (non-physiological):
A response to increased oestrogen effect relative to androgen effect from a cause other than ageing.
Pseudo-gynaecomastia:
Male breast enlargement entirely due to adipose tissue.
Simon classification[2]
Based on the amount of tissue to be removed in cases of surgery:
Class I: minor breast enlargement with no skin redundancy
Class IIa: moderate breast enlargement with no skin redundancy
Class IIb: moderate breast enlargement with minor skin redundancy
Class III: marked breast enlargement with major skin redundancy (resembles the female breast).
Use of this content is subject to our disclaimer